Introduction
Spontaneous pneumomediastinum (SPM) is a rare entity in pediatric age, with multifactorial etiology. The triad of chest pain, dyspnea, and subcutaneous emphysema should lead to clinical suspicion. Chest X-ray is the diagnostic exam of choice. Treatment should be conservative, and most patients recover without sequelae.1,2
Case report
Herein is reported the case of a 16-year-old male adolescent, with a history of multiple allergies (mites, dogs, cats, and grasses) and marked smoking habits since the age of 13 (one pack/day for one year). The boy was admitted to the Emergency Department of the local hospital with dry cough, dyspnea, chest pain with pleuritic characteristics worsened in dorsal decubitus and relieved in sitting position, and fever with 12 hours of evolution. When questioned, the he referred daily cannabis use, cocaine inhalation, and sporadic amphetamine intake.
Physical examination revealed a tall, distressed young man with dyspnea, polypnea, chest tightness, and hypoxemia with 90% peripheral oxygen saturation. Crepitus was present in the cervical region and right hemithorax on palpation. Pulmonary sounds presented decreased vesicular murmur with wheezing.
Chest X-ray was performed, evidencing para-cardiac mediastinal hyper transparency bypassing the aortic knob, a discrete air blade involving the cardiac silhouette, and subcutaneous emphysema in the right supraclavicular region (Figure I). Electrocardiogram showed no pathological changes. Urine analyses were positive for tetrahydrocannabinoids.
The patient was admitted for clinical surveillance, with cardiorespiratory monitoring and symptomatic treatment (rest, analgesia, and oxygen supply with air-entrainment mask).
Mycoplasma pneumoniae serology revealed IgM of 33U/mL and IgG of 25U/mL. Allergy study was also performed, showing marked sensitization to mites, serum IgE levels of 4,422 KU/L, and IgE for Dermatophagoides pteronyssinus and Dermatophagoides farinae higher than 100 KUA/L.
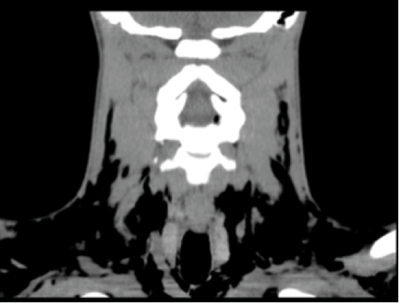
To assess the extent of disseminated air and rule out underlying pulmonary pathology, computed tomography (CT) scan was performed, revealing extensive subcutaneous emphysema covering the cervical region, dissecting the different anterior and posterior cervical spaces as well as peri and retropharyngeal and interthoracic regions. Air dissected the different mediastinal spaces, with emphysema also surrounding some regions of the gutter muscles and vertebral canal. Emphysema of the chest wall was also identified (Figures IIandIII).
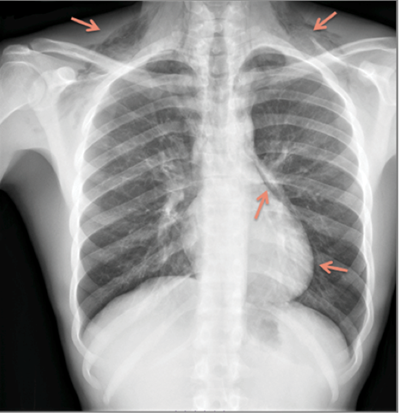
Figure I Chest radiography revealing linear streaks of lucencies, representing free air in the mediastinum and neck soft tissue
The patient was hospitalized during four days, with no major complications. On discharge, thoracic X ray was repeated, showing a decrease in cervical subcutaneous emphysema and partial pneumomediastinum resorption. The patient was discharged home, with smoking cessation recommendation. He was evaluated one week after discharge in cardiothoracic surgery consultation, with complete pneumomediastinum resolution. One month after discharge, the patient showed a reduction in tobacco and illicit drug consumption. He currently maintains follow-up in outpatient adolescent, pedopsychiatry, and pulmonology consultations. Environmental measures to prevent allergens (mites) were reinforced.
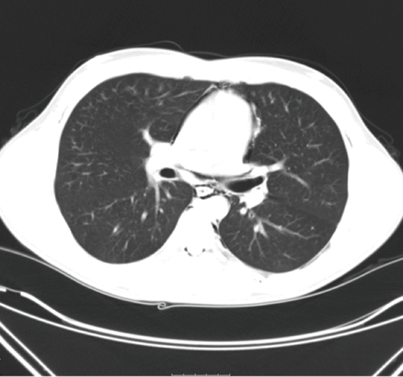
Figure II Chest CT scan showing air around the mediastinal structures, compatible with pneumomediastinum
Conclusion
SPM should always be considered in the differential diagnosis of boys with chest pain, especially of l slender biotype.3,4 It is a disease with multifactorial etiology and chest radiography is usually enough to establish diagnosis.5 It is an uncommon pathology, sometimes associated with unexpected clinical presentation, requiring a high index of suspicion.4-6 SPM is usually a benign and self-limiting condition and prognosis is related to the underlying disorder.7
Several pneumomediastinum triggering and predisposing factors can be identified in this case report, such as marked smoking habits, acute mycoplasma infection, and inhaled and smoked drug consumption. No previous asthma history was reported, only a history of multiple allergies, with subsequent positive atopy study. In Pediatrics, the most common predisposing diagnosis is asthma, followed by respiratory infections and vomiting. Other precipitants include drug inhalation (commonly cocaine, marijuana, or ecstasy).7
In the present case, history suggestive of upper respiratory infections associated with identification of IgM for Mycoplasma pneumoniae led to the hypothesis that acute infection by this agent triggered violent enough coughing to elicit pressure changes leading to air leakage. In absence of a gold standard exam, diagnosis of Mycoplasma pneumoniae infection is performed through non-culture tests, as serology and molecular biology tests. Although not performed, direct Mycoplasma pneumoniae detection in nasopharyngeal secretions (sputum/bronchial lavage) by high-sensitivity and high-specificity polymerase chain reaction is possible, but an expensive resource.5
While investigating the etiology of spontaneous mediastinum, particularly in young and healthy patients, drug abuse should always be considered to provide proper psychiatric and social guidance.