Introduction
Paraganglioma is an extra-adrenal tumor very similar to pheochromocytoma with no possible distinction in cell levels. Histology cannot differentiate them, so this is done by anatomical location. (Neumann, Young, & Eng, 2019) They are considered the most common benign tumors of the middle ear and arise inside of the temporal bone through the tympanic plexus. Paragangliomas represent less than 1% of tumors of the head and neck and the most common are those located in the carotid body. (Sweeney, Carlson, Wanna, Bennett, 2015). The term jugulotympanic paraganglioma should be used instead of tympanic glomus and jugular glomus. (Neumann, Young, & Eng, 2019; Thompson, 2006). The most frequently manifested symptoms are hearing loss and ipsilateral pulsatile tinnitus (SCHIPPER et al., 2004). They are highly vascularized tumors and can involve blood and neural vessels, often making treatment difficult (HU; PERSKY, 2003). Paragangliomas are rare tumors, essentially benign non-catecholamine-producing (Baysal, van Schothorst, Farr, Grashof, Myssiorek, Rubinstein,.,… Richard III, 1999), with an incidence associated with pheochromocytomas. A total of 500 to 1600 cases per year are registered in the United States (Chen, H., Sippel, R. S., O'Dorisio, M. S., Vinik, A. I., Lloyd, R. V., Pacak, K., & North American Neuroendocrine Tumor Society, 2010). The tympanic glomus is the second most common tumor of the temporal bone and the most common neoplasm of the middle ear, being more prevalent in women with a 3: 1 ratio in relation to men and with a higher incidence in the fifth decade of life (Bogar, Freitas, Caropreso, Miniti, Silva, & Bento, 1990; Singh, Badhwar, D'Souza, & Indrajit, 2004). Some syndromes have been associated with the occurrence of paragangliomas, but most of them occur spontaneously. These syndromes can occur at any age, but have a higher incidence between 40 and 50 years (Welander, Söderkvist, & Gimm, 2011).
Development
Clinical manifestations
Pulsatile tinnitus and hearing loss are the most frequent symptoms of tympanic paraganglioma (Neto, Vuono, Souza, Testa, Pizarro, & Barros, 2005; O'Leary, Shelton, Giddings, Kwartler, & Brackmann, 1991; Spector, Maisel, & Ogura, 1973). Tympanic paragangliomas can trigger clinical manifestations such as hypertension, sweating, headache, tachycardia, anxiety, tremors, pallor, nausea, abdominal and chest pain, in addition to local symptoms, which can cause severe cardiovascular and neurological diseases, although up to 10% can be asymptomatic. Most systemic clinical presentations are caused by sympathetic paragangliomas. Parasympathetic paragangliomas produce little or no catecholamine (Erickson, Kudva, Ebersold, Thompson, Grant, van Heerden, & Young, 2001; Welander, Söderkvist, & Gimm, 2011).
Classification
The Fisch and Mattox classification is used for jugulotympanic paragangliomas (Fisch, & Mattox, 1988) Table 1.
Case reports
Case 1
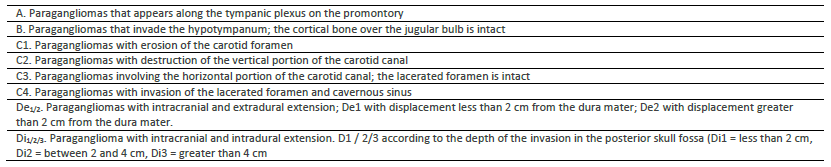
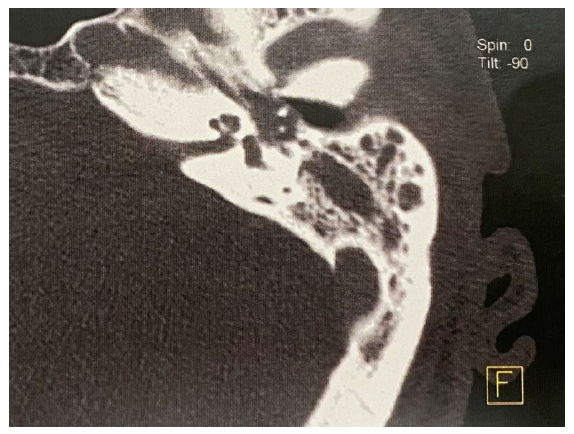
Patient I.F, female, 73 years old, with a history of pulsatile tinnitus on the left for approximately two years. Recent worsening. Associated hearing loss. He denies otalgia or otorrhea. Otoscopy showed an intact tympanic membrane with a red retrotympanic anterior tumor. Audiometry exam showing sensorineural loss on a downward ramp from 3000Hz. The tomography of the temporal bones showed an image of soft tissue density in the left middle ear occupying the anterior region. MRI suggestive of glomus. Undergoing exploratory tympanotomy under general anesthesia, with visualization of a pulsatile red mass in the middle ear, occupying the anterior region of the tympanic box. Mass resection with cauterization of the pedicle. Whole and mobile ossicular chain. Repositioning of the tympanic flap. Reports improvement in hearing and absence of tinnitus. It is classified as category A in the Fisch classification. Fig 1, Fig 2.
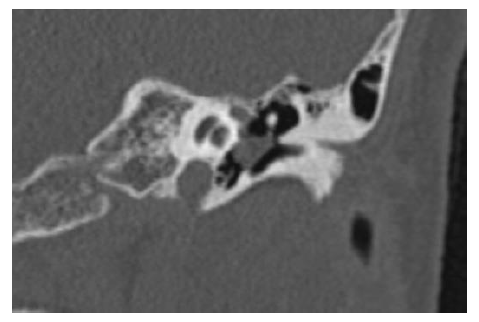
Figure 1 CT of temporal bones (coronal section) showing circumscribed veiling on the left promontory.

Figure 2 CT of temporal bones (axial section) showing circumscribed veiling on the left promontory. Mastoid without veiling.
Case 2
Patient B.A.O, male, 68 years old, with a history of hearing loss for four years without complaint of otorrhea or otalgia. Aural feeling of fullness. Denies tinnitus. Otoscopy showed an intact, white tympanic membrane. The tomography of the temporal bones showed the mastoid to be well cellularized, but veiled, as well as the left tympanic box. MRI did not suggest paraganglioma. Audiometry showing moderate to severe mixed loss on a downward slope. Undergoing an exploratory tympanotomy, with a posterior endaural incision under general anesthesia, with visualization of a pulsatile red mass occupying the entire middle ear, attached to the ossicular chain. Resection of the mass with cauterization of the pedicle with bipolar cautery. Whole and mobile ossicular chain. Repositioning of the tympanic flap. Reports improvement in hearing. It is classified as category B in the Fisch classification. Fig3
3.
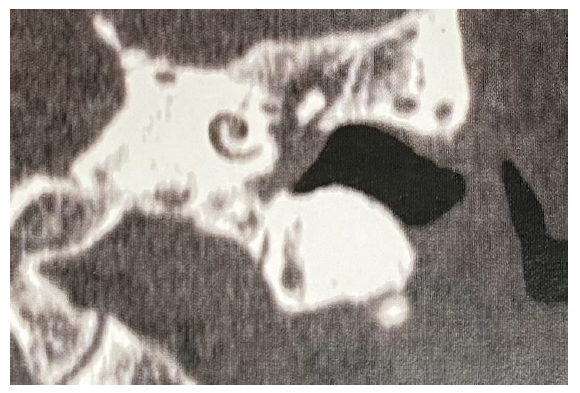
Figure 3 CT of temporal bones (coronal section) showing veiling of the entire tympanic box to the left.
Conclusions
The growth of tympanic paragangliomas is slow with benign behavior and mild symptoms when small. For this reason, the diagnosis often occurs when the tumor has reached larger dimensions. The most reported symptoms are tinnitus and hearing loss (Schipper, Boedeker, Maier, & Neumann, 2004). The physical examination may show a tumor with red retrotympanic color. Very typical clinical findings were observed in case 1. The patient, in this case, had pulsatile tinnitus and hearing loss, with a retrotympanic red mass (Tiago, Gil, Ribeiro, Anjos, Sens, & Valle, 2007). Hearing loss was not conductive, as in most cases, because the glomus did not affect the ossicular chain. The sensorineural loss of the patient suggests presbycusis, compatible with tomography and resonance exams. The patient in case 2 had no clinical signs suggestive of paraganglioma, did not report pulsatile tinnitus and only a sensation of aural fullness, being referred with suspicion of chronic otitis media. The total mastoid and middle ear veiling, seen on tomography, suggested chronic otitis media. The hypotransparency of the tympanic membrane did not allow the visualization of the retrotympanic lesion. These factors led to the intraoperative diagnosis of glomus in case 2. Fig. 4
The treatment of choice is surgery with endaural access in tumors located on the promontory (Woods, Strasnick, Jackson, 1993; Fleury, Legent, Marsault, Basset, Sterkers, & Compere, 1979). The endaural access was performed in both cases, with total resection of the lesion after cauterization of the vascular pedicle. Ligation of the pedicle and bleeding control facilitated complete resection of the lesion. The obliteration of the attic by the tumoral lesion may explain the mastoid veiling in case 2. The ossicular chain was not damaged. Both patients reported improvement in hearing after surgery and absence of pulsatile tinnitus in case 1.
Early diagnosis allows for a less invasive surgical approach with preservation of anatomical structures and auditory function in patients with tympanic paragangliomas. Patients with complaints of pulsatile tinnitus and / or conductive or mixed hearing loss should be investigated, early, with imaging tests. Thus, in patients presenting symptoms such as hearing loss and pulsatile tinnitus, an otological investigation is essential (Appannan, & Md Daud, 2018).