Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.9 no.5 Coimbra dez. 2015
CASE REPORT/CASO CLÍNICO
Obstetric outcomes after radical trachelectomy in a series of four pregnancies
Desfechos obstétricos pós-traquelectomia radical numa série de quatro gestações
Joana Goulão Barros*, Inês Pereira*, Mónica Centeno**, Luísa Pinto**, Luís M. Graça***
Departamento de Obstetrícia, Ginecologia e Medicina da Reprodução, Hospital Universitário de Santa Maria, CHLN
*Internas do Internato Complementar em Obstetrícia e Ginecologia
**Assistente Hospitalar de Obstetrícia e Ginecologia
***Director de Serviço de Obstetrícia e Ginecologia e Professor Catedrático
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Vaginal radical trachelectomy has been established as a valuable fertility-preserving treatment in women with early stage cervical cancer. Pregnancies after this procedure may pose several clinical challenges. The aim of this study was to report pregnancy outcomes after vaginal radical trachelectomy.
We surveilled four pregnancies in three different patients. No first trimester miscarriages were observed. One of the patients suffered a second trimester pregnancy loss as a consequence of a preterm premature rupture of membranes. A total of three pregnancies reached the third trimester, and one delivered prematurely, at 29 weeks of gestation. A caesarean section was performed in all cases that reached viability.
Good maternal and neonatal outcomes are possible in pregnancies after radical trachelectomy. Obstetrical surveillance must be undertaken in a maternal-fetal unit included in a tertiary hospital, in order to achieve the best results.
Keywords: Pregnancy; Vaginal trachelectomy.
Introduction
Cervical cancer is one of the most common cancers affecting women of childbearing age, with up to 42% of cases being diagnosed in women prior to the age of 451.
The traditional treatment for cervical cancer – radical surgery and/or chemoradiation therapy – does not allow the preservation of a functional utero-ovarian system for reproductive purposes.
In countries where cervical cancer screening programs are in place, a significant proportion of cervical cancer is diagnosed at an early stage, making radical traquelectomy an accepted therapeutic option in women who want to preserve fertility2.
Traquelectomy is a procedure first described by the French gynaecologist Daniel Dargent in 1987, which is indicated for early stage cervical carcinoma (FIGO stage IA1/IB1, with less than 2 cm)3,4. It is a locally radical surgery that allows preservation of the body of the uterus, making childbearing possible at the expense of an increased risk of second-trimester abortion, premature preterm rupture of membranes and preterm delivery in a subsequent pregnancy5,6. The results reported over the last two decades have confirmed a cancer recurrence rate of less than 5%, with promising fertility and obstetrical outcomes7. Nevertheless, the obstetrical management of these patients has not been formally addressed, and some concerns have been raised regarding pregnancy surveillance in this population5,8.
In this study, we analyze the pregnancy outcomes of women who underwent radical vaginal traquelectomy, and whose subsequent pregnancies were surveilled at our maternal-fetal unit.
Case report
We performed a retrospective review and analysis of clinical data concerning four pregnancies in three different women admitted to our maternal-fetal unit over a four-year period (from January 2008 to January of 2012), who had previously been submitted to a radical vaginal trachelectomy. We obtained written informed consent from all the participants.
All patients had a previous diagnosis of invasive cervical cancer stage IB1 according to the International Federation of Gynecology and Obstetrics (FIGO) classification4 and wanted to preserve fertility. They were submitted to a vaginal radical trachelectomy and laparoscopic lymphadenectomy at the Centre Oscar Lambert in Lille, France. This procedure includes placing a cervical cerclage with a monofilament non-absorbable suture.
The patients were referred to our maternal-fetal unit during early pregnancy.
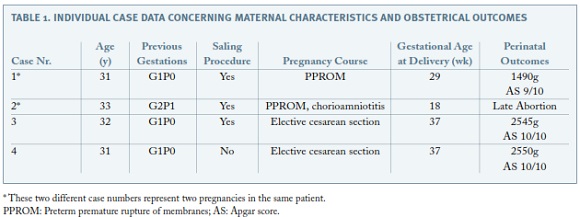
A description of the four cases is presented in Table I.
All three patients were nulliparous and one had a second pregnancy during this 4-year period.
We did not observe any first trimester miscarriage. One of the patients had a second trimester pregnancy loss, at 18 weeks of gestation, after preterm premature rupture of membranes (PPROM) with subsequent chorioamnionitis. At this point, antibiotic therapy was initiated and a vaginal uterine evacuation was performed 12 hours later, under general anesthesia, after cutting the cervical cerclage and performing digital dilation of the cervix. The patient was discharged three days after the procedure without any complication. This same patient had already suffered a preterm premature rupture of membranes in the previous pregnancy at 29 weeks.
Three pregnancies reached the third trimester, although one delivered prematurely, at 29 weeks of gestation, as previously referred. Two of the four pregnancies were delivered at term.
At early second trimester the cervix was measured by vaginal ultrasound, and the patients were submitted to a Saling procedure at 14 weeks of gestation if the cervix length was less than 15 mm. The Saling procedure was performed in another hospital in the same city, and consisted on removing part of the superficial epithelium of the cervix and proximal vagina and stitching it over the cervix obtaining a cervical occlusion in order to prevent infection. All Saling procedures were performed under loco-regional anesthesia. This procedure was performed in three pregnancies around the 14th week of gestation. Two of the procedures were performed in the same patient in consecutive pregnancies. In one patient this procedure was not considered necessary as the cervix length was 15 mm.
Betamethasone was administrated to all women for fetal lung maturation (two administrations of 12 mg with a 24 hour interval) between 26 and 30 weeks of gestation, due to the known risk of preterm delivery.
Only one patient needed tocolytic therapy due to preterm contractions, and nifedipine 10 mg every 6 hours orally was prescribed, from the 26th week of gestation till 29th week, when preterm premature rupture of membranes occurred.
A caesarean section was performed to all women who reached the third trimester, no longer than 37 weeks, with repermeabilization of the cervical canal by digital dilation in all cases submitted to Saling procedure. No perioperative complications were registered.
There were no neonatal deaths. The premature newborn was admitted to the Neonatal Intensive Care Unit and was discharged at day 44.
Discussion
Obstetric surveillance of women previously submitted to radical trachelectomy poses several challenges to the obstetrician, with clinical management being usually empirical rather than evidence-based. There is evidence that these pregnancies entail a higher risk of adverse perinatal outcomes 9-12.
The most common complications associated with pregnancy after trachelectomy are preterm labor, premature preterm rupture of membranes, and second trimester pregnancy loss, which are in line with our findings6,9,10. Notwithstanding, a recent study7 reports obstetric results that are considerably more favorable than previously reported ones9,10, with a rate of second trimester pregnancy loss and significant prematurity (less than 32 weeks) of 3% and 4%, respectively. As the authors state, this discrepancy might be related to differences in the length of the remaining cervix. In our study, 2 out of 4 pregnancies were complicated with PPROM, and this situation occurred in the same patient, in both pregnancies. This patient had a cervical length inferior to 15 mm at 14 weeks of gestation. Thus, differences in cervical length might be in the core of this issue.
Performing a Saling procedure is controversial. It has been advocated as a cervical occlusion, in order to prevent ascending infection and subsequent chorioamnionitis. These patients are more prone to infection due to the presence of a cerclage with a monofilament non-absorbable suture, placed during the trachelectomy procedure in a neo-cervix not protected by a cervical mucus plug10,11. In agreement with the surgeon who performed the trachelectomies, we only advised a Saling procedure if the cervical length was inferior to 15 mm at 14 weeks of gestation. In 3 of the 4 pregnancies, a Saling procedure was performed, with only 1 of these 3 pregnancies reaching term. This might be related to the fact that these pregnancies encompassed a greater risk a priori, due to a shorter cervix, and these findings are emphasized by the fact that the only patient who did not have an indication for a Saling procedure, reached term. We did not observe any complications directly related to the Saling procedure. Nonetheless, this procedure should only be performed when indicated.
The uterine evacuation that followed the 2nd trimester abortion was mandatory, because after the procedure of trachelectomy, the cervix becomes incapable of dilation, so it is necessary to dilate the cervix mechanically and then perform the vaginal uterine evacuation.
Given the high risk of preterm birth, all patients received corticosteroids for induction of fetal lung maturation, although this is not a universally recommended practice7.
After a trachelectomy, delivery should be performed by cesarean section, since a vaginal delivery would comprise multiple risks in view of the presence of a short-scarred cervix and of the proximity of the uterine vessels7. For these reasons, it has been advised to schedule an elective cesarean at 37-38 weeks of gestation, in an attempt to avoid spontaneous labor7. The cesarean technique has also been the subject of discussion, with some authors recommending a low-transverse uterine incision and others favoring the longitudinal midline incision, due to the potential risk of transverse incision extending into the uterine vessels6,7. In our study, all cesarean sections were performed using a low-transverse incision and we did not observe any complications.
Preservation of childbearing function, by means of a trachelectomy, is a great possibility for patients with early-stage cervical cancer. It is necessary that all clinicians are aware of this procedure and its consequences, mostly regarding a subsequent pregnancy, even if it is not performed in their centers. Once pregnant, these patients should be closely surveilled. However, there are no clear guidelines regarding this antenatal surveillance. Given the high risk for preterm delivery, we advise that obstetrical management should be undertaken in a fetal-maternal unit included in a tertiary hospital, in order to achieve the best outcome. There are still several issues concerning perinatal and intrapartum care lacking clarification, such as bed rest and sexual intercourse during pregnancy, prophylactic corticosteroids for fetal lung maturation and the cesarean section technique. These and other issues remain unsolved and are challenging subjects for further research.
REFERENCES
1. SEER Stat fact sheet: cervix uteri cancer. National Cancer Institute. http://seer.cancer.gov/statfacts/html/cervix.html Published 2012. Accessed February 10, 2013. [ Links ]
2. Wong I, Justin W, Gangooly S, Sabatini L, Al-Shawaf T, Davis C et al. Assisted conception following radical trachelectomy. Hum Reprod 2009;24(4):876-879. [ Links ]
3. Dargent D, Brun JL, Roy M. La trachélectomie élargie (TE): une alternative à l’hystérectomie radicale dans le traitment des cancers infiltrants développés sur la face externe du col utérin. J Obstet Gynecol 1994;2:292-295. [ Links ]
4. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix and endometrium. Int J Gynecol Obstet 2009;105:103—104. [ Links ]
5. Bernardini M, Barrett J, Seaward G, Covens A. Pregnancy outcomes in patients after radical trachelectomy. Am J Obstet Gynecol 2003;189(5):1378-1382. [ Links ]
6. Sheperd J, Spencer C, Herod J, Ind T. Radical vaginal trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer – cumulative pregnancy rate in a series of 123 women. BJOG 2006;113(6):719-724. [ Links ]
7. Plante M, Gregoire J, Renaud MC, Roy M. The vaginal radical trachelectomy: an update of a series of 125 cases and 106 pregnancies. Gynecol Oncol 2011;121(2):290-297. [ Links ]
8. Plante M, Renaud MC, Hoskins IA, Roy M. Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancies and review of the literature. Gynecol Oncol 2005;98(1):3-10. [ Links ]
9. Jolley JA, Battista L, Wing DA. Management of pregnancy after radical trachelectomy: case reports and systematic review of the literature. Am J Perinatol 2007;24(9):531-539. [ Links ]
10. Boss EA, van Golde RJ, Beerendonk CC, Massuger LF. Pregnancy after radical trachelectomy: a real option? Gynecol Oncol 2005;99(3 Suppl 1):S152-156. [ Links ]
11. Ishioka S, Endo T, Hayashi T, Baba T, Umemura K, Saito T. Pregnancy-related complications after vaginal radical trachelectomy for early-stage invasive uterine cervical cancer. Int J Clin Oncol 2007;12(5):350-355. [ Links ]
12. Speiser D, Mangler M, Kohler C, Hasenbein K, Hertel H, Chiantera V, et al. Fertility outcome after radical vaginal trachelectomy: a prospective study of 212 patients. Int J Gynecol Cancer 2011;21(9):1635-1639. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Joana Goulão Bravo
Serviço de Obstetrícia e Ginecologia
Hospital Universitário de Santa Maria
Avenida Prof. Egas Moniz
1649-035 Lisboa
E-mail: joanagmb@gmail.com
Recebido em: 30-06-2014
Aceite para publicação: 23-10-2014