Introduction
The severe acute respiratory syndrome coronavirus (SARS-CoV-2) is rapidly infecting people around the world, resulting in the infectious disease COVID-19that has been declared a pandemic (Huang et al., 2020). Critical illness associated with SARS-CoV-2 infection is often associated with prolonged periods of intensive care treatment, with a consequent negative impact on clinical and functional results in the short and medium terms. Recipients of heart transplants (HT) may be at increased risk of adverse outcomes attributable to infection with COVID-19 because of multiple comorbidities and clinically significant immunosuppression; however, the effects of this disease in these patients are unclear (Bottio et al., 2021). To improve patients' quality of life, an integrated rehabilitative process that includes cardiac, respiratory, neuromuscular, and swallowing interventions, as well as psychological support, is recommended (Agostini et al. 2021). It is therefore predictable and desirable to actively participate in ICU rehabilitation.
1. Case presentation
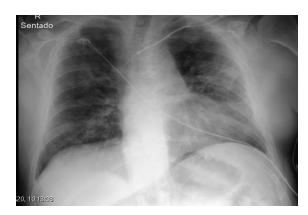
This case represents a 60-year-old man who had a heart transplant 9 months earlier, without complications, is diabetic, has chronic obstructive pulmonary disease (COPD), a history of dilated cardiomyopathy with recurrent heart failure admissions and end-organ hypoperfusion. He arrived at the hospital hypoxic and gradually deteriorated, necessitating non-invasive mechanical ventilation (Hi-Flow) and ICU care treatment. On admission to the ICU, he presented with respiratory distress and hypoxia, and the chest x-ray showed progressive bilateral pulmonary infiltrates (Figure 1). This was followed up with a 5-day history of cough, fever, and activity Intolerance.
Rehabilitation Nurses´ intervention started on the second day in the ICU. It focused on a respiratory and functional rehabilitation program, twice day for 30-45minutes each, for 10 days. Table 1 describes Rehabilitation Nursing diagnoses and interventions using International Classification for Nursing Practice (CIPE®) terms and is registered in the B-simple program. Some interventions respond to more than one diagnoses.
Table 1 Rehabilitation Nursing Plan.
| Date | Diagnoses | Intervention |
|---|---|---|
| 01/12 | Respiratory function: compromised | Breathing techniques (active cycle of breathing technique, thoracic expansion exercises, forced expiration technique) |
| Exercise Intolerance Knowledge about energy conservation techniques - not demonstrated | Get out of bed Teaching about energy conservation technics during activities (ex. eating, taking a bath, speaking…) | |
| Muscle movement: compromised | Active-assisted mobilization in all joints, 1 set, 10 repetitions | |
| 05/12 | Respiratory function: compromised | Breathing techniques (active cycle of breathing technique, thoracic expansion exercises, forced expiration technique) Inspiratory muscle training (spirometry)- 5 exercises 7 times/day |
| Muscle movement: compromised | Active-resisted mobilization in all joints, 1 set, 10 repetitions Strength training (0,5kg)- warms- 1 set, 5 repetitions | |
| Exercise Intolerance Knowledge about energy conservation Technics - not demonstrated | Aerobic training (cycle ergometer- 5 mints) Teaching about energy conservation technics during activities | |
| 07/12 | Respiratory function: compromised | Breathing techniques (thoracic expansion exercises) Inspiratory muscle training (spirometry)- 7 exercises 10 times/day |
| Exercise Intolerance | Aerobic training (cycle ergometer- 20mints), walk- 100 meters) | |
| Muscle movement: compromised | Active-resisted mobilization in all joints, 1 set, 15 repetitions, Strength training (0.5kg)- warms - 1 set, 9 repetitions (2 times/day) | |
| 09/12 | Respiratory function: compromised | Breathing techniques (thoracic expansion exercises) Inspiratory muscle training (spirometry)- 10 exercises 10 times/day |
| Activity intolerance | Aerobic training (cycle ergometer- 15+15mints), walk- 150 meters | |
| Muscle movement: compromised | Strength training (0.5kg), warms - 2 set, 8 repetitions (2 times/day) |
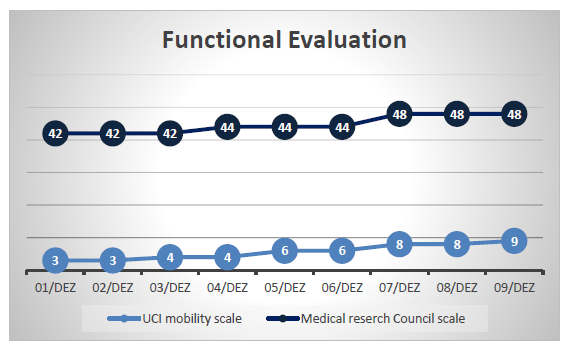
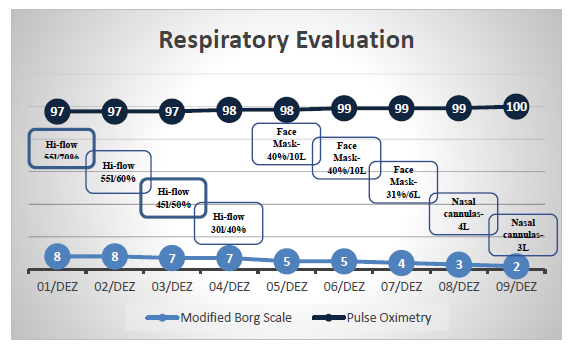
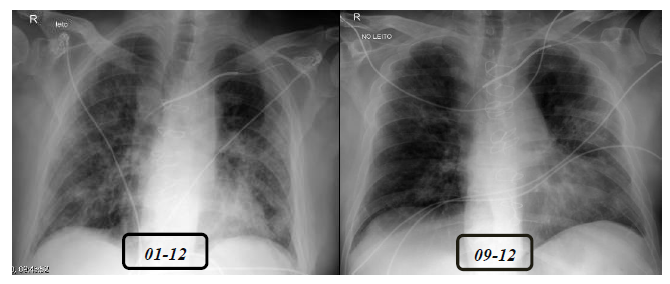
Results were evaluated using the ICU mobility scale (Hogdson et al, 2014), The Medical Research Council (MRC) Scale for Muscle Strength (Medical Research Council, 1976), modified Borg Scale (Borg, 1970), pulse oximetry, and with the improvement of rehabilitation nursing diagnoses. It was clear that there was a positive evolution, as is visible on Figure 2 and 3 and compared on the thoracic X-ray (Figure 4).
No adverse events were verified during the rehabilitation intervention. After 10 days, the patient was transferred to an inpatient unit and went home 3 days later.
2. Discussion
Patients with COVID-19 disease may need prolonged bed rest, leading to immobilization syndrome associated with respiratory dysfunction, both of which might require rehabilitation interventions. Prolonged immobility promotes muscle weakness, physical deconditioning, as well as changes in balance and posture, and joint stiffness and pain, which have a strong impact on patients’ general condition, quality of life, and self-care (Latif et al.,2020). This was the risk for this patient, aggravated by the fact that he had a heart transplant, was in recovery and was a COPD. So, rehabilitation interventions were focused on motor improvement and immobilization syndrome prevention, liked as described in the literature. Early mobilization and rehabilitation in ICU patients are widely shared and accepted, and have been supported by randomized controlled trials, systematic reviews, and recommendations (Clini & Ambrosino, 2005; Reid et al., 2018). Bernal-Utrera and colleagues (2021) described in their review that rehabilitation is a necessary strategy in critically ill patients with COVID-19 because it prevents complications and contributes to the stabilization of patients in critical periods, facilitating their recovery. They described that intervention could be based on three main treatment modalities: respiratory techniques, to favor pulmonary ventilation, the mobilization and excretion of secretions, and the stimulation of respiratory muscles; positional treatment, exercise therapy to improve immune function and reduce complications, favoring functional recuperation. In this case, rehabilitation nurse interventions were based on this.
The patient improved his functionality and became more independent in self-care and walking. Respiratory Rehabilitation was the most difficult aspect of providing consistent care in this situation, which was extremely demanding and could result in ICU staff shortages. It was needed to reduce unnecessary exposure of healthcare workers to the virus, so, for example aerosol therapy couldn't be used. Few rehabilitation exercises concerning COVID-19 patients were reported, but we know that they were necessary. A modified version of rehabilitation exercises based on the underlying mechanisms of the COVID-19 were applicable. These exercises aimed to improve the pulmonary function of patients and facilitate the airway cleaning process; some of them were done it in the prone position. As shown in Graph 2, there were improvements in hypoxemia and, subjective notion of effort, with a progressive reduction in the need for oxygen therapy as well as a thoracic x-ray.
With the patient's positive evolution, it was also possible to plan a low-intensity physical exercise with the monitoring of his subjective notion of effort, which included walking, cycloergonometry, and strength exercise with a 0.5 kg. The Uhlig and collegues (2022) described in their study that initiation of out-of-bed mobilization and the levels of mobility (sitting over the edge of the bed, sitting in a chair, standing, and ambulating) reached by critically ill patients with COVID-19during hospitalization achieved higher mobility levels in the ICU and at hospital discharge.