INTRODUCTION
Soccer players commonly compete with insufficient time for complete recovery between matches (Silva et al., 2018). This can result in exacerbated residual fatigue, manifested by an increase in indicators of exercise-induced muscle damage (EIMD) and inflammation, impaired performance, and delayed onset muscle soreness (DOMS) (Silva et al., 2018). Assessing residual fatigue markers provides valuable information about the muscle recovery status, allowing practitioners to analyse the athlete’s readiness to train and compete (Kellmann et al., 2018). Moreover, manipulating the training load according to the athlete’s recovery status is pivotal to preventing injuries, illness, and non-functional overreaching (Kellmann et al., 2018).
Infrared thermography (IRT) generates thermal images (thermograms) based on the infrared radiation emitted from objects, allowing us to quantify the skin temperature (Tsk) safely, contact-free, and non-invasively (Moreira et al., 2017). Tsk was suggested as a marker of residual fatigue, hypothesising that the inflammation in response to EIMD would increase the local Tsk across days following physical exercise (Fernandes et al., 2017). However, Tsk monitoring via IRT to detect residual fatigue in athletes remains unclear in the literature since the results of different studies on this topic are contradictory. For example, some authors have reported Tsk increments in the subsequent days following exercise (Uchôa et al., 2018; Priego-Quesada, Oficial-Casado, Gandia-Soriano, & Carpes, 2019; Rojas-Valverde, Gutiérrez-Vargas, Sánchez-Ureña, Gutiérrez-Vargas, & Priego-Quesada, 2021), whereas others have failed to find Tsk changes after EIMD (Pérez-Guarner et al., 2019; Barboza et al., 2021; Ferreira-Júnior et al, 2021).
Therefore, to date, evidence is lacking to support the use of Tsk measurements to infer muscle recovery status. Research studies conducted with rigorous control of intervening factors on Tsk are necessary to address this question, although they are scarce (Fernandes et al., 2017; Priego-Quesada et al., 2019). Investigating the Tsk response to exercise in an athlete following a standardised daily routine in a military base could provide an appropriate experimental control, helping us understand the impact of exercise-induced fatigue on Tsk. Thus, the purpose of this study was to analyse the effect of different volumes of a soccer simulation protocol (SSP) on Tsk, muscle damage, and inflammation in a military player in a boarding school. We hypothesise that a 90-min SSP would induce muscle damage and inflammation, which would result in Tsk increases during the post-exercise recovery period.
METHODS
This single-case study involved a reversal design, which allows for rigorous experimental evaluation of intervention effects and a strong basis for establishing causal inferences (Lobo, Moeyaert, Baraldi Cunha, & Babik, 2017). Single-case research design aims to observe one or a few subjects’ outcomes as a dependent variable at different moments and to compare the changes for assessing the impact of interventions (Kinugasa, Cerin, & Hooper, 2004; Lobo et al., 2017).
We analysed the effects of two sessions of an SSP (45 min vs 90 min) on the lower limbs’ Tsk in a young soccer player to investigate whether IRT would detect residual fatigue. Residual fatigue was characterised through perceptual measures (DOMS) and blood biomarkers of muscle damage (creatine kinase [CK]) and inflammation (C-reactive protein [CRP]), which have been suggested to study soccer-induced fatigue (Silva et al., 2018; Souglis, Bogdanis, Chryssanthopoulos, Apostolidis, & Geladas, 2018; Rodrigues Júnior et al., 2021). We analysed a military participant since the standardised routine in a military base contributes to strict control of confounding factors on Tsk, which is a differential of our study. Moreover, the SSP applied has been demonstrated to be effective in inducing residual fatigue, providing us with internal validity and experimental control (Da Silva & Lovell, 2020).
A 90-min SSP session was applied to induce residual fatigue, and a 45-min session was considered a control condition. Temperature and relative humidity during the interventions were similar: 22.5± 0.1°C, 55.3± 1.5% (45-min SSP); 23.3± 0.9°C, 42.7± 1.1% (90-min SSP) (Davis, Vantage Vue, Hayward, CA, USA). The two SSP trials were conducted on a natural grass soccer pitch, from 4 to 6 PM, separated by 7 days. Measures of Tsk, DOMS, and blood samples to quantify biochemical markers were collected at 6 moments: 24 h pre (baseline), 24 h (Post24h), and 48 h (Post48h) post the beginning of each experimental condition (recovery period).
Throughout the study, the participant followed a standardised routine. He abstained from any physical exercise for four days before the beginning of the study and during the whole data collection period. No strategy for enhancing recovery from EIMD and inflammation was applied. Figure 1 represents the study design, data collection, and intervention timeline, and Table 1 shows the participant’s routine.
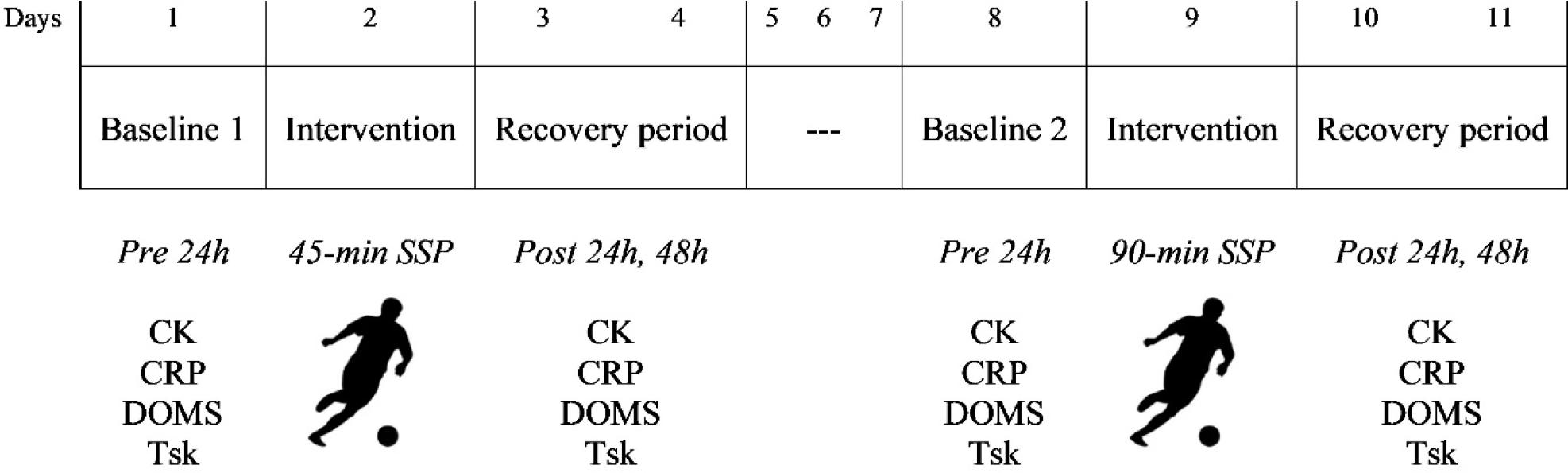
CK: creatine kinase; CRP: C-Reactive Protein; DOMS: delayed onset muscle soreness; Tsk: skin temperature; SSP: soccer simulation protocol.
Figure 1. Schematic representation of the study design.
Table 1. Participant’s daily routine*.
| Time | Activity |
|---|---|
| 6:00 | Waking up |
| 6:00 - 6:45 | Breakfast |
| 7:00 - 9:25 | Theoretical classes |
| 9:25 - 9:50 | Class interval and snack |
| 9:50 - 12:15 | Theoretical classes |
| 12:25 - 13:50 | Lunch |
| 13:50 - 15:35 | Theoretical classes |
| 16:00 - 18:00 | Data collection and intervention) |
| 18:00 - 19:00 | Dinner |
| 19:00 - 21:00 | Accommodation (resting or studying) |
| 21:00 | Supper |
| 22:00 | End of the routine (turn the lights off and sleep time) |
*When there was no data collection, the participant could rest or study at the accommodation or be engaged in non-fatiguing activities in a leisure room (e.g., playing video games, snooker, or watching tv).
Participant
The participant is a right-handed midfielder, non-smoker, and member of a soccer team at an Air Force Academy Preparatory School (age, 17 years old; height, 179 cm; body mass, 68.1 kg; Σ3 skinfolds, 21 mm; VO2max, 54.5 mL·kg−1 ·min−1). His futsal and soccer experience was 5 years and 2.6 years, respectively. Four weeks before the intervention, the participant’s health condition was attested through a medical check-up; then, he was familiarised with an SSP (Da Silva & Lovell, 2020), and his VO2max was predicted through Yo-Yo intermittent recovery test level 1 (Bangsbo, Iaia, & Krustrup, 2008). He regularly participated in 4-5 training sessions a week (1 h 45 min) and played 6 friendly matches during the season (during the last 4 months). No recent history of musculoskeletal injury was reported, and no consumption of aid supplements or medications for 6 months before and during the study. The participant and his guardians were informed about the study procedures and risks involved before giving written consent to participate. This study is part of a larger study approved by the local Research Ethics Committee (no. 3.303.938).
Procedures
The participant completed two sessions (45 and 90 min) of an SSP played from audio commands. This protocol includes technical and jumping activities, and its external validity to mimic the external load and physiological responses to soccer-match play has been previously demonstrated (Da Silva & Lovell, 2020). Both sessions were preceded by a 10-min standardised warm-up consisting of jogging, running drills, and stretching. Heart rate (HR) was monitored every 5 min (FT1, Polar, Kempele, OULU, Finland) and rating of perceived exertion (RPE) every 15 min on a 0-10 scale (Foster et al., 2001). Moreover, the internal load was quantified through the session RPE method (Foster et al., 2001), multiplying the protocol duration (in minutes) by the RPE score acquired 30 minutes post-SSP.
Data collection was conducted at the same time of the day to minimise circadian variation (Fernández-Cuevas et al., 2015). Previously, the participant was asked to avoid sun exposure, alcoholic beverages, caffeine, ointments, cosmetics, and showering for 4 h before the assessment. Moreover, urine specific gravity was assessed daily on a refractometer (a300, Atago, Ribeirão Preto, SP, Brazil) to ensure an appropriate hydration status (< 1.020 g·mL−1) (Barley, Chapman, & Abbiss, 2020).
First, a venous blood sample was collected for analysis of creatine kinase (CK) (UV Kinetic) and high-sensitivity C-Reactive Protein (CRP) (Immunoturbidimetry). The samples were centrifugated at 3,500 rpm for 10 min, and aliquots were stored at -20°C until further analysis. After the blood collection, the participant was acclimated for 10 min (Marins et al., 2014), wearing a swimming suit, in a thermo-neutral room (temperature: 20.5± 0.4°C; humidity: 60.5± 4.2%) controlled by an air-conditioning system (Split, Consul, São Bernardo do Campo, SP, Brasil). There was no ventilation directed to the participant. After that, two thermograms of the participant’s front and rear lower limbs were obtained through a T420 imager (FLIR Systems, Stockholm, Sweden) with 2% accuracy, at 7.5–13 μm infrared spectral band, 60 Hz refresh rate, autofocus, and 320 × 240 pixels. The precision of detecting a temperature change was ≤ 0.05°C. The camera was turned on 30 minutes before the measurements to allow sensor stabilisation. It was positioned on a tripod 2.4 meters from the volunteer, perpendicular to the regions of interest (ROIs). Emissivity for human skin was set at 0.98. The procedures for recording the thermograms followed the Thermographic Imaging of Sport and Exercise Medicine consensus statement recommendations (Moreira et al., 2017). Thermograms were analysed using the KELVIN+® software (Radsquare Tecnologia, São Paulo, SP, Brazil), version 1.0; mean Tsk was automatically quantified for quadriceps, hamstrings, hip adductors, and gastrocnemius. Figure 2 presents two thermograms indicating the ROIs analysed. Finally, the participant rated his perception of DOMS for quadriceps, hamstring, and gastrocnemius on a visual analogue scale ranging from 0 (absence of soreness) to 10 cm (very intense soreness).
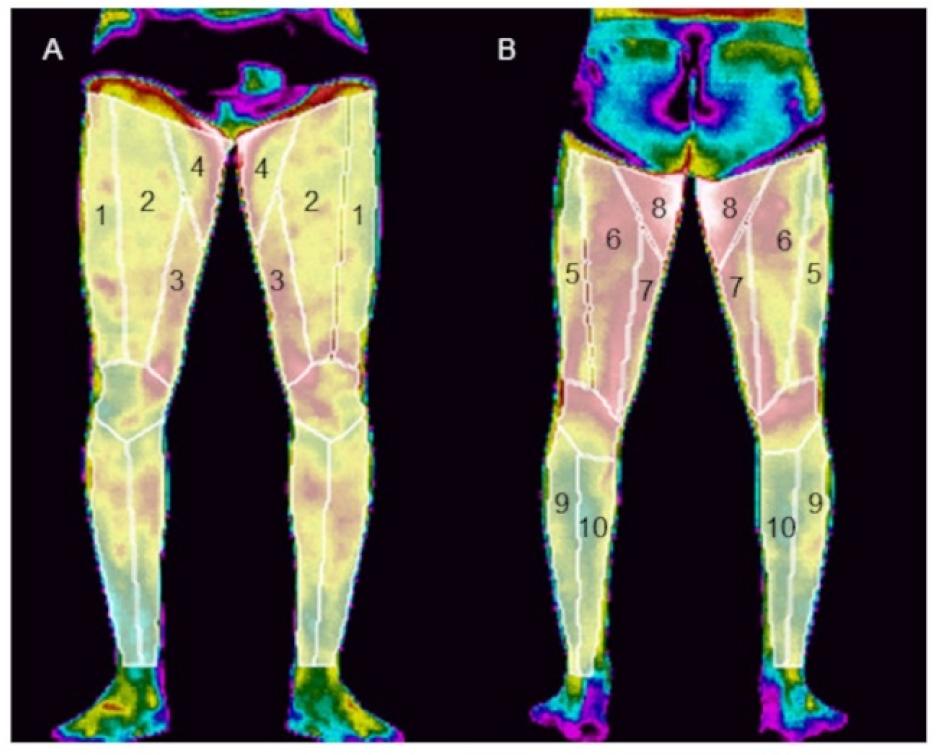
1: vastus lateralis; 2: rectus femoris; 3: vastus medialis; 4: hip adductor; 5: biceps femoris; 6: semitendinosus; 7: semimembranosus; 8: hip adductor; 9: gastrocnemius lateralis; 10: gastrocnemius medialis.
Figure 2. Thermograms with regions of interest analyzed: (A) front lower limbs; (B) rear lower limbs.
Data analysis
Differences relative to baseline values were expressed as percentage changes for CK and CRP data and absolute changes for mean Tsk. Pixels with temperatures higher than 33°C were quantified (Excel, Microsoft, Redmond, WA, USA) as a percentage related to the total of lower limbs’ pixels (excluding the background pixels). This Tsk threshold (> 33°C) was established according to a previous study (Rodrigues Júnior et al., 2021). Moreover, percentage changes for these pixels over time were calculated.
RESULTS
Heart rate, rating of perceived exertion, and internal load (session rating of perceived exertion × time)
During the SSP sessions, the average HR was similar between conditions (90-min SSP: 155± 7.6 bpm vs 45-min SSP: 158± 5.3 bpm). Relative to peak HR, the protocols’ intensity was 85.9% and 84.7% for the 90-min and 45-min SSP conditions, respectively. During protocols, the average RPE was 5.5± 1.6 (90-min SSP) and 5.3± 1.1 (45-min SSP). As intended, the internal load was 2.1 folds higher for the 90-min vs 45-min SSP (690 vs 330 arbitrary units, respectively).
Biochemical markers
The CK and CRP values are presented in Table 2.
Table 2. Changes in Creatine Kinase and C-Reactive Protein in response to different volumes of a soccer match simulation protocol.
| Variable | Protocol (min) | Time-point of measurement | ||
|---|---|---|---|---|
| Pre 24 h | Post 24 h | Post 48 h | ||
| Creatine Kinase (U·L−1) | 90 | 90 | 336 | 257 |
| 45 | 98 | 157 | 149 | |
| C-Reactive Protein (mg·L−1) | 90 | 0.40 | 1.13 | 2.13 |
| 45 | 0.70 | 0.50 | 0.42 | |
CK appeared to be similar at baseline (Pre24h) between conditions. CK peaked 24 h post the 90-min SSP, with values 3.7 folds (273.3%) higher than baseline, remaining elevated 48 h post (2.8 folds, 185.6%). Although CK increased 24 h (1.6 folds, 60.2%) and 48 h (1.5 folds, 52%) post the 45-min SSP, its values were not consistent with EIMD. Regarding CRP, its values increased 2.8 folds (182.5%) 24 h post and peaked 48 h post the 90-min SSP (5.3 folds, 432.5%). There was no increase in CRP following the 45-min SSP.
Perceptual response
The participant only reported DOMS (0-10) for quadriceps (1 point) 24 h post the 90-min SSP and for gastrocnemius 24 h (4 points) and 48 h (2 points) post the 90-min SSP.
Skin temperature
Table 3 presents the Tsk values and the differences relative to baseline (∆) following the SSP sessions.
Table 3. Tsk changes in response to different volumes of a soccer match simulation protocol.
| Region of interest | SSP (min) | Time-points of measurement | Difference to baseline (∆) | |||
|---|---|---|---|---|---|---|
| Pre 24 h | Post 24 h | Post 48 h | ∆ 24 h | ∆ 48 h | ||
| Skin temperature (°C) | ||||||
| Vastus lateralis | 90 | 32 | 32.84 | 32.55 | 0.84 | 0.55 |
| 45 | 32.16 | 31.81 | 30.46 | -0.36 | -1.70 | |
| Rectus femoris | 90 | 32.43 | 32.96 | 32.84 | 0.53 | 0.41 |
| 45 | 32.82 | 32.18 | 31.42 | -0.64 | -1.39 | |
| Vastus medialis | 90 | 32.75 | 33.12 | 33.26 | 0.37 | 0.51 |
| 45 | 32.88 | 32.32 | 31.76 | -0.56 | -1.12 | |
| Hip adductor (anterior view) | 90 | 32.67 | 33.20 | 33.09 | 0.53 | 0.42 |
| 45 | 33.18 | 32.57 | 31.84 | -0.61 | -1.33 | |
| Biceps femoris | 90 | 32.23 | 32.84 | 32.96 | 0.61 | 0.73 |
| 45 | 32.36 | 32.06 | 31.69 | -0.30 | -0.67 | |
| Semitendinosus | 90 | 32.87 | 33.09 | 33.04 | 0.22 | 0.17 |
| 45 | 32.92 | 32.31 | 32.25 | -0.60 | -0.67 | |
| Semimembranosus | 90 | 32.96 | 33.35 | 33.26 | 0.39 | 0.30 |
| 45 | 33.08 | 32.36 | 32.33 | -0.72 | -0.75 | |
| Hip adductor (posterior view) | 90 | 33.50 | 33.99 | 33.79 | 0.50 | 0.30 |
| 45 | 33.53 | 33.20 | 32.93 | -0.33 | -0.61 | |
| Gastrocnemius lateralis | 90 | 30.78 | 31.74 | 31.26 | 0.96 | 0.48 |
| 45 | 30.97 | 30.23 | 30.94 | -0.73 | -0.02 | |
| Gastrocnemius medialis | 90 | 30.48 | 31.75 | 31.22 | 1.27 | 0.74 |
| 45 | 30.95 | 30.03 | 30.85 | -0.93 | -0.10 | |
SSP: soccer simulation protocol.
When comparing the basal Tsk between conditions (Pre24h), only small differences were observed (vastus lateralis: 0.16°C; rectus femoris: 0.39°C; vastus medialis: 0.13°C; hip adductor in the anterior view: 0.51°C; biceps femoris: 0.13°C; semitendinosus: 0.05°C; semimembranosus: 0.12°C; hip adductor in the posterior view: 0.03°C; gastrocnemius medialis: 0.47°C; gastrocnemius lateralis: 0.19°C). Following the 45-min SSP, Tsk reduced in all analysed ROIs both 24 h and 48 h post protocol. On the other hand, when the participant underwent the 90-min SSP, Tsk increased 24 h and 48 h post protocol in all ROIs.
Figure 3 shows the thermal changes over time referent to the pixels with temperatures higher than 33°C (highlighted in red). Figure 4 presents these pixels quantified as a percentage of the total number of pixels overlying the lower limbs.
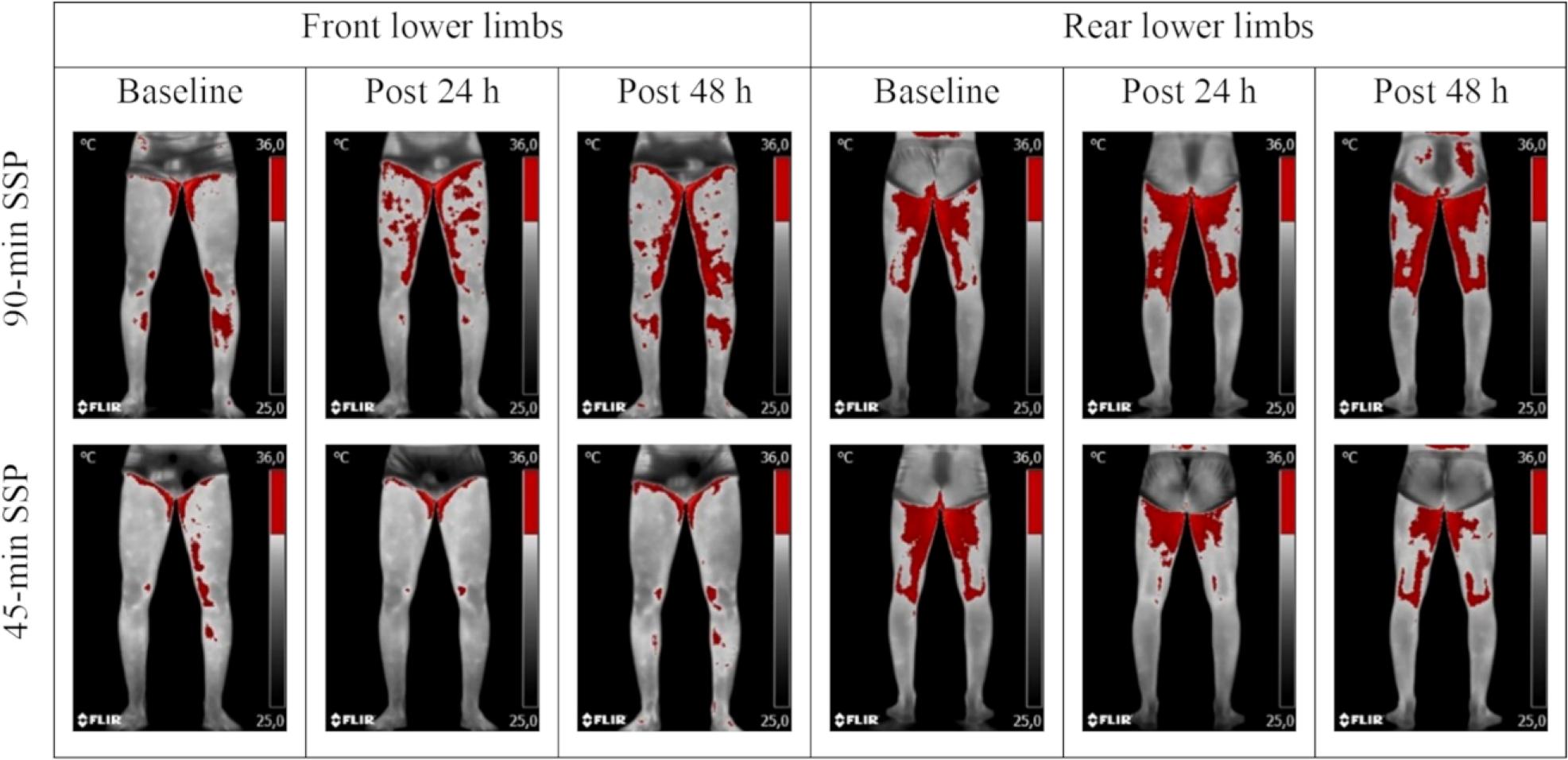
*Red pixels represent temperatures higher than 33°C; SSP: soccer simulation protocol.
Figure 3. Participant’s thermograms at moments 24 h pre (baseline), 24 h post, and 48 h post the experimental conditions*.
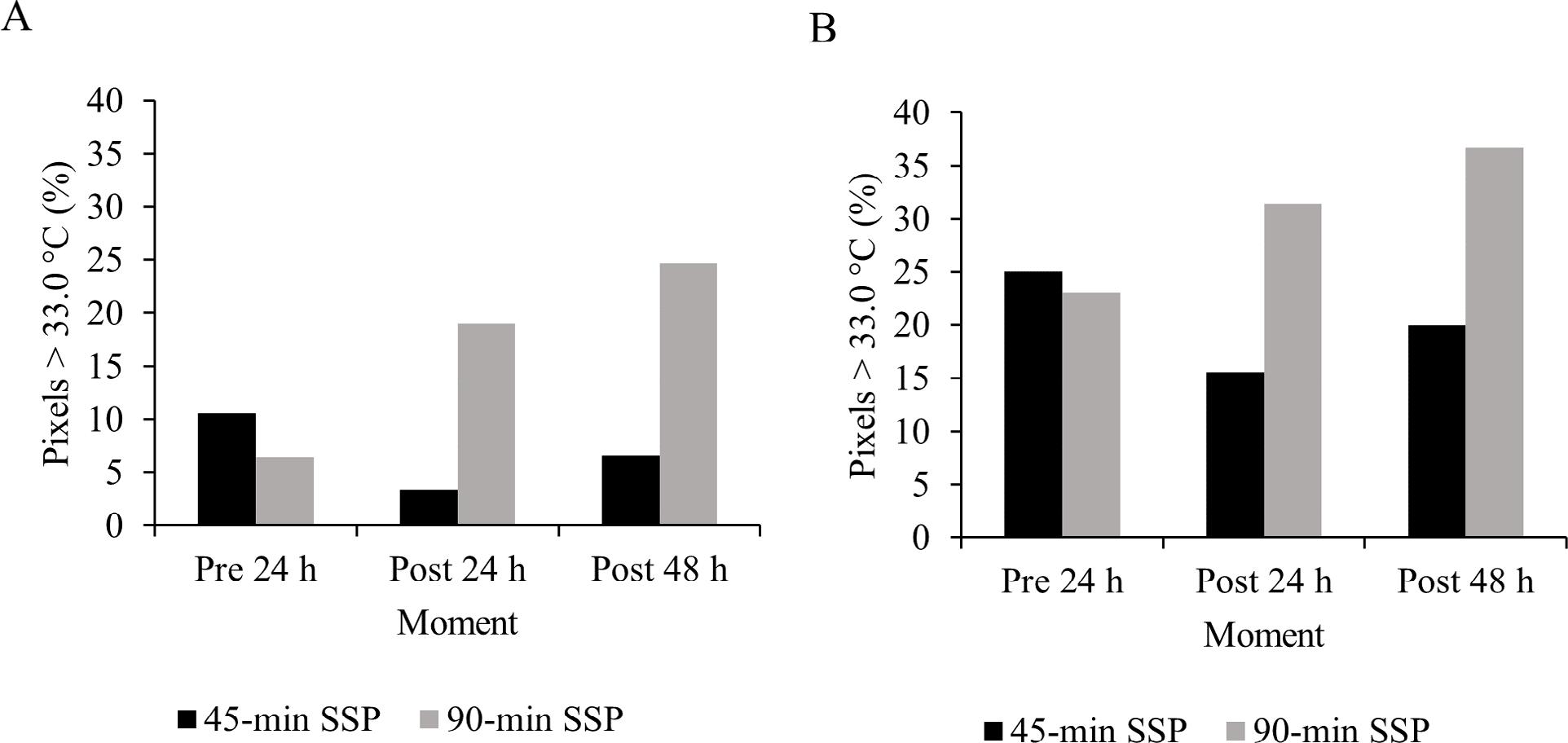
SSP: soccer simulation protocol; A: front lower limbs; B: rear lower limbs.
Figure 4. Percentage of pixels with temperatures higher than 33°C in the participant’s thermograms.
At baseline (Pre24h), thermograms appear to be very similar. Following the 90-min SSP, red pixels (> 33°C) increased 196.88% (Post24h) and 285.94% (Post48h) over the front lower limbs, and 35.93% (Post24h) and 58.87% (Post48h) over the rear lower limbs when compared to Pre24h (Figure 4A). Oppositely, following the 45-min SSP, red pixels were reduced by 67.92% (Post24h) and 37.74% (Post48h) on the front lower limbs, and 37.74% (Post24h) and 20.32% (Post48h) on the rear lower limbs (Figure 4B).
DISCUSSION
This study analysed the effect of different volumes of an SSP on the lower limbs’ Tsk in a young player to investigate whether IRT can detect residual fatigue. We found similar Tsk values before the two interventions (Pre24h), with differences of < 0.2°C in 7 ROIs and ≤ 0.5°C in 3 ROIs. This demonstrates that the participant’s standardised routine and compliance with the previous instructions for the thermographic evaluation mitigated interferences of confounding factors on Tsk. The two SSP sessions reproduced the physiological response of an official soccer match, as observed by the similar average HR during interventions (~85% of the peak HR). Moreover, as expected, the 90-min SSP induced residual fatigue, which is in line with a previous study (Da Silva & Lovell, 2020).
Our results indicate that IRT can be potentially sensitive to detect soccer-induced residual fatigue. We observed a marked increase in the lower limbs’ Tsk 24 h and 48 h post the 90-min SSP. The most remarkable changes occurred on gastrocnemius lateralis and medialis 24 h post-SSP, increasing 1.3 and 1°C, respectively (Table 3). This thermal response was accompanied by DOMS in the quadriceps and gastrocnemius and increases in muscle damage and inflammation blood biomarkers, suggesting that the participant was not completely recovered 48 h after the 90-min SSP. Conversely, Tsk reduced after the 45-min SSP in all ROIs, when no sign of DOMS, muscle damage, or inflammation was observed.
These findings support the effect of residual fatigue on Tsk and suggest that inflammation may partly explain our results. The high demands of soccer matches induce muscle damage due to intense activities that require eccentric work, such as sprints, acceleration, deceleration, changes of direction, jumps, and kicks (Silva et al., 2018; Souglis et al., 2018). EIMD triggers a mandatory inflammatory response for proper muscle repair and regeneration (Peake, Neubauer, Gatta, & Nosaka, 2017; Chazaud, 2020). During inflammation, physiological processes such as muscle vasodilation, increased blood flow, and high local metabolism generate heat (Scott, Khan, Roberts, Cook, & Duronio, 2004; Peake et al., 2017; Chazaud, 2020), which could impact the local Tsk.
Our study reinforces the findings of Rodrigues Júnior et al. (2021), who reported higher Tsk values, CK, and CRP levels after a competitive season in professional soccer players, and Fernandes et al. (2017), who reported Tsk and CK increases following two consecutive official soccer matches, separated by 3 days, in elite under-20 players. The Tsk increment was of lower magnitude in our study since SSP induces a lower magnitude of inflammation when compared to official matches (Silva et al., 2018). However, applying this SSP allowed us a better experimental control due to the standardised actions and absence of collision and fall, common in official matches.
Although it appears plausible that exercise-induced inflammation increase Tsk, some authors have observed no Tsk change after resistance exercise (Ferreira-Júnior et al., 2021), eccentric exercise-induced muscle damage (Barboza et al., 2021), or long-distance running (Pérez-Guarner et al., 2019). Moreover, the Tsk response to marathon running has not been associated with indirect markers of muscle damage (Rojas-Valverde et al., 2021). Therefore, more studies are needed to understand the impact of muscle damage and inflammation on Tsk and which mechanisms interfere with the thermal response following exercise.
A limitation of the study is that we analysed only a single basal Tsk measurement before the intervention. Since many factors affect Tsk (Fernández-Cuevas et al., 2015), it is interesting that further studies record additional measures of basal Tsk to calculate the typical error of the measurement, especially when the control of intervening factors is impaired. This can help researchers and coaches to establish a normal range of thermal variability and monitor Tsk changes individually in response to training/competition. Another limitation is that we did not evaluate muscle function and performance parameters, which would have helped us better characterise the magnitude of SSP-induced fatigue.
Further group-based studies should analyse the Tsk response to simulated soccer matches, including a control group (no exercise), and investigate if intensified periods of training or competition (e.g., preseason, congested matches schedule) induce cumulative Tsk increases during the recovery period. This would allow analysing the impact of greater magnitudes of residual fatigue on Tsk. Finally, it is interesting to study the association between the Tsk response to exercise and a set of markers of recovery, including psychological, physiological, muscle function, and performance parameters. Muscle function measured as maximal voluntary contraction torque deserves attention in this context since it has been appointed as the main EIMD indirect marker (Damas, Nosaka, Libardi, Chen, & Urinowitsch, 2016).
CONCLUSIONS
IRT detects residual fatigue induced by a simulated soccer match in a young military player. Monitoring Tsk changes via IRT can be a promising alternative to monitoring the individual state of muscle recovery. As a practical application, we suggest IRT could be regarded as a multivariate approach for monitoring residual fatigue in soccer players. IRT can help coaches and support staff analyse the individual muscle recovery state objectively, quickly, and non-invasively by contrasting Tsk changes with the individual thermal profile.















