Introduction
Delirium is a common neurobehavioral syndrome considered to be caused by a dysregulation of baseline neuronal activity secondary to systemic disturbances.1 In the hospital setting, delirium is a risk factor for clinical complications, a longer length of stay and discharge to a post-acute nursing facility.2 Even with respect to long-term outcomes there is evidence that delirium episodes are associated with poorer outcome, independently of confounders such as age, sex, comorbid illness or illness severity, and baseline dementia.3 It is well recognized that the first step in delirium management, in any hospital setting, is to perform a timely and accurate diagnosis, preferably via the use of a brief (validated) instrument that assesses features in the Confusion Assessment Method algorithm.2,4The systematic assessment of delirium may, nevertheless, be rendered difficult in the Emergency Department (ED) due to the intrinsic characteristics of the setting: acute patients and time constraints. Thus, for the ED, the few studies available indicate that health care providers may miss delirium up to approximately 75% of the time,5-7which may hinder a translation into appropriate (early) treatment measures of delirium.5,6
For the ED environment, a total of 7 different scales have been identified for delirium screening.5 Of these, The Confu-sion Assessment Method for Intensive Care Unit (CAM-ICU) is the most widely used.5,6Overall, the CAM-ICU has shown a good profile of specificity and sensitivity, having been validated across different hospital settings.8-13Concerning the ED setting there are few studies; however, Han et al (2014) validated the CAM-ICU in the ED in a cohort of 406 older (>65 years) patients. The study indicated a CAM-ICU sensitivity of 72.0% (95% confidence interval [CI] = 58.3% to 82.5%) and 68.0% (95% CI = 54.2% to 79.2%) in the emergency physician and in the research assistants’ application of the scale, respectively, and a specificity of 98.6% (95% CI = 96.8% to 99.4%) for both raters.7 In Europe, so far, the only study that directly addressed the process of validation of the CAM-ICU for delirium in the ED setting, from Van de Meeberg et al, reported a sensitivity of 100%, a specificity was 98%, and a positive predictive value of 92%, and negative predictive value was 100%.14In another study from Holland, Lucke et al applied the CAM-ICU in a large cohort of ED patients, and founded a low prevalence of delirium, suggesting a low performance. However, it was not a study of the validation of the CAM-ICU in the ED.15
To our knowledge, no other groups have addressed the performance of the CAM-ICU in the ED, particularly outside the United States. In fact, a recent review indicates that the validation data of the CAM developed specifically for the ED setting is limited.16 Thus, despite the relevant work on the application of the CAM-ICU in critically ill, intensive care unit and older patients,7,8,11-13uncertainty about its diagnostic accuracy and reliability remains,7 with an identified need for continued assessment across ED settings and in large(r) cohorts.5Here, in the ED of a main hospital referral centre, across its emergency units (allocation to these specialized units is based on patients' screening and severity), the aim was two-fold: (i) to compare the results of the CAM-ICU on the identification of delirium versus the ‘gold standard’ DSM-5, and (ii) to address for the applicability of the CAM-ICU European Portuguese version, as applied by researchers (senior medical students) and medical professionals (emergency internists), trained for its application, “in lieu” of the DSM-5.
Methods
CHARACTERIZATION OF THE EMERGENCY DEPARTMENT
The study was conducted at the ED of Hospital de Braga (Braga, Portugal), a University of Minho (Braga, Portugal) affiliated hospital with 705-beds, which serves a population of 1 200 000 as a tertiary referral centre. The ED at the Hospital de Braga has an annual census of approximately 175 000 visits, and it comprises two ED clinical decision units, the EDCDU1 and the EDCDU2, an ED physician office (EDPHOF) and an ED intermediate care unit (EDIMCU). These units are rooms properly organized with priority hierarchies based on patients' screening and severity. All the units are physically connected to the ED, sharing medical and nursing staff.
For the ED patients (all age ranges), the EDCDUs provide an alternative to discharge or hospital inpatient admission; patients may benefit from an extended observation period, generally less than 24 hours. Patients screened on admission with the Yellow or the Orange criteria of the Manchester triage,17 or who need to stay in the supine position in a stretcher, are referred to the EDCDU1 and the EDCDU2, respectively. The EDPHOF unit attends to problems related to patients’ health with low severity degree; where, any patient screened to the EDPHOF may be forwarded to other ED units in case of worsening health status and if this referral is justified. The EDIMCU is a 9-bed unit that receives patients from multiple intra- and inter-hospital origins, including from the ED, surgical and medical wards (as a step-up unit), ICU (as a step-down unit), recovery operatory room, and other hospitals (without intermediate and/or intensive care units). The criteria for admission to the EDIMCU follows the Guidelines on Admission and Discharge for Adult Intermediate Care Units of the Society of the Critical Medicine.18
STUDY POPULATION AND DESIGN
In order to obtain an approximate sample to the reality of the ED at Hospital de Braga, across time, data were randomly and prospectively recorded, in a convenience sample, across 3 separate collection periods (June 2014 to Novem-ber 2014; July 2015; and, April 2016 to July 2016), across the ED units (EDCDU1 and 2, EDIMCU and EDPHOF). Winter season (December to March) was not considered due to the ED overcrowding (mainly respiratory illnesses in older adults and chronic patients), and the potential overextension of the ED waiting period, or length of stay, that can characterize the Department in that time of year [a phenomenon termed “exit block” (or access block).19
The study inclusion criteria included patients aged 18 years or older, admitted to the ED, whenever members of the study research team were present. Patients were excluded if: (i) obstetric and pediatric population; (ii) ambulatory patients in their full range of movements and autonomous who refer directly to the ED; or, (iii) unviable to assess for delirium using the CAM-ICU20 at any time during the initial screening procedure, including clinical evaluation refusal by the patient, inability to follow simple commands before acute illness onset, language communication barriers, advanced dementia previously diagnosed, or other diagnosed neuropsychiatric disorder, and coma. The exclusion criteria used are in accordance with previous similar studies.8,21Patients who had been evaluated using the CAM-ICU in prior ED admissions, or that were evaluated outside the formal study periods of assessment for the purpose of this work, were also excluded due to impossibility to control any methodological or selection bias. The sample size estimated to determine de validity of the CAM-ICU was based on the subject to item ratio. A subject to item of 10 was fixed as the minimum, which makes it necessary to have a minimum sample of 70 patients enrolled considering 7 items associated with CAM-ICU: Feature 1, Feature 2, Feature 3, Feature 4 (which contains 4 questions to evaluate the disorganized thinking).22
Before the start of data collection, all researchers (senior medical students) and medical professionals (emergency internists), who participated in delirium assessment using the CAM-ICU, underwent a training period coordinated by two staff members as part of the hospital Quality Assurance Program. Training materials were provided by Vanderbilt University including training manuals, didactic lectures, demonstrations and direct practice of the assessment tools in patient scenarios.20
The Ethical Committee at Hospital de Braga approved the study protocol and waived informed consent. The study was non-interventional; therapies with regard to the clinical diagnosis, delirium and sedation state were left to the discretion of the attending physician.
MEASUREMENTS
Delirium status was assessed using CAM-ICU20 following the same methodology reported by Han et al7,23and Mariz et al.21The CAM-ICU takes less than 2 minutes to complete and reports on: i) acute onset of mental status changes or a fluctuating course, ii) inattention, iii) disorganized thinking, and iv) altered level of consciousness.8,20The Richmond Agitation and Sedation Scale (RASS) was used to categorize the psychomotor subtype of delirium (RASS score between: +1 and +4, hyperactive delirium; 0 and -3, hypoactive delirium).20,24Depending on resident psychiatrists’ availability, within a 3-hour time period of the CAM-ICU assessment by the researcher/medical professional, and if the patient had not yet been discharged from the ED, delirium was assessed by the resident psychiatrist using the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as the gold standard for delirium status diagnosis.4 This involved an inclusive interpretation of Criteria A and D, as indicated by the European Delirium Association and the American Delirium Association.25 The psychiatrists involved in the study have a permanent presence at ED, sharing the patients’ management in the same setting as the physicians in the frontline of the ED, but were blind to the CAM-ICU result. Patients were assessed no more than once by each method and, if evaluated by both metho-ds, these were conducted within a 3-hour timeframe.
Patient data included: age, gender, admission type (emer-gency department, operating room, wards, intensive care unit, inter-hospital transfer), location in the ED, and diagnostic groups (cardiovascular, drug toxicity/ withdrawal, gastrointestinal, genitourinary, neurologic, haemato-oncologic, pulmonary, trauma/ musculoskeletal and other). The systemic inflammatory response syndrome (SIRS) criteria (two or more of the following criteria: heart rate > 90 beats/min; body temperature < 36 or > 38°C; respiratory rate > 20 breaths/min; white blood cell count < 4x109 or > 12x109 cells/L [23]) was used as a surrogate for severity of illness. Data were col-lected from the Clinical Process through the Glintt® computer system which only the researcher responsible for the project had access.
STATISTICAL ANALYSIS
All statistical analyses were conducted using SPSS statistics version 23.0. Measures of central tendency and dispersion for continuous variables were reported as medians and standard deviation (SD). Categorical variables were reported as absolute numbers and proportions. Criterion validity was determined by comparing the CAM-ICU raters to the delirium expert rating by using the DSM-5 criterion as the reference standard. To determine validity a 2 x 2 table was created comparing the reference standard ratings with the CAM-ICU ratings included the number of true positives (TP), false positives (FP), false negatives (FN), and true negatives (TN). Sensitivity= TP/(TP+FN); specificity=TN/(FP+TN); accuracy=(TP+TN)/(TP+FP+FN+TN); likelihood ratio= sensitivity/(1-specificity); positive predictive value (PPV) and negative predictive value (NPV). Ninety-five percent confidence intervals (CI) for these test characteristics were calculated by using “VassarStats: Website for Statistical Computation” (http://vassarstats.net). Exact chi-square testes and ANOVA analysis were performed as appropriate to deter-mine if baseline features differed between ‘Delirium’ and ‘No Delirium’ groups. Prevalence of delirium in the ED of Hospi-tal de Braga was determined. Agreement between CAM-ICU/DSM-5 diagnosis of delirium was calculated with the kappa statistic and the McNemar’s test.
Results
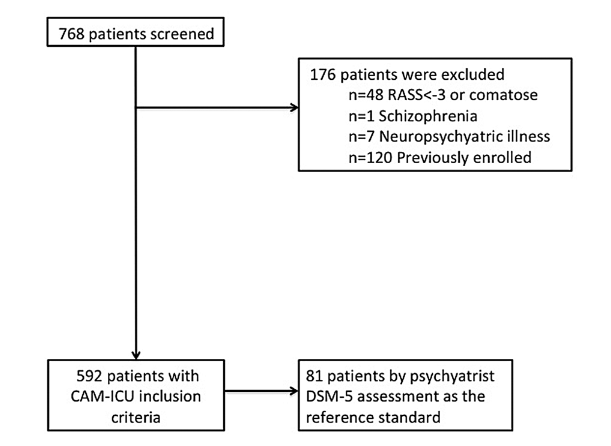
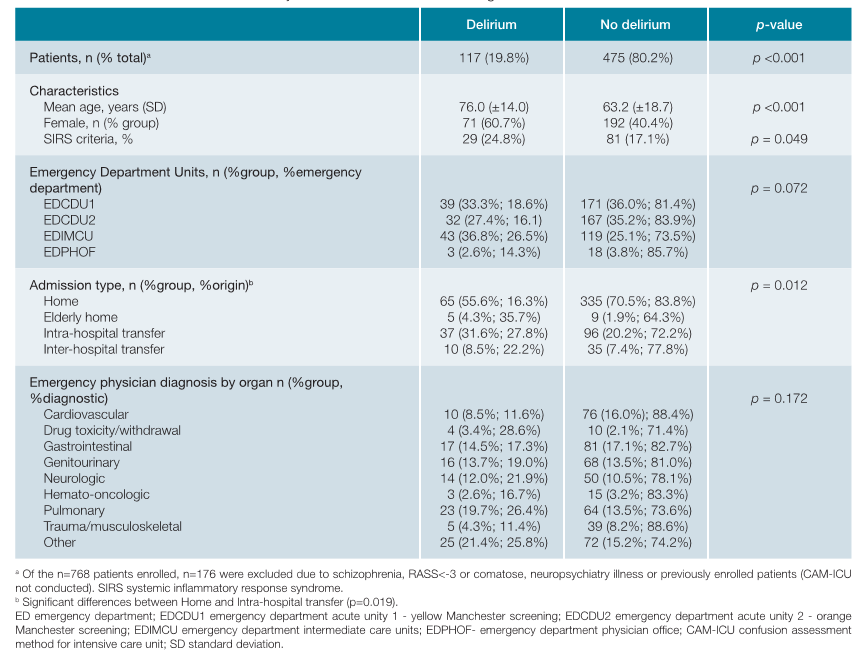
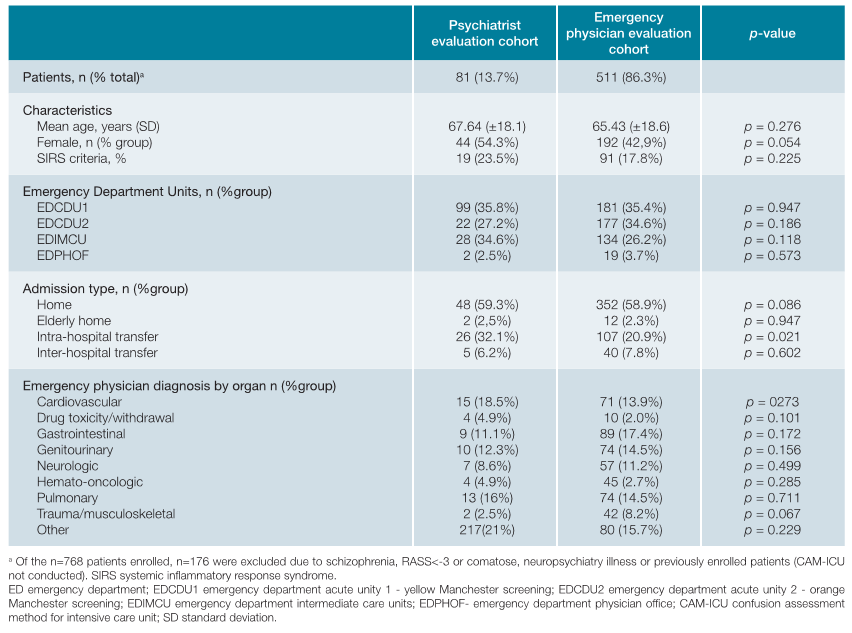
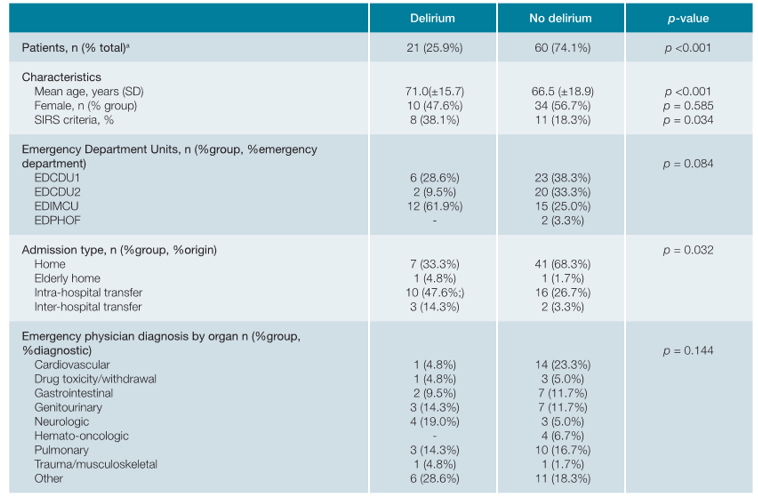
A total of 768 patients were screened in the time periods referred; of these, all 592 patients that met the inclusion criteria (study sample) were evaluated using the CAM-ICU and, of these, 81 (13.7%) were further evaluated by the resident psychiatrist on duty (blind to the CAM-ICU result) following the DSM-5 criteria (Fig. 1). Baseline characteristics of the study cohort are presented in Table 1. The median age of the study sample was 65.74 years old (± 18.68), 61.3% (n = 363) were aged 65 years or more, and 263 (44.4%) were female. The distribution of patients by emergency units was: 35.5% (n = 210) EDCDU1, 33.6% (n = 199) EDCDU2, 27.4% (n = 162) EDIMCU and 3.5% (n = 21) EDPHOF. Characteristics of the CAM-ICU evaluation cohort by the ED physicians versus the psychiatric evaluation cohort are presented in Table 2. There were no significant differences between the psychiatric evaluation and the ED physician’s evaluation, besides more patients from intra-hospital transfer in the former (32.1% vs 20.9%; p = 0.021).
Using the CAM-ICU, delirium was observed in 17.6% (90/511) (ED physician evaluation); while, using the standard evaluation technique DSM-5, 25.9% (21/81) delirium cases were diagnosed (psychiatric evaluation). Characteristics of the ‘Delirium’ patients are presented in Table 3; these were significantly older compared to ‘No Delirium’ (mean 71.0 vs 66.5, p <0.001) and presented higher percentage confor-ming to the SIRS criteria (38.1% vs 18.3%, p = 0.034). Most patients were alert and calm at evaluation time (RASS = 0; 68.1% via CAM-ICU, 70.4% via DSM-5); most of those assessed with delirium were hypoactive (79.5% via CAM-ICU; 71.4% via DSM-5). One false negative was observed; at the moment of CAM-ICU assessment, the patient was at his mental status baseline (RASS=0) and there was no evidence of a fluctuating course of mental status.
Table 3: Patient characteristics stratified by delirium status assessed using both the CAM-ICU and the DSM-5 by psychiatrist assessment.
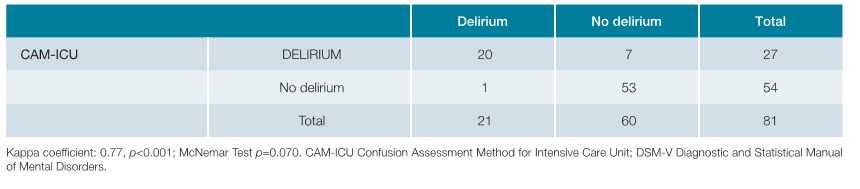
The CAM-ICU identified 20 of the 21 delirious patients identified by the DSM-5 and showed an overall sensitivity of 95.2% (95% CI= 74.1 to 99.8) and specificity of 88.3% (95% CI= 76.8 to 94.8). The negative likelihood ratio (LR-) was 0.05 (95% CI= 0.01 to 0.37). The positive likelihood ratio (LR+) was 8.16 (95% CI= 4.04 to 16.48) (Tables 4 and 5).
Discussion
A psychiatric evaluation of a fluctuating case in an ED is a high constrain depending on time and immediate psychiatric staff availability, with time being of priority in delirium treatment. The present study was carried out in the ED of a central district hospital, across multiple collection points, assessing for a large cohort of patients. The study corroborates for the easy-of-use of the scale and its feasibility and practicality in the ED setting. The scale incorporates objective assessments, allowing to remove any possible subjectivity from delirium assessment and rendering it easier to use by eventually less experienced users.
The results indicate that the CAM-ICU has high levels of sensitivity (95.2%: 95% CI= 74.1 to 99.8) and specificity (88.3%: 95% CI= 76.8 to 94.8), suggesting that when the CAM-ICU is positive (in the ED setting) any relevant treatment for this condition may be initiated. A common feature of every published research work on CAM-ICU is its high specificity. The routinely use of delirium screening and diagnostics tools can increase the detection rate of cases. Ely et al (2001) carried out the first validation study of the CAM-ICU in an inten-sive care unit (ICU) in critically ill patients in a study sample of 31 patients.8 The study showed a high specificity (95% to 100%) and sensitivity (89% to 93%) and an excellent interrater correlation. The same authors published a second study enrolling 111 patients on mechanical ventilation that confirmed the high interrater correlation (kappa coefficient: 0.99, 95% CI: 0.92 - 0.99), and the high sensitivity (93% to 100%) and specificity (98% to 100%) of the scale.9 Tobar et al (2010) validated the Spanish CAM-ICU version in 29 critical patients, also undergoing mechanical ventilation, obtaining a sensitivity between 80% to 83% and a specificity of 96%.10 Flores et al, (2011) validated the CAM-ICU in a mixed population of critically ill patients in four ICUs in Brazil, enrolling a total of 119 patients, and showed an overall sensitivity of 72.5% (95% CI: 55.9% - 84.9%) and specificity of 96.2% (95% CI: 88.5% - 99%).11
Still, the present study differs in some respects from other works. Here, at 88.3%, the calculated specificity was not as high for the CAM-ICU as others have published (varying from 93% to 100%). This difference does not seem to be related to the implementation of CAM-ICU using the European Portuguese language as other authors have applied Spanish and Portuguese (Brazil) and translations of the CAM-ICU and have obtained high specificities.10,11,14The most likely explanation relates with the patient’s characteristics. Here, the study was carried out with a high spectrum of patients with different characteristics, including range in ages, emergency physician diagnosis, admission type and disease severity. In contrast, many of the previous studies were done using more homogeneous cohorts either in terms of age and less critical conditions,7 or in well-defined diagnosis groups such as medical oncology and patients with acute stroke.12,13Thus, the sensitivity and specificity differences showed in different CAM-ICU validation works may be related to the patients’ characteristics, namely age and illness severity, warranting continued work in the area. Nonetheless, it also of note that a cohort's heterogeneity may not necessarily explain relatively low specificities. The CAM-ICU's specificity may also be diminished in patients with dementia7 or, also of consideration, can also be explained by random chance. Here, the sensitivity obtained for the CAM-ICU presented a higher value than the values presented in other studies, which may be related with the (high) severity of patients in the cohort.
There are other influences to be noted, regarding ED organization and structure. In particular, our ED system is very based on Clinical Decision Units (CDU), that overall could be partially compared with the Observation Units in the US, although CDU are fully integrated in the ED. More so, our ED is an open system, absorbing a very substantial proportion of non-urgent situations, which for a multitude of reasons are not managed in the primary care system. It is estimated that approximately 25% of the attendees at hospital emergency units do not need immediate care.26 This number can be higher in central district hospitals. Accordingly, at the ED of Hospital de Braga, following the Manchester Triage System classification, an average of 35% of patients were green coded in 2017 (internal hospital data, unpublished), mainly in the EDPHOF. For that reason, we chose not to include patients from the EDPHOF, as these patients are mainly low priority, non-urgent patients, who should have been attended in their GPs.
LIMITATIONS
The study has limitations that are of note. Throughout the data collection time periods different researchers/medical professionals applied the CAM-ICU. Albeit all receiving the same procedural training this may potentially have influenced results. Nonetheless, the tool is simple and easily applied, and several studies have indicated for an excellent interrater correlation in the application of the CAM-ICU. In this regard, another possible limitation was that only research personnel and clinicians administered the CAM-ICU (the scale was not applied by support staff to the ED, technical staff or nurses); which may bias possibly toward higher performances of the CAM-ICU. Still, the researchers were senior medical students, which may add value to the hypothesis that even less experienced health personal may, when properly trained, also aptly apply the tool.
Another limitation, a selection bias is of note given that a convenience sample was enrolled for the confirmatory psychiatry evaluation (those present in the ED at the time) due to the difficulty of psychiatrist’s availability by limitations of staff. Albeit the psychiatrist having no influence on the selection of patients, the difference of CAM-ICU positive patients between the group who received the psychiatrist evaluation and the group who did not (26% vs 33%, respectively) may point out that psychiatrists may have inadvertently selected patients who were more obviously delirious; that is, more true positives. This may falsely ncrease sensitivity while falsely decreasing specificity. We think the differences are merely due to chance but care in data interpretation is of note. It is also of care, particularly given the age spectrum of the delirious patients, that there is not a measu-re of the effect of dementia and severity of illness in the diagnostic performance. Importantly, all the psychiatrists involved have a strong training in ED work. Finally, the setting of the ED here addressed is very different than most EDs particularly in the US, thus any generalizations should be of great caution. As described, here the vast majority of patients were enrolled in the EDCDU and EDIMCU and may likely comprise a minority of the more conventional ED population particularly in the US setting; more so, only 3% were evaluated in the EDPHOF which could be lower than in other places. In this context, the cohort studied may be characterized by being ‘sicker’ and ‘older’ compared to other EDs, although of note that it is the delirium assessment tool currently recommended by the Geriatric Emergency Department Guidelines is the bCAM, which is a modification of the CAM-ICU to improve the CAM-ICU's sensitivity and enhance its brevity.27,28However, as we discussed above, there is still uncertanties of the performance of the different scales in differents EDs outside where they were validated. Ultimately, such differences may affect diagnostic performances and are here of final consideration.
Conclusion
The work indicates that the CAM-ICU European Portuguese is a practical instrument for the assessment of delirium in the real setting of an ED showing sensibility, specificity and accuracy for delirium diagnosis in the setting considered. The findings indicate for the accuracy of the CAM-ICU in delirium diagnosis, suggesting that is an appropriate tool to develop a delirium diagnostic profile in ED patients. Also, the CAM-ICU observed a prevalence of delirium of 19.8% in the ED, following previous works.23 It is expected that its systematic use in the ED will improve delirium detection rates and contribute to decrease the morbidity and mortality associated with clinical diagnosis of delirium, bridging the gap regarding to the subjectivity about delirium status. In the future, delirium should be systematically assessed in the ED and a protocol should be considered to follow-up and evaluation of delirious patients.