Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.21 no.1 Lisboa fev. 2014
https://doi.org/10.1016/j.jpg.2013.04.006
ARTIGO ORIGINAL
Comparative study of spot urine Na/K ratio and 24-hour urine sodium in natriuresis evaluation of cirrhotic patients with ascites
Análise comparativa da razão Na/K em amostra isolada de urina com sódio na urina de 24 horas na avaliação da natriurese de cirróticos com ascite
Otávio Marcos da Silva, Gabriela Bicca Thiele, Leonardo Fayad, César Lazzarotto, Esther Buzaglo Dantas-Corrêa, Leonardo de Lucca Schiavon, Janaína Luz Narciso-Schiavon*
Núcleo de Estudos em Gastroenterologia e Hepatologia (NEGH), Federal University of Santa Catarina (UFSC), Florianópolis, SC, Brazil
*Corresponding author
ABSTRACT
Introduction: The spot urine sodium/potassium (Na/Ku) ratio is a convenient tool to identify sodium excretion < 78 mequiv./d. It has been established that this ratio is as useful and accurate as 24-h urine sodium (Nau24h), but no Latin American study has evaluated this issue. The aim of this study is to evaluate the accuracy of the Na/Ku ratio and to compare it to Nau24h.
Materials and methods: This cross-sectional study included 20 patients with decompensated liver cirrhosis and ascites.
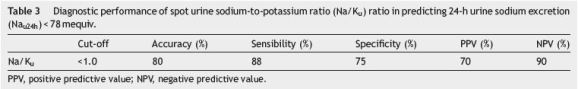
Results:Mean age was 56.1±11.8 years old, 70% were men and 60% presented Nau24h < 78 mequiv./d. Poor sodium excretion group presented higher MELD score (P = 0.002), creatinine (P = 0.029), AST (P = 0.027) and bilirubin (P = 0.013) levels, and also lower median spot sodium urine (P = 0.001). There was a high positive correlation between Na/Ku ratio and Nau24h (r = 0.857; P < 0.001) and negative correlation with MELD (r =−0.498; P = 0.025) and sérum creatinine (r =−0.498; P = 0.025). The AUROC of Na/Ku in predicting Nau24h < 78 mequiv./d was 0.948±0.046 and the classical Na/Ku ratio cut-off (≤1.0) showed PPV = 70%, NPV = 90%, accuracy = 80%, sensitivity = 88% and specificity = 75%.
Conclusion: Na/Ku ≤1 is sensitive and specific, and substantially correlates with Nau24h, which enables the use of this test in the routine evaluation of patients with liver cirrhosis decompensated in ascites.
Keywords: Liver cirrhosis; Ascites; Sodium; Urine; End stage liver disease
RESUMO
Introdução: A razão sódio/potássio em amostra isolada de urina (Na/Ku) é uma ferramenta apropriada para identificar a excreção urinária de sódio < 78mEq/d. Foi estabelecido que essa razão é tão útil e acurada quanto a dosagem de sódio na urina de 24 horas (Nau24h), contudo nenhum estudo Latino Americano avaliou essa questão. O objetivo desse estudo foi avaliar a razão Na/Ku e compará-la a dosagem de Nau24h.
Material e métodos: Estudo transversal que incluiu 20 pacientes com cirrose hepática descompensada em ascite.
Resultados: A idade média foi de 56,1 ± 11,8 anos, 70% eram homens e 60% apresentaram Nau24h < 78 mEq/d. O grupo mau excretor de sódio apresentou maior escore MELD (P = 0,002), creatinina (P = 0,029), AST (P = 0,027), bilirrubinas (P = 0,013), e também menor mediana de sódio em amostra isolada de urina (P = 0.001). Houve correlação positiva entre razão Na/Ku e Nau24h (r = 0,857; P < 0,001) e correlação negativa com MELD (r = 0,498; P = 0.025) e creatinina sérica (r =−0,498; P = 0,025). A AUROC da razão Na/Ku em predizer Nau24h < 78 mEq/d foi de 0,948 ± 0,046 e o cut-off clássico da razão Na/Ku (≤1.0) exibiu VPP = 70%, VPN = 90%, acurácia = 80%, sensibilidade = 88% e especificidade = 75%.
Conclusão: Na/Ku ≤1 é sensível e específico e se correlaciona substancialmente com Nau24h, o que permite o uso desse teste na avaliação rotineira de pacientes com cirrose descompensada em ascite.
Palavras Chave: Cirrose hepática; Ascite; Sódio; Urina; Doença hepática terminal
Introduction
Ascites is defined as the pathological accumulation of fluid in the peritoneal cavity.1 There are three theories to explain the development of ascites in individuals with liver cirrhosis: underfill, overflow and vasodilatation. The modern view suggests that the three states are in greater or lesser extent, present in the same patient with cirrhosis.2 The underfill theory proposes that the two most important factors in the development of ascites are portal venous hypertension and failure of the liver to synthesize of albumin, which results in a reduction in plasma osmotic pressure. These factors lead to reduction in effective circulating volume, which activates the renin-angiotensin-aldosterone system and promotes the absorption of sodium and water. Ascites may be formed partly from the hepatic lymph and thoracic duct would be responsible for removing it. By these various compensatory mechanisms, body fluids are depleted, more ascites is formed and the cycle restarts.3 The overflow theory states that, initially, there would be increased sodium retention by the kidneys which would increase the effective circulating volume. Peripheral vascular resistance would decrease to accommodate hypervolemia. The encounter between hypervolemia and increased portal pressure would result in overflow that would form the ascites.4 The vasodilation theory explains that the ascites formation would start with arterial vasodilation in the splanchnic circulation secondary to portal hypertension. Then a hyperdynamic circulation would occur to maintain homeostasis. This compensatory mechanism, with the progress of the disease would be insufficient to support homeostasis. Blood pressure would decrease which would stimulate the baroreceptors and lead to increased homeostatic activity of the sympathetic nervous system, the renin-angiotensin-aldosterone system, circulation levels of antidiuretic hormone, and retention of sodium and water. The activation of these systems associated with decreased lymphatic return by splanchnic congestion would form the ascites.4 The vasodilation theory would be present in pre-ascitic phase and it would be importante in any subsequent developments. The overflow theory would be the most important aetiology in the first months of the development of ascites in individuals with cirrhosis, and the underfill theory explains most of the findings of ascites in patients with chronic decompensation.2
Ascites is considered the most common of the three major complications of cirrhosis. Other complications are hepatic encephalopathy and oesophageal variceal bleeding. About 50% of patients with compensated cirrhosis develop ascites over 10 years of follow-up.5 In 1 year with ascites, approximately 15% of patients will die, and 44% will die in 5 years.6
The mainstay treatments of patients with cirrhosis and ascites are: a low sodium diet (2000 mg/day = 88 mequiv./day) and diuretics.7 The measurement of urinary sodium excretion has been used for many years to identify the patient under sodium restrictive diet and distinguish him from those who require diuretics. Although spot urine Na measurement could be useful in this setting, the sodium excretion is not uniform during the day, which complicates the interpretation of results. For that reason, the most used method to estimate natriuresis is the measurement of 24-h urine sodium excretion (Nau24h). Patients with a restricted diet of 2000 mg of salt that does not lose weight and have Nau24h excretion ≥78 mequiv. Per day are usually labelled as noncompliant diet.8 Although widely requested in evaluating this group of patients, the collection of Nau24h can be cumbersome to the patient, nursing and physician. The patient may have difficulty storing urinary content (e.g., hepatic encephalopathy, management of the collector, embarrassment in front of other patients and visitors). Nursing may present difficulty in monitoring the urine collection and checking whether the collected volume actually corresponds to 24-h urine. The physician, when requesting the test makes urges for the result, which usually exceeds the 24 h of collection.
The Na/K ratio in spot urine sample (Na/Ku) is a practical way to identify Nau24h dosage lower than 78 mequiv.. Some evidence shows that this ratio is as useful and accurate as the collection Nau24h, but no Latin American study has evaluated this issue.9-15 This study aims to evaluate the accuracy of the Na/Ku ratio and compare it to Nau24h in the evaluation of natriuresis in patients with decompensated liver cirrhosis ascites.
Methods
This cross-sectional study assessed individuals with decompensated liver cirrhosis and ascites admitted to the hospital or treated in the outpatient clinics of Gastroenterology at University Hospital Polydoro Ernani de São Thiago of Federal University of Santa Catarina. Between August 2010 and January 2012, 42 patients admitted in the gastroenterology ward or in the outpatient gastroenterology clinic. The study protocol complies with the ethical principles of the Declaration of Helsinki and was approved by the local research ethics committee under number 322597.
Clinical variables of all individuals included in the study were collected in interview and confirmed in medical records. Laboratory parameters were extracted from medical records. The following variables were studied: age, gender, race, being a carrier of hepatitis B or C, alcohol consumption >40 g/day, diabetes mellitus, hypertension, liver cancer, history of upper gastrointestinal bleeding, spontaneous bacterial peritonitis, use of diuretics; serum creatinine, haemoglobin, platelets, sérum sodium, serum potassium, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), bilirubin, sérum albumin, international normalized ratio (INR), activated prothrombin time (APT); Nau24h dosage, sodium and potassium in urine sample. Biochemical liver tests AST, ALT, ALP and GGT were expressed as times the upper limit of normal (xULN). The other laboratory variables were expressed as absolute values. Examination of bilirubin, INR and creatinine values were used in the MELD calculation (Model for End-stage Liver Disease).16 The Na/Ku ratio is calculated on the values of sodium and potassium in spot urine sample. Urine was collected within less than or equal to 48 h from admission. Collection of 24-h urine sample for calculation of sodium was done in sterile plastic containers by recording the volume in 24 h; starting at 8:00 a.m. Instructions were given to assure completeness of collection. All samples were processed on the day of collection. In order to obtain the whole 24-h urinary sodium, sodium concentration was multiplied by the volume in litters. Random urine samples were obtained before or after completion of 24-h collection for measurement of spot Na/K ratio. Any kidney disease was excluded by medical history, urinalysis, sérum creatinine and ultrasound examination of the kidneys.
Numerical variables were expressed as mean and standard deviation, whereas categorical variables were described in absolute numbers and proportions. Continuous variables were compared using either Students t test or Mann-Whitney when appropriate, categorical variables were analysed using either Chi-squared test or Fishers exact test. A P-value < 0.050 was considered statistically significant. The correlation between the Nau24h and Na/Ku ratio was evaluated by the Spearmans correlation coefficient. Diagnostic accuracy of the Na/Ku ratio was analysed by estimating the area under the receiver operating characteristics curve (AUROC) and by calculating sensitivity, specificity, positive and negative predictive value. All tests were performed by the statistics software SPSS, version 17.0 (SPSS, Chicago, IL, USA).
Results
Sample analysis
Between August 2010 and January 2012, 42 patients admitted in the gastroenterology ward were evaluated for inclusion as they present liver cirrhosis decompensated in ascites. Twenty-two patients without urinary sodium dosage were excluded. Twenty patients with decompensated liver cirrhosis and ascites were included. Among them, 60% presented poor urinary sodium excretion (Nau24h dosage lower than 78 mequiv.).
Among the 20 included individuals, the mean age, standard deviation and median were 56.1±11.8 (54.5) years, 70.0% were men, 66.7% were Caucasian. Regard to the aetiology of cirrhosis: 33.3% had alcohol abuse and hepatitis C virus, 27.8% had alcohol only (Table 1). Three patients had hepatocellular carcinoma.
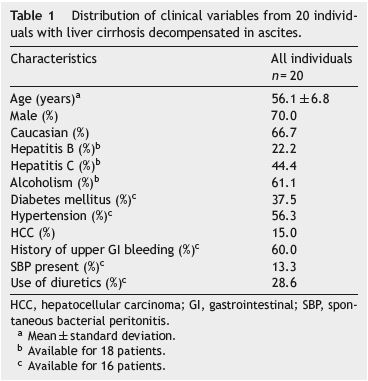
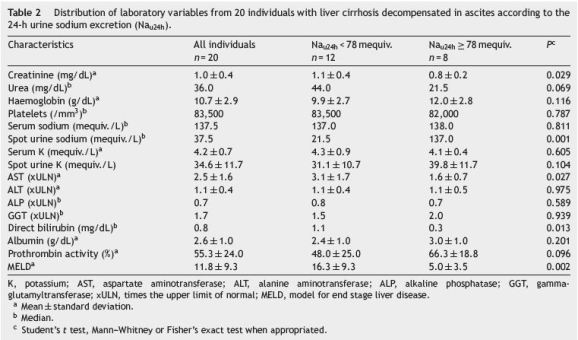
Evaluation of included patients according to the ability to excrete sodium (Nau24h)
When individuals with poor urinary sodium excretion were compared to those with Nau24h ≥ 78 mequiv. (Tables 1 and 2), they exhibited a higher proportion of male sex (91.7% vs. 37.5%; P = 0.018); higher mean MELD scores (16.3±9.3 vs. 5.0±3.5; P = 0.002), higher mean creatinine (1.1±0.4 mg/dL vs. 0.8±0.2 mg/dL; P = 0.029), higher AST means (3.1±1.7 vs. xULN 1.6±0.7; P = 0.027), higher median bilirubin (1.1 g/dL vs. 0.3 g/dL; P = 0.013) and lower median spot urine sodium (21.5 mequiv./L 222 vs. 137.0 mequiv./L; P = 0.001); P = no. No diferences were observed with respect to age, race, aetiology of cirrhosis, diabetes, hypertension, hepatocellular carcinoma, prior upper gastrointestinal bleeding, spontaneous bacterial peritonitis, current use of diuretics, urea, haemoglobin, platelets, serum sodium, serum potassium, spot urine potassium, ALT, ALP, GGT, albumin, and INR when individual with poor urinary sodium excretion were compared to those with Nau24h ≥78 mequiv.
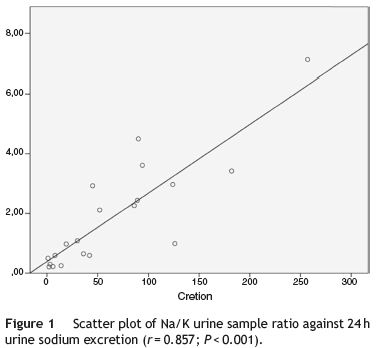
There was a strong positive correlation between the Na/Ku and Nau24h (r = 0. 857, P < 0.001) (Fig. 1). A negative correlation between MELD score (r =−0.498; P = 0.025) and serum creatinine (r =−0.498; P = 0.025) was evidenced. There were no significant correlations between the Na/Ku ratio and age, platelet count, serum sodium, AST, ALT, direct bilirubin, albumin and INR.
Performance of the Na/Ku ratio in predicting 24 h urinary sodium excretion
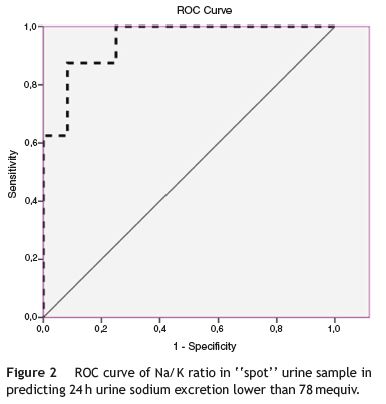
The AUROC for Na/Ku in the prediction of Nau24h < 78 mequiv. was 0.948±0.046, P = 0.001 (Fig. 2). Table 3 shows in details the diagnostic performance of the Na/Ku ratio in predicting Nau24h < 78 mequiv. For the Na/Ku ratio, the classical cutoff (≤1.0) showed 70% positive predictive value (PPV) to diagnose Nau24h dosage < 78 mequiv. with negative predictive value (NPV) of 90%, accuracy of 80%, 88% sensitivity and specificity of 75%.
Discussion
Cirrhosis is the twelfth leading cause of death in the United States of America.17 Several authors evaluated patients with decompensated liver cirrhosis ascites. Usually, the studied population is predominantly composed by men, 59-74%, age ranging from 53.6 to 60 years.18-20 In this study it has been observed that 70% of subjects were male; mean age was 56.1 years, which coincides with that described in literature. With regard to the aetiology of cirrhosis, it varies according to the prevalence of the diseases on the studied area, with a higher prevalence of HBV (64.8%) in China, higher incidence of alcoholic cirrhosis (76.4%) in Germany (19) and Barcelona (44.7%).18 The present study demonstrated a higher prevalence of HCV as compared to Europe and Asia, the latter being an area of high prevalence of HBV21 and exhibits high prevalence of alcoholism as a cause of chronic liver disease.
In cirrhosis, the development of ascites and diuretic response are determined by the renin-angiotensin- aldosterone and renal sodium handling.22 This study observed that patients presenting with more severe liver disease (MELD, creatinine, bilirubin, AST) are those who have lowest urinary sodium excretion. Likewise, Cholongitas et al. recently demonstrated that the factors independently associated with poor urinary sodium excretion in cirrhosis are albumin, creatinine and Na/Ku.11
The Na/Ku ratio emerged as an option to Nau24h in evaluating the ability of cirrhotic patients with ascites to excrete salt. During ascites treatment, absence of weight loss may be secondary to poor response to diuretics or a consequence of non-adherence to low sodium diet. It is important to recognize these differences to avoid possible complications caused by unnecessary increase in dosage of a diuretic, such as hepatic encephalopathy, renal dysfunction and electrolyte disturbance, and complications caused by the drainage of large volumes of ascitic fluid by paracentesis as mechanical trauma and circulatory dysfunction.23 Despite the good performance of the AUROC for Na/Ku in the prediction of Nau24h < 78 mequiv., these data should be cautiously interpreted, as Na/Ku ration is non-linear. Nevertheless, respectable negative predictive value, accuracy, sensitivity and specificity were good enough to support its routine use. Furthermore, these findings are supported by previous studies. After extensive literature review it has been verified that only eight studies9-15,24 compared Na/Ku ratio with Nau24h dosage in order to identify poor urinary sodium excretion (Nau24h < 78 mequiv.), and only three of them are complete articles.13,14,24 Two studies are letters to the editor11,15 and three are abstracts published in congress annals9,10,12, one of which is unavailable for consultation.9 These studies have identified different cut-offs for the Na/Ku ratio. The cut-off point of 1 currently recommended by American Association for the Study of Liver Diseases,1 is the most sensitive and specific 64-95% and 75-92%.10-12,15 However, Rojpalakorn et al. have identified low specificity (6%) for the classic cut-off, thus has questioned their practical application.24 In the present study, besides the high sensitivity and specificity demonstrated for 1 cut off Na/Ku ratio, it has been found strong positive correlation between Na/Ku ratio and Nau24h, previously demonstrated by Pinto-Marques et al.15 Other cut-off points for the Na/Ku ratio have been studied. The cut-offs 1.25 and 2.5 have demonstrated a specificity and a sensitivity ranging from 72% to 88% and 85% to 96%, respectively.13,14
Stiehm et al. analysed 729 specimens of urine in 21 patients, a similar number of individuals included in this study.10 The circadian variability was assessed analysing the Na/Ku ratio according to diuretic administration in diferente day periods and no differences were demonstrated between groups. Likewise, Park et al. analysed two dosages Na/Ku ratio, in the morning and afternoon to check whether the not uniform sodium excretion during the day interfere in the ratios inferred.14 Apparently the urinary potassium excretion varies in accordance with sodium, maintaining the proportion at different times of day. The present study evaluated only a single urine sample from each patient, as previously published by El-Bokl et al. and Rojpalakorn et al.13,24
Based on these data, we conclude that the Na/Ku ratio cut off point of 1.0 may be sensitive and specific to assess the ability of sodium excretion in patients with liver cirrhosis and ascites and it correlates strongly with Nau24h dosage, which enables the utilization of this simple and useful test in the routine evaluation of these patients.
References
1. Runyon BA. AASLD Practice Guidelines Committee Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087-92. [ Links ]
2. Andrade Junior DR, Galvão FHF, Santos AS, Andrade DR. Ascite - Estado da arte baseado em evidências. Rev Assoc Med Bras. 2009;55:489-96. [ Links ]
3. Sherlock S, Shaldon S. The aetiology and management of ascites in patients with hepatic cirrhosis: a review. Gut. 1963;4: 95-105. [ Links ]
4. Vicente A, Colmenero J. Ascites and hepatorenal syndrome in cirrhosis: pathophysiological basis of therapy and current management. J Hepatol. 2003;38 Suppl. 1:S69-89. [ Links ]
5. Ginés P, Quintero E, Arroyo V, Terés J, Bruguera M, Rimola A, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122-8. [ Links ]
6. Planas R, Montoliu S, Balleste B, Rivera M, Miguel M, Masnou H, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol. 2006;4:1385-94. [ Links ]
7. Runyon BA. Care of patients with ascites. N Engl J Med. 1994;330:337-42. [ Links ]
8. Runyon BA. Management of adult patients with ascites due to cirrhosis. Hepatology. 2004;39:841-56. [ Links ]
9. Karatapanis S, Ketikoglou I, Skorda L, Kopanakis D, Metaxaki P, Lisgos F, et al. The role of spot urine Na+/K+ ratio in the management of ascites in cirrhotic patients. Gut. 2003;52 Suppl. VI:A53. [ Links ]
10. Stiehm AJ, Mendler MH, Runyon BA. Detection of diuretic resistance or diuretic-sensitivity by spot urine Na/K ratios in 729 specimens from cirrhotics with ascites: approximately 90 percent accuracy as compared to 24-hr urine Na excretion. Hepatology. 2002;36:222A. [ Links ]
11. Cholongitas E, Karatapanis S, Nakouti T, Birtsou C, Skorda L, Kouvelis I, et al. Can 24 h urine sodium excretion be replaced by spot urine sodium/potassium in patients with decompensated cirrhosis? Liver Int. 2012;32:172-3. [ Links ]
12. Runyon BA, Heck M. Utility of 24-hour urine sodium collection and urine Na/K ratios in the management of patients with cirrhosis and ascites. Hepatology. 1996;24:571A. [ Links ]
13. El-Bokl MA, Senousy BE, El-Karmouty KZ, Mohammed IE, Mohammed SM, Shabana SS, et al. Spot urinary sodium for assessing dietary sodium restriction in cirrhotic ascites. World J Gastroenterol. 2009;15:3631-5. [ Links ]
14. Park JE, Lee CH, Kim BS, Shin IH. Diagnostic usefulness of the random urine Na/K ratio in cirrhotic patients with ascites: a pilot study. Korean J Hepatol. 2010;16:66-74. [ Links ]
15. Pinto-Marques P, Vieira A. Urinary sodium/potassium ratio on random sample as a useful tool to assess diuretic-induced natriuresis on chronic liver disease-associated ascitis. Am J Gastroenterol. 2007;102:212-3. [ Links ]
16. Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-70. [ Links ]
17. Minino AM, Heron MP, Smith BK. Deaths preliminary data for 2004. Natl Vital Stat Rep. 2006;54:1-7. [ Links ]
18. Fagundes C, Pépin MN, Guevara M, Barreto R, Casals G, Solà E, et al. Urinary neutrophil gelatinase-associated lipocalin as biomarker in the differential diagnosis of impairment of kidney function in cirrhosis. J Hepatol. 2012;57:267-73. [ Links ]
19. Wiegand J, Kühne M, Pradat P, Mössner J, Trepo C, Tillmann HL. Different patterns of decompensation in patients with alcoholic vs. non-alcoholic liver cirrhosis. Aliment Pharmacol Ther. 2012;35:1443-50. [ Links ]
20. Shi KQ, Fan YC, Ying L, Lin XF, Song M, Li LF, et al. Risk stratification of spontaneous bacterial peritonitis in cirrhosis with ascites based on classification and regression tree analysis. Mol Biol Rep. 2012;39:6161-9. [ Links ]
21. Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepatitis. 2004;11:97-107. [ Links ]
22. Salerno F, Guevara M, Bernardi M, Moreau R, Wong F, Angeli P, et al. Refractory ascites: pathogenesis, definition and therapy of severe complication in patients with cirrhosis. Liver Int. 2010;30:937-47. [ Links ]
23. Runyon BA, Antillon MR, Montano AA. Effect of diuresis versus therapeutic paracentesis on ascitic fluid opsonic activity and serum complement. Gastroenterology. 1989;97:158-62. [ Links ]
24. Rojpalakorn P, Thong-U-Thaisri P, Pramoolsinsap C. The diagnostic value of spot urine sodium-to-potassium (UNa/K) ratio compared to 24-hour urine sodium (24-hr UNa) for the management of cirrhotic patients with ascites. Thai J Gastroenterol. 2006;7:66-70. [ Links ]
*Corresponding author
E-mail address: janaina.narciso@uol.com.br (J. Luz Narciso-Schiavon).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgments
This paper is presented as partial fulfilment of the requirements for the Medical Doctor (MD) degree from the Federal University of Santa Catarina.
Received 7 February 2013; accepted 29 April 2013













