Introduction
Ectopic pregnancies concern all pregnancies that occur outside the uterine cavity. Its incidence is rising, comprising approximately 1-2% of all pregnancies, of which 98% occur within the fallopian tubes. Other less common locations include the tubal interstitial segment, cervix, peritoneal cavity, cesarean scar and ovary, with the latter having an estimated incidence of 1 in 2100 to 1 in 7000 pregnancies, meaning ~3% of all ectopic pregnancies1.
Common risk factors include previous tubal surgery, infertility and assisted reproductive technologies, intrauterine device placement, tobacco use, endometriosis and pelvic inflammatory disease2.
On presentation, most women complain of lower abdominal pain and scarce vaginal bleeding.
Diagnosis is usually made after determination of ß-hCG levels and visualization of embryonic structures outside the uterus or an empty uterine cavity associated with raised ß-hCG3.
Case report
A 35 year-old healthy primiparous woman presented to the emergency with scant vaginal bleeding and 4 weeks and 6 days of amenorrhea. She had no history of previous surgeries or infertility treatments and was medicated with folic acid.
The serum ß-hCG value 3 days earlier was 24,380 U/L (reference value <5 U/L).
Vaginal inspection revealed moderate bleeding through the external cervical os and bimanual palpation was painless and no masses were identified.
An ultrasound was performed and a gestational sac with 38x33 mm with an embryo without heartbeat was seen on the right adnexal area (Figure 1). A corpus luteum was identified in the ipsilateral ovary. The uterus was empty with a 5 mm endometrial line and no fluid was present on the pouch of Douglas.
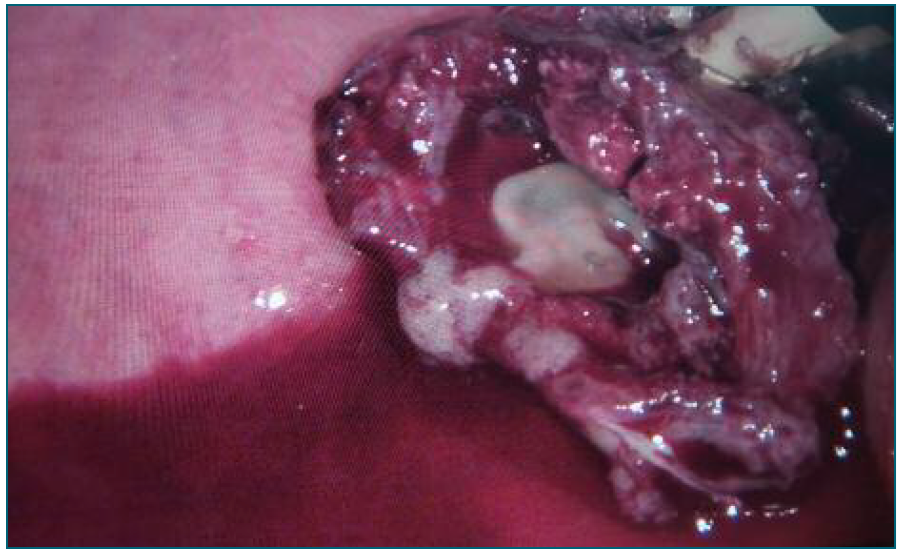
An exploratory laparoscopy was indicated, where an enlarged violaceous ovary with a heterogeneous 4 cm mass was visualized and a small amount of blood on the posterior coul-de-sac was found. (Figure 2)
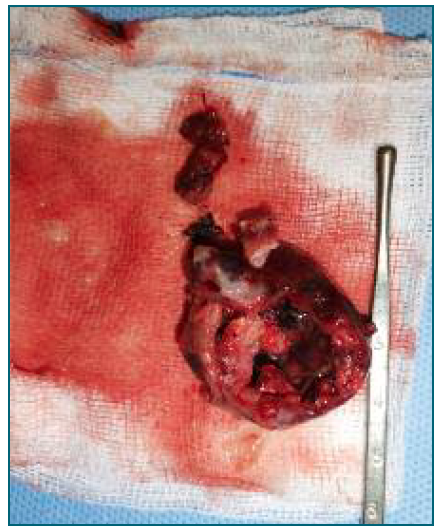
An attempt was made to preserve the remaining ovarian tissue, so only the lesion was removed and sent to pathology. Histological analysis confirmed the findings, reporting an ectopic ovarian pregnancy (Figure 3).
The woman was discharged 2 days after surgery wi-thout any complications.
Discussion
Ovarian pregnancies consist in a rare form of ectopic pregnancy which develop partially or completely inside the ovarian parenchyma. Most cases occur in the ovary ipsilateral to the corpus luteum, when the fertilized egg is retained in the ovary.
Its pathophysiology is thought to be the result of failure in follicular extrusion after ovulation or secondary implantation of the pregnancy in the ovary after fertilization inside the fallopian tube.
A high level of suspicion is needed for its diagnosis and often can only be done after visualization of the adnexal structures during surgery. Ultrasound findings are nonspecific and may resemble the ones found in tubal pregnancies, especially in advanced stages or ruptured pregnancies. When a small gestational sac is present inside the ovary, it might be mistaken for a corpus luteum, despite trophoblastic tissue being more echogenic.
In the presented case, the exact pregnancy location could only be determined during surgery, after laparoscopic visualization of an intact tube and ovarian mass, which was later confirmed through histological report of an ovarian pregnancy.
Treatment options include medical treatment with methotrexate and surgical excision of the pregnancy, through ovarian wedge resection, whenever possible, or complete oophorectomy. The implications in future pregnancies are more severe in oophorectomy, especially when the contralateral ovary is already compromised. In this case, no subsequent pregnancy was yet desired by the woman, so implications cannot yet be assessed.
The case presented serves to illustrate the difficulty in localizing ectopic pregnancies and the importance of timely treatment, regarding maternal morbidity and future fertility.
Authors’ contributions
Ana Filipa Maia - wrote the article and assisted the surgery.
Mariana Solinho - co-author, helped reporting the case.
Ana Sofia Domingos - co-author, helped reporting the case.
Catarina Inácio - co-author, helped reporting the case.
Margarida Estrela - co-author, made the diagnosis and was the main surgeon, helped writing and reviewed the article.