Introduction
Rare disease (RD) is defined by the European Commission on Public Health as any life-threatening or chronically debilitatin disease existing at a prevalence of less than one case per two thousand people.1,2However, according to Orphanet, this rarity is bound to the region where it happens and the number of people affected compared to the general population.3 Characteristics such as chronicity, unknown etiology, lack of treatment, or limitations in the quality of life must be present for a disease to be considered rare.4 RDs’ origin is mostly genetic (80%) but can also be congenital or neurological.4,5
Currently, there are 300 million people with RDs worldwide, of which around 18 to 30 million are in the European Union.3,6In Portugal, it is estimated that between 600000 to 800000 individuals have an RD.6
Oral health is a fundamental right that contributes to every individual’s quality of life and well-being.7,8 People with disabilities (PwD) have poorer oral health and, consequently, a worse quality of life.9,10 Additionally, some have a profound disability with a higher need for oral hygiene assistance and poor access to oral health care, which further compromises oral health.11
As with other disabilities, people with an RD often experience difficulties in performing oral hygiene, becoming more susceptible to oral problems. Moreover, dental anomalies, malocclusion, lower access to oral health services, and lower quality of care are more frequent in these individuals.12-14 While oral diseases and their manifestations in each RD have been established, some data suggest that 15% of RDs impact oral health and the necessity of dental care.15
Individuals with RDs require early and specialized oral health care, which is usually difficult to obtain due to the lack of trained and skilled oral health professionals. In addition, due to heavy daily routines and a lack of information, the caregivers of individuals with RDs tend to neglect oral health.14
The Faculdade de Medicina Dentária da Universidade de Lisboa (FMD-UL) has been providing appointments for PwD, including patients with RDs, since 1986. This study aimed to analyze the patient profile and characterize the oral health status of individuals with an RD who visited the FMD-UL, as well as the difficulties in their daily oral hygiene.
Material and methods
This observational, analytical, cross-sectional study included a non-probabilistic sample consisting of individuals with na RD, according to Orphanet.3 Orphanet is a unique resource that gathers knowledge on RDs to improve the diagnosis, care, and treatment of patients with RDs. This initiative became a European endeavor in 2000, supported by grants from the European Commission.3
This study was authorized by the Ethics Committee of FMD-UL. The collected data were used exclusively for statistical purposes, the information was confidential, and the patients were identified only by the clinical file number. All patients or their caregivers gave explicit informed consent for the use of information for academic or research purposes on their first appointment at FMD-UL.
A single researcher collected all data by analyzing the clinical files of patients who attended the clinic for PwD at FMDUL between January 2015 and December 2019. The researcher collected data on each patient’s profile, oral habits, and clinical data. The patients’ profile data included age, sex, main deficiency condition and comorbidities, mobility, daily activity dependency, and communication. The oral habits variables encompassed toothbrushing frequency, oral hygiene difficulties, chewing ability and type of diet, and non-nutritive sucking habits. The clinical data included the Decayed, Missing, and Filled Teeth index (DMFT) for assessing the oral condition,16 the bleeding index (BI-S) for gingival health,17 and the simplified debris index (DI-S).18
Data was analyzed using the Statistical Package for the Social Sciences software program (IBM SPSS Statistics Base version 26.0.). The sample’s characterization and the questionnaire answers were structured through descriptive statistical methods by calculating absolute and relative frequencies. Numerical data were organized following the measures of central tendency (mean), dispersion (standard deviation), and range (minimum and maximum), depending on the type of variable under study.
Results
Among the 555 clinical files of patients who attended FMD-UL’s oral health clinic for PwD between 2015 and 2019, 64 (11.5%) individuals had 33 different RDs. This sample’s mean age was 32.8 years (±10.29), between 9 and 52 years old, and the male sex was the most prevalent (35; 54.7%) (Table 1). Most individuals were institutionalized (42; 65.9%).
Among the RDs found (n=33), the most prevalent was Rett syndrome (n=7; 21.2%). Among the total sample, 40.6% (26) were not able to communicate, most (39; 60.9%) required assistance for activities of daily living, and 48.4% (31) had difficulty in mobility (Table 1).
Around 60.9% (39) of patients had some non-nutritive sucking habit, and the most common was pacifier sucking (21; 32.8%). The number of individuals with RDs with any non-nutritive sucking habits was 10 (30.3%). Regarding their diet, 71.9% (46) consumed a normal diet, and 29.7% (19) showed deficient chewing. However, 9.4% (6) of patients could not chew. Brachycephaly and Lennox Gastaut were the RDs that showed the worst combined result in these parameters (Table 2).
Toothbrushing was performed twice daily by half of the participants, but 60.9% (39) needed assistance in daily oral hygiene.
The most recurrent toothbrushing difficulties were rinsing correctly (34; 53.1%) and swallowing toothpaste (31; 48.4%) (Table 3). Most of the sample (35; 54.7%) cooperated in oral hygiene, but adjustments were regularly required, namely head control (Table 3).
The total DMFT was 8.73 (±7.60), and filled teeth were the most prevalent (4.66 ± 5.36) (Table 4). The BI-S had a mean score of 1.22 (±0.56), which is equivalent to mild inflammation with slight color change, mild edema, and no bleeding on probing.
The presence of bacterial plaque (DI-S) showed a mean value of 1.62 (±0.76), which represents between 1/3 and 2/3 of the tooth surface covered by soft deposits (Table 4).
Discussion
This study aimed to assess oral health in patients with RDs but not to compare them, as all have different characteristics.
Thus, it intended to provide an overview of the particularities of this population’s oral health conditions, oral habits, and difficulties in oral hygiene.
Although some studies have addressed oral diseases in specific RDs, there is scarce literature on national and international research comprising people with RDs’ difficulties in daily oral hygiene and oral health status. Although not yet considered a global issue, this understanding of oral health in RDs is cumulative.15
In the oral hygiene clinic for PwD, there were 33 different types of RDs in 64 individuals, which shows that RDs are frequente and diverse in this clinic. This finding may derive from FMD-UL having a specific clinic trained for people with disabilities and receiving numerous patients from various regions of the country, which, consequently, entails a wide variety of pathologies, including RDs. The sample’s predominant sex was male, probably because some RDs are typically sex-related, as in the Fragile X syndrome.19
Due to RDs’ characteristics and their carriers’ profound disabilities and special assistance needs, the high level of dependency, the high difficulty in moving around, and the communication difficulties are not surprising. However, no patients with Fragile X and Cornelia de Lange syndromes had movement difficulties in this study. In turn, Angelman syndrome stood out negatively as all patients with this disease were unable to communicate and were dependent. Even so, only one individual with this syndrome followed a liquid or soft diet. The feeding capacity was related to a higher frequency of dental appointments in a study on Rett Syndrome.20 The level of dependency and mobility constraints of individuals with RDs cause greater difficulties in accessing oral hygiene appointments due to the architectural barriers that still exist and oral health professionals’ low capacity and training to provide care to PwD.21
Non-nutritive sucking habits are reportedly frequent in people with disabilities. The same was found in the presente study, as 32.8% of the participants had finger-sucking or pacifier- sucking habits, more prevalent in Rett and Angelman syndromes.
When the habit of non-nutritive sucking persists beyond the age of three, it is considered a harmful oral habit.22 In Rett’s syndrome, the most common parafunctional habit was bruxism and open bite. However, other oral manifestations were found, such as tongue protrusion and finger or pacifier sucking, resulting in an open bite.23
Limitations in motor coordination and parafunctional habits make daily oral hygiene practices, such as toothbrushing and rinsing, challenging.24,25 In the present study, the most recurrent problems were rinsing incorrectly and swallowing toothpaste. These difficulties may contribute to worse oral health status, with a greater susceptibility to dental caries and periodontal disease.25 There is no scientific evidence proving the effectiveness of rinsing, and some studies even recommend not to rinse after brushing when using toothpaste with sodium monofluorophosphate.26 However, because pouching is very common in patients with special needs, this capacity is very important for oral cleaning in these individuals.25 Moreover, the amount of toothpaste placed on the toothbrush should be monitored, as individuals with cognitive or developmental disabilities may have difficulty understanding the concept of swallowing and may inadvertently swallow unwanted materials due to lack of awareness or impulsivity.27
Table 1 Sex, age, mobility, communication, and degree of dependency per rare disease.

S. - Syndrome; AMVG - Arteriovenous malformation of the vein of Galen; AADC - Aromatic l-amino acid decarboxylase; CDG - Congenital disorders of glycosylation
Table 2 Type of diet, type of chewing, and non-nutritive habits per rare disease.

S. - Syndrome; AMVG - Arteriovenous malformation of the vein of Galen; AADC - Aromatic l-amino acid decarboxylase; CDG - Congenital disorders of glycosylation
Table 3 Toothbrushing frequency, toothbrushing difficulties, autonomy in toothbrushing, and cooperation during the appointment per rare disease.
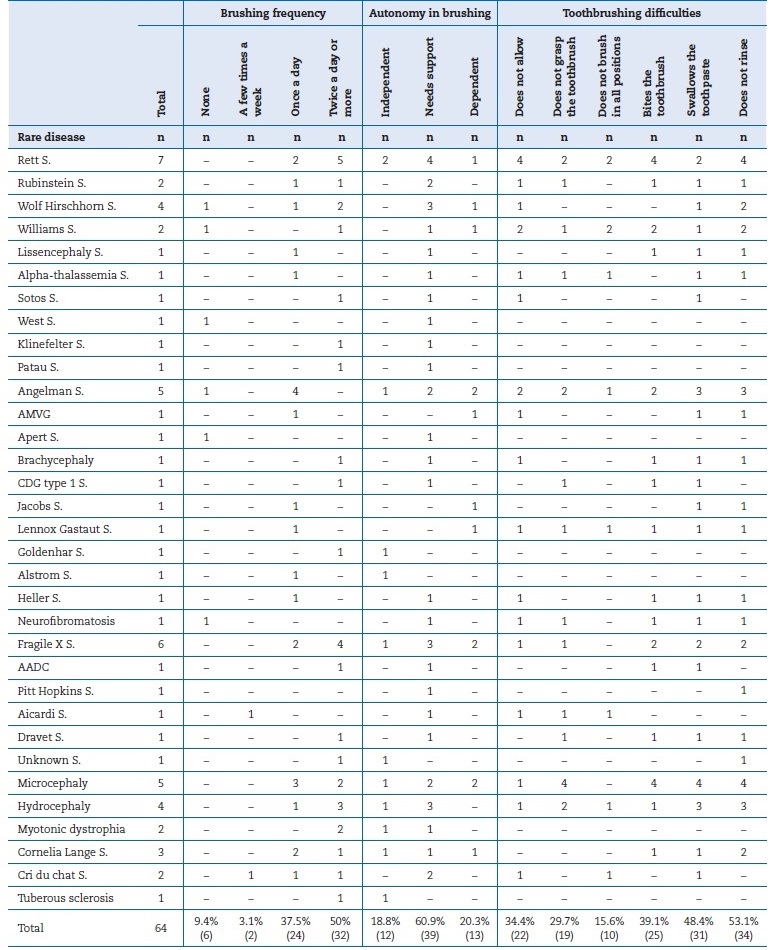
S. - Syndrome; AMVG - Arteriovenous malformation of the vein of Galen; AADC - Aromatic l-amino acid decarboxylase; CDG - Congenital disorders of glycosylation
Table 4 Decayed, Missing, and Filled Teeth index (DMFT), debris index (DI-S), and bleeding index (BI-S) per rare disease.
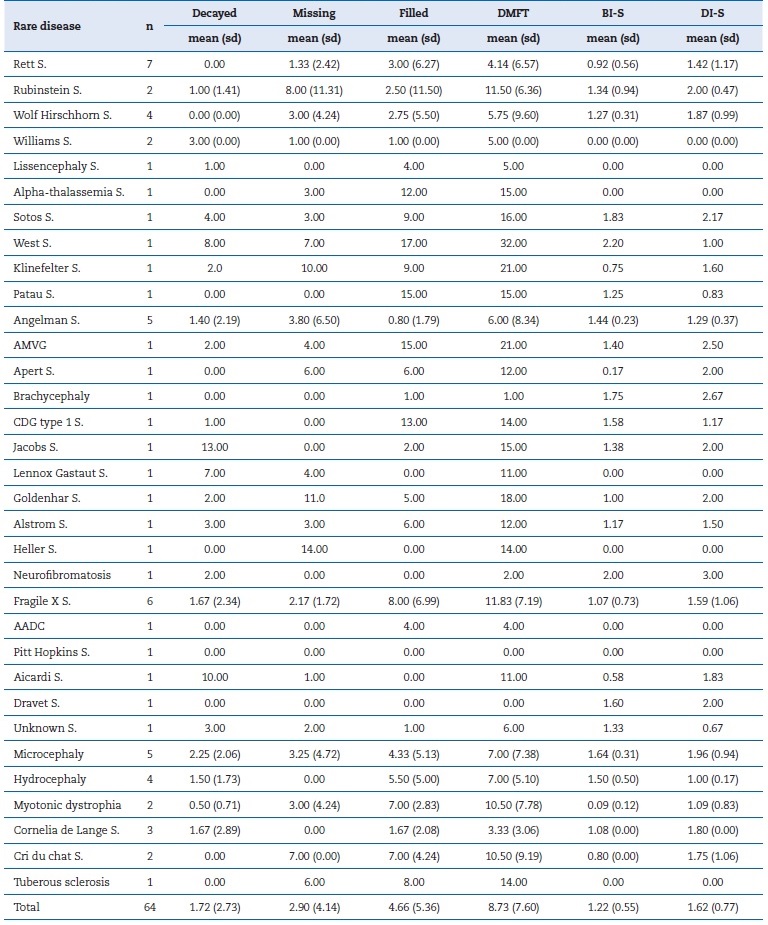
S. - Syndrome; AMVG - Arteriovenous malformation of the vein of Galen; AADC - Aromatic l-amino acid decarboxylase; CDG - Congenital disorders of glycosylation
Besides the difficulty in correctly swallowing, there is difficulty in toothbrushing, associated with the existing motor and intellectual deficits and the oral manifestations of this population, such as malocclusion, tooth agenesis, tooth rotation, and microdontia.24 In this study, most patients needed assistance in performing daily toothbrushing. Namely, all individuals with Cri du Chat syndrome required assistance in toothbrushing, contrary to the finding of a study in which most patients with Cri du Chat brushed their teeth alone, without adult supervision.28 According to the III National Study on the
Prevalence of Oral Diseases in Portugal (ENPDO III)29 in people without RDs, 74.3% brushed their teeth twice daily in the age group 35-44 z, which is a higher prevalence than the one found in the population with RDs in our study (50.0%).
The mean value of DMFT was 8.81 (±7.54), similar to the results in a study carried out in the same clinic in individuals with intellectual disabilities (8.91 ±6.72).30 According to Vettore et al.,25 children and adolescents with RDs have more decayed teeth, dental anomalies, and malocclusion. However, another study showed no higher prevalence of dental caries in patients with RDs.25,31 The mean value of decayed teeth in this study was 1.77 (±2.73), a relatively low value for a population with disabilities and similar to the general population of a similar age (1.63)29 and to the dependent population that attended the special needs clinic at FMD-UL (1.84).32 Individuals with Jacobs syndrome showed the highest value of decayed teeth (13.00), which may result from their poor manual dexterity and hyperdontia.
Individuals with Aicardi syndrome had the next highest value, 10 decayed teeth; the literature describes patients with this syndrome as having a greater tendency to develop caries and gingivitis, associated with malocclusion and deficiente muscle tone.15
The difference in DMFT values between the various studies may be linked to fluoride exposure, sugar-rich diets, and the frequency of visits to the oral health professional.31 In the present study, filled teeth were prevalent (4.47; ±5.35), showing concern about carrying out treatments and seeking good oral health. However, it is important to acknowledge that the presente study was conducted in a clinical setting, which entails several limitations. Individuals attending clinical appointments may differ significantly from those who do not attend appointments as regularly. The distinct sampling characteristics among studies inevitably influence their results and representativeness. In a study on Rett’s syndrome, caries were less significant in those patients compared to the control group,4 which agrees with the present study, where individuals with Rett’s syndrome had a mean value of decayed teeth of zero. According to the literature, bruxism is reported in most of the population with Rett’s syndrome, and this may be related to the low prevalence of dental caries in this population.20
The BI-S showed a medium value equivalent to mild gingival inflammation with a slight alteration in color, light edema, and no bleeding. It was higher in patients with West syndrome (2.20) and neurofibromatosis (2.00).
The DI-S obtained a mean value representing less than 2/3 of the tooth surface covered by soft deposits. However, this index shows the state of oral health solely during the observation and may be variable throughout the day.18 In comparison with another study on intellectual disability,30 the DI-S values are slightly higher, which may be justified by the high level of dependency, both cognitive and motor, of the population with RDs. Similarly, in another study,25 children and adolescentes with RDs tended to have poor oral hygiene and lower standards of dental care than those without rare genetic disorders.
Patients with RDs require specific special care that responds to their real needs, necessitating adaptive strategies. Thus, individualized preventive education and therapies are essential, and each patient’s needs must be considered. In order to promote good oral hygiene practices, it is imperative to provide caregivers with training and support. Given the difficulties and characteristics of these patients, oral hygiene becomes a difficult process to carry out daily.
Some techniques can be used to facilitate toothbrushing and help caregivers maintain the oral hygiene of these individuals. Head control is one of the most used and successful techniques in RD individuals since it provides safety and Comfort for both the patient and the caregiver. This method consists of keeping the patient’s head stable, giving the caregiver a better view of the oral cavity. This technique can be particularly helpful for individuals with poor motor skills or coordination problems. In cases where the individual with an RD has motor difficulties, coordination problems, or lack of cooperation, the limb control technique can help ensure that the individual remains still during the procedure. This technique can be done using support devices, such as support bands, which help keep the individual’s arms secure. Using the bite block is also a common technique during oral hygiene in people with RDs and can be used in individuals who bite the toothbrush.
As seen in this study, RDs are characterized by several oral conditions that vary not only among different diseases but also among patients with the same RD. This diversity represents an obstacle to characterizing oral conditions typical of each RD, requiring more extensive studies. Collaboration of oral health professionals in multidisciplinary teams may be one way to improve the diagnosis and treatment of patients with RDs.
This study relies on a convenience sample, which may introduce bias in the selection of participants. The sample included patients from a clinic at FMD-UL; therefore, the sample was particularly concerned about their oral health. The non-random nature of the sample may compromise the generalizability of the results to the population with disabilities.
However, it contributes to a better understanding of these diseases.
Conclusions
The study showed that each RD has its own oral characteristics, which distinguish them from each other and require a comprehensive study. The specific behavioral difficulties in this population make daily oral hygiene and visits to the dental office more challenging. The oral health professional must have a broad knowledge of the needs of each RD and the most suitable adaptations. Despite the inherent limitations of this population, the mean number of decayed teeth was reasonable, and the mean number of filled teeth was high, showing that this population is concerned with treatment and seeks good oral health.















