Introduction
Epidural analgesia is frequently used for labour analgesia, usually without complications. Epidural abscess is a rare but potentially devastating complication, that can result in important neurological morbidity and death1. Its incidence is unknown, but low. In a series of 17.372 epidural catheter insertions, 9 cases were reported (incidence of 0.052%)2. Evidence on this topic is sparse, with very few published cases in the last years. In this article, a postpartum epidural abscess is described, and the need of timely diagnosis and treatment to prevent permanent neurologic damage and death is emphasized.
An informed consent was obtained from the patient prior to the elaboration of this article.
Clinical case
A healthy 30-year-old woman was submitted to a caesarean section for non-reassuring foetal status and foetal growth restriction, under epidural anaesthesia. The immediate postpartum period had no complications, and the patient was discharged after 72 hours.
On the 12th postoperative day, the patient went to the emergency room with a several-day left iliac fossa and lumbar pain, that irradiated to the left lower limb with mobilization and on orthostatic position, and did not resolve with oral analgesia. She also had fever since the day before. On admission, she was apyretic, normotensive but tachycardic. The puerperal exam was normal, and the surgical wound did not have inflammatory signs. She presented pain in the lumbosacral and left iliac fossa regions with digital pressure, with no changes in lumbar inspection or palpation, with Lasègue and Bragard positive signs on the left, without neurologic deficits.
The workup showed severe anaemia (haemoglobin 7.2g/dL) and elevated inflammatory markers (leukocytes (22.000 leucócitos/µL) and elevated C reactive protein (268mg/dL)).
An abdominopelvic computed tomography (CT) scan showed a subcutaneous liquid/gaseous collection with 1.5x9.5x4.5cm in the site of the surgical incision, whose percutaneous needle puncture revealed serohematic fluid. The lumbar CT scan showed a 26mm hypodense L3-L4 lesion, with a probable epidural location and dural sac deformation, which could represent a hematoma or an abscess, requiring better characterization by magnetic resonance (MR).
In the following hours, the patient presented with sustained fever and lumbar pain under analgesia, and posteriorly developed urinary retention needing catheterization, defecatory difficulty and limited gait caused by diminished left lower limb strength.
The lumbar MR confirmed a 3cm epidural abscess, which exerted an important mass effect on the dural sac (Figure 1). Given the spinal cord compression and cauda equina syndrome, the patient was submitted to an urgent laminectomy and abscess drainage.
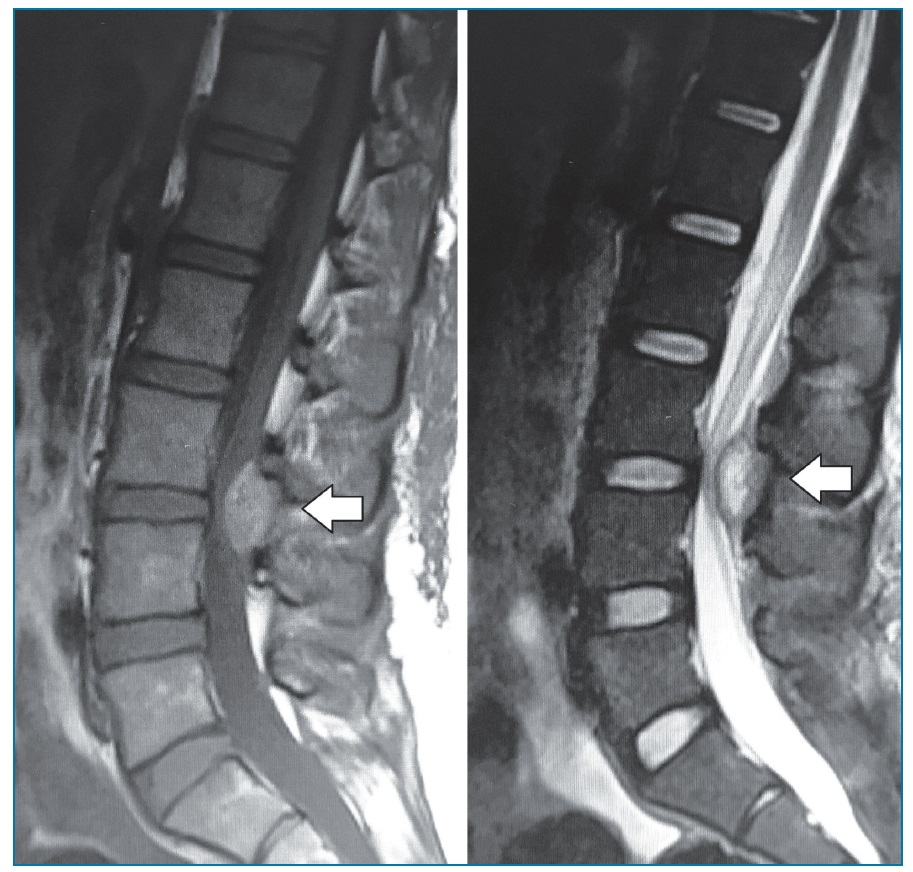
Figure 1 Median sagittal view on MRI (T1 -weighted on the left and T2 -weighted on the right) showed a 27mm fluid collection at disc level L3 -L4, compressing the dural sac (white arrow).
She completed 15 days of intravenous antibiotic therapy, initially empiric with ceftriaxone and vancomycin and posteriorly changed to flucloxacillin after methicillin-sensitive Staphylococcus aureus (MSSA) isolation.
There were no complications in the post-operative period. The patient was apyretic and without sensitive or motor function deficits. A follow-up lumbar RM a week later showed little inflammation signs compatible with the post-operative period. She was discharged 15 days after surgery and completed two additional weeks of antibiotic therapy with oral flucloxacillin. A follow-up lumbar MR a year later showed complete resolution and the patient is without neurologic deficits to date.
Discussion
The incidence of epidural abscess in the postpartum period is unknown, but extremely low, according to the available evidence. A 2015 review article about bacterial infection after epidural catheterization included only 5 cases of epidural abscess in the postpartum period3.
Studies suggest that the risk of infectious complications after epidural catheterization is variable, depending on the presence of predisposing factors, namely the duration of the catheterization, with a period higher than 3 days being considered a risk factor2. In the Xue et al. review mentioned before, the duration of catheterization varied between 6 and 48 hours3. There was just one case, described in 2004 by Schroeder et al. where the epidural catheter was kept by a short period (6h), the only one less than 24 hours4. The catheterization technique itself, along with correct skin disinfection and aseptic conditions are also factors that could influence the rate of infection.
Other risk factors, such as advanced age, immunodepression, diabetes mellitus or oncological disease could raise the risk. In the present case, the patient was healthy and the epidural catheter was in place for about 30 hours.
Epidural space infection is specially associated to the catheter insertion moment. The most commonly isolated microorganisms are Staphylococcus aureus and epidermis, in about 2/3 of the cases, followed by Streptococcus and gram-negative bacteria, in a lower percentage. In up to 15% of abscesses, it is not possible to identify the causative microorganism1,2. In the presented case, a methicillin sensitive Staphylococcus aureus was isolated.
Lumbar pain is the most frequent reported symptom, in up to 90% of cases5. In the Xue et al. review, all patients reported this symptom. The same happened with our patient. However, the lumbar pain incidence in the postpartum period is high, regardless of the type of labour analgesia that was used. Therefore, without other associated symptoms, namely neurological deficits or fever, it is extremely difficult to diagnose an epidural abscess. Our patient presented with lumbar pain for several days, and fever and the progressive neurological deficits, along with infection markers, appeared only 10 days after the caesarean section, and these symptoms were not present on admission to the emergency room.
Imaging is crucial to the confirmation of the diagnosis, the MRI being the most sensible imaging technique, as it was in the presented case, given the CT scan did not allow a definitive diagnosis6. The conservative treatment can be considered when there are no neurologic deficits7. In the Xue et al. review, only 2 out of 5 patients needed surgical intervention3. If neurologic damage is suspected, with spinal cord compression, as in the presented case, the risk of permanent damage or eventually death is high, therefore urgent surgical treatment with decompression and drainage is inevitable.
In all cases, antibiotic therapy is imperative. It should be started as soon as the diagnosis is suspected, initially empiric and posteriorly adjusted to the causative agent1. Although there are not randomized controlled trials evaluating antibiotic regimens for the treatment of epidural abscess, the recommended empiric regimens include antibiotics active against the most commonly isolated pathogens (exposed before in this article), being the first line vancomycin plus ceftriaxone or cefotaxime. Other cephalosporins such as cefepime or ceftazidime, or meropenem could be options in the suspicion of Pseudomonas aeruginosa, or in patients in the intensive care unit or risk factors such as diabetes mellitus. In the presented case, the patient (who did not present additional comorbidities) was prescribed therapy with vancomycin plus ceftriaxone until the identification of the causal agent. Once this is isolated, the treatment should be simplified and directed to the specific pathogen. For methicillin-resistant Staphylococcus aureus infections, vancomycin should be continued; on the contrary, for MSSA infections, the therapy should be changed to narrow-spectrum beta-lactam antibiotics such as oxacillin. In this case, therapy was changed to flucloxacillin, according to the antibiotic sensitivity tests and Infectious Diseases’ orientations. The appropriate duration of antimicrobial therapy is not known, but is generally recommended 4 to 6 weeks. Our patient completed a total 4 weeks of antibiotic therapy, 2 of which after hospital discharge1.
A follow-up imaging technique (MR) must be done 4 to 6 weeks to show complete resolution if the patient is improving1. Our patient was submitted to a post--operative MR only one week after surgery, which might have been precocious, since it can show some inflammatory alterations in result of the recent surgical procedure.
In conclusion, epidural abscess is a major complication of epidural anaesthesia, and although rare, can have an important impact on neurologic integrity. The clinical manifestations are unspecific, turning the diagnosis a challenge, particularly in healthy patients with no additional risk factors or comorbidities. Therefore, it is necessary to have a high degree of suspicion and consider every possibility, including complications of recent medical interventions, since timely diagnosis and treatment are crucial to prevent permanent neurologic damage and death.














