Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.16 no.3 Lisboa set. 2020
EDITORIAL
Adaptações no serviço de cirurgia vascular do CHULN durante a pandemia de COVID-19 e impacto na atividade global
Adaptations in the vascular surgery department of the CHULN during the COVID-19 pandemic and impact on overall activity
António Duarte1, Ryan Melo1, Alice Lopes1, João Rato1, Marta Rodrigues1, Mickael Henriques1, Miguel Gomes1, Vanda Pinto1, Karla Ribeiro1, Emanuel Silva1, Mariana Moutinho1, Pedro Garrido1, Viviana Manuel1, Augusto Ministro1, Gonçalo Sobrinho1, Luís Silvestre1, Pedro Amorim1, Ruy Fernandes1, Nuno Meireles1, Carlos Martins1 e Luís Mendes Pedro1
1Serviço de Cirurgia Vascular, Departamento de Coração e Vasos, Centro Hospitalar Universitário Lisboa Norte (CHULN), Lisboa, Portugal. Faculdade de Medicina da Universidade de Lisboa, Portugal. Centro Académico de Medicina de Lisboa
Endereço para correspondência | Dirección para correspondencia | Correspondence
RESUMO
Com o surgir da pandemia a SARS-CoV-2 no início de 2020, os serviços de saúde sofreram várias adaptações de forma a mitigar e controlar a progressão do surto a nível europeu e nacional. Estes ajustes repercutiram-se inevitavelmente na dinâmica da maioria dos serviços hospitalares, nomeadamente no nosso serviço de Cirurgia Vascular. Perante a previsível chegada de uma segunda vaga na Europa e em Portugal, com desfechos e repercussões imprevisíveis nos serviços de saúde, é fundamental aprender com as experiências anteriores e partilhar estratégias para prestar o melhor cuidado aos nossos doentes, apesar das restrições impostas pela pandemia. Através deste artigo, analisamos as adaptações no Centro Hospitalar Universitário Lisboa Norte para superar a pandemia e, em particular, no serviço de cirurgia vascular. Avaliamos ainda o impacto dessas mudanças na nossa atividade global, em comparação com a experiência vivenciada noutros centros nacionais e internacionais. Perante uma segunda vaga iminente, é crucial tirar lições desta pandemia por forma a evitar uma potencial crise na saúde.
Palavras-chave: COVID-19; pandemia; cirurgia vascular; surto; SARS-CoV-2
ABSTRACT
With the onset of the SARS-CoV-2 pandemic in early 2020, health services and personnel adapted their resources to mitigate and control the outbreak. These needs inevitably led to adaptations in most medical and surgical departments, including in our Vascular Surgery department. As we are facing a second outbreak of this pandemic, with unpredictable outcomes and repercussions in health services, it is crucial to learn from previous experiences and share strategies to perform the best care to our patients, despite the restrictions that have been imposed. Through this paper, we review the adaptations in Centro Hospitalar Universitário Lisboa Norte and particularly in our department to overcome the pandemic. We also assess the impact of these changes in our activity and compare with the experience of other fellow surgeons. With an upcoming second outbreak, it is crucial to learn from this and other departments’ experiences to overcome a potential health crisis.
Keywords: COVID-19; Pandemic; vascular surgery; outbreak; SARS-CoV-2
Introduction
A novel respiratory virus outbreak spread from the province of Wuhan, China in early 2020.(1)
With the onset of the SARS-CoV-2 pandemic, health services and personnel focused their efforts and resources on mitigating the outbreak and controlling the spread of cases. These needs inevitably led to adaptations in most medical and surgical departments, including in our Service of Vascular Surgery.(2)
As we are facing a second outbreak of this pandemic, with unpredictable outcomes and repercussions in health systems, it is crucial to learn from previous experiences and share strategies to perform the best care to our patients, despite the restrictions that have been imposed.
The aim of this paper is to report the impact of the COVID-19 pandemic in the surgical setup and activity of our Vascular Surgery department.
How did the Centro Hospitalar Universitário Lisboa Norte (CHULN) react to the COVID-19 pandemic?
In March 2020, Portuguese health authorities issued a series of recommendations for personnel and resources’ reorganization. These adaptations were mirrored by the CHULN administrative board. First, all personnel were allocated to contingency groups, should there be a need for more professionals in the frontline. Furthermore, residents in training programs in other departments were called back to their native services. However, residents working in COVID-19 units and ICU facilities continued their internships to respond to the outbreak. COVID-19 and COVID-19 free circuits were created to cope with inpatient admissions and the Gynecology operating room was converted for surgical procedures to SARS-CoV-2 positive patients or urgent patients awaiting result. Patients were admitted for the shortest period necessary and immediately discharged if no further treatment was needed. Visits to inpatients were suppressed to avoid cross-infection from the visitors. All patients solely awaiting complementary exams were also discharged. Lastly, presential outpatient visits were reduced, with priority to urgent cases and strictly necessary acts. Physicians were encouraged to perform non-presential visits for most patients.
How did our Vascular Surgery department react to the COVID-19 pandemic?
In our department, the medical staff received training in personal protection equipment wearing in the event of a local outbreak and some doctors had also a basic ICU training. Our medical staff was divided in two separate teams. Each team performed presential work every two weeks under all safety precautions in order to reduce virus transmission across our personnel. In addition to this reorganization, one resident was reallocated to a COVID-19 specific ward and one senior assistant stayed at home, according to a decision from the Head of the Vascular Department. Furthermore, 6 members of our nurse personnel were reallocated to other units, including COVID-specific wards. All 6 members served as leaders in their respective teams. Additionally, our wards were converted into COVID-specific ICU units and our patients were admitted in the Cardiology and Cardiothoracic Departments, leading to a decrease in our total capacity.
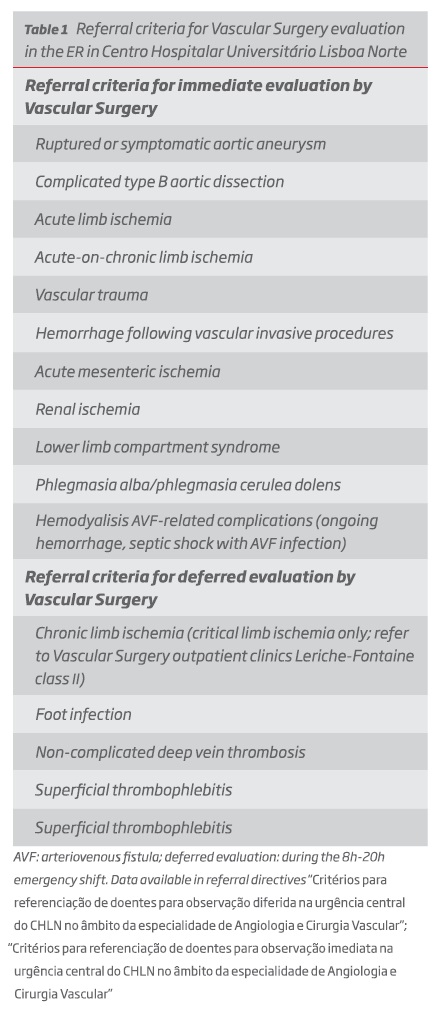
We also created a referral guide for vascular emergencies during night shifts (table 1). All medical and nurse members fulfilled all safety and protection recommendations. So far, we reported no positive SARS-CoV-2 case in our department.
The Vascular Surgery activity during the pandemic first outbreak.
According to the Portuguese Medical Association recommendations for the COVID-19 pandemic, all non-emergent surgical activity was suppressed or reduced.
All the emergent surgical activity was maintained in the central emergency theatre. However, as the availability of the elective OR for non-emergent cases was markedly reduced, we focused on urgent cases, namely symptomatic carotid stenosis, abdominal aortic aneurysms with diameter higher than 5,5cm and chronic limb-threatening ischemia patients with a high risk of amputation.(2) Moreover, we performed more endovascular surgeries with the collaboration of the Radiology department and used more frequently percutaneous accesses and local or locoregional anesthesia. This strategy was found to be beneficial because of a lesser risk of aerosol-generating procedures and cross-infection, as well as the possibility of more blood preservation.(3)
This prioritization strategy was also adopted by departments in other countries highly affected by the pandemic and reported in the literature. In Italy, Pini and colleagues focused on emergency and acute surgical cases while maintaining the same standard of care and safety for their patients.(4) In Turkey, Ünal and colleagues defined a group of 4 levels of priority to distinguish emergent and urgent cases from deferrable surgeries, hence improving the decision-making process in their clinical practice.(3)
In our department, similarly to other groups, all patients, whether elective or urgent, were tested for SARS-CoV-2. Patients deemed of greater emergency were assumed to be SARS-CoV-2 positive and submitted to surgery in a COVID-specific operating room.(2)
Overall, during the first pandemic outbreak, we reported a relative increase in the number of elective admissions while the number of emergency episodes significantly decreased. This reduction may be explained by a fear of going to the hospital and contracting a SARS-CoV-2 infection. Indeed, Rausei and colleagues reported a 45% decrease in the number of emergency surgical admissions in one of the most affected zones by the pandemic in Italy. The authors relate these outcomes to a fear to reach the ER to avoid infection, as well as a result of the confinement measures.(5,6) A similar conclusion regarding emergency admissions was drawn in a publication from a major hospital in Oporto.(7) Nevertheless, contrary to their experience, we did not observe a higher decrease in elective arterial surgery.
Regarding outpatient clinics, we performed less than 50% of the average number of episodes between February and June 2018 and 2019. Additionally, we started performing non-presential acts. We performed significantly more consults via phone calls, predominantly for follow-up appointments. This adaptation was a direct consequence of the confinement period and the rise of telemedicine clinical acts. Similar strategies were adopted in other European countries, such as Ireland.(8) A case report from an American health system reported a sharp rise in telemedicine visits close to 700%.(9) Contrary to the authors’ experience, who performed telemedicine visits both for emergency and elective cases, we maintained presential visits for urgent and priority cases. Another group in Washington also reported more than 50% of all consults were performed with telemedicine tools, with the general acceptance from their patients.(10)
From February to June 2020, our ward total capacity decreased from 32 to a minimum of 7 hospital beds in April, to 18 in June 2020. Despite the shortage in our ward capacity, the average duration of hospital length of stay was shorter during the COVID-19 pandemic. In a letter to the editor, Farroha observed a similar decrease in the length of stay for patients in a burn center.(11) In our department, we believe this may be explained by a higher rate of less invasive, endovascular procedures and more regular use of percutaneous access, as well as a shorter time from admission to surgery. Furthermore, early discharges were more frequent during this period and patients needing more complex wound care were transferred to another facility within our university center (Hospital Pulido Valente). Consequently, we inevitably admitted more patients with less severe conditions or procedures, and less patients with more complex procedures, with longer lengths of stay. This latter population remains one of our main challenges and concerns for a likely second outbreak of this pandemic.
Despite the decrease in hospital beds and in the number of admissions, our mortality rate did not increase when comparing with previous years. This may be interpreted as a result of the changes in practice and the ability to maintain the best care to our patients with the cooperation of the other Services of the Department (Cardiology and Cardiothoracic Surgery). Nevertheless, we cannot exclude an increase in out-of-hospital mortality during the pandemic. Through the analysis of Portuguese data sets between March and April 2020, Nogueira and colleagues estimated an excess mortality of 2400 to 4000 deaths.(12) According to the authors, this increase cannot be fully accounted to the increase in COVID-19 related deaths and may be related to a decrease in healthcare access and an increase in the severity of non-COVID 19 conditions. We are deeply worried that an unknown number of our patients might be unable to get adequate access to the health system, either through their own fear of coming to the hospital or difficulty in the primary care access and proper timely referral.
Conclusions
The COVID-19 pandemic led to significant changes in hospital care, including in our Vascular Surgery department. Following personnel reallocations and a decrease in hospital beds to respond to the outbreak, we decreased our number of admissions and outpatient visits. Despite these restrictions, we introduced non-presential clinical acts and focused on emergency and priority cases. This allowed us to maintain the best standard of care without an increase in our patients’ in-hospital mortality rate. With an upcoming second outbreak, it is crucial to learn from this and other departments’ experiences to overcome a potential health crisis. Further studies need to assess the true long-term impact of the pandemic on chronic conditions, namely chronic limb-threatening ischemia or aortic aneurysmal disease.
REFERENCES
1. Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak: What we know. International Journal of Infectious Diseases. 2020;94:44-48. DOI: 10.1016/j.ijid.2020.03.004 [ Links ]
2. Gouveia e Melo R, Pedro LM. Vascular surgery department adjustments in the era of the COVID-19 pandemic. Journal of Vascular Surgery. 2020;72(1):375-376. DOI: 10.1016/j.jvs.2020.04.017 [ Links ]
3. Ünal EU, Maviolu HL, 0scan HZ. Vascular surgery in the COVID-19 pandemic. Journal of Vascular Surgery. 2020;72(2):752-754. DOI: 10.1016/j.jvs.2020.04.480 [ Links ]
4. Pini R, Faggioli G, Vacirca A, et al. Is it Possible to Safely Maintain a Regular Vascular Practice During the COVID-19 Pandemic? European Journal of Vascular and Endovascular Surgery. Published online May 2020:S1078588420304469. DOI: 10.1016/j.ejvs.2020.05.024 [ Links ]
5. Rausei S, Ferrara F, Zurleni T, et al. Dramatic decrease of surgical emergencies during COVID-19 outbreak. Journal of Trauma and Acute Care Surgery. 2020;Publish Ahead of Print. DOI: 10.1097/TA.0000000000002923 [ Links ]
6. Mantica G, Riccardi N, Terrone C, Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020;183:40-41. DOI: 10.1016/j.puhe.2020.04.046 [ Links ]
7. Pereira-Neves A, Rocha-Neves J, Cerqueira A, Teixeira J. Management and outcomes of a vascular surgery department with sudden medical staff outbreak of COVID-19. Journal of Vascular Surgery. 2020;72(3):1151. DOI: 10.1016/j.jvs.2020.05.055 [ Links ]
8. Connolly MJ, Ahmed Z, Aly S, et al. The impact of COVID-19 on an Irish vascular unit’s service. Journal of Vascular Surgery. Published online August 2020:S0741521420317699. DOI: 10.1016/j.jvs.2020.07.082 [ Links ]
9. Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. Journal of the American Medical Informatics Association. 2020;27(7):1132-1135. DOI: 10.1093/jamia/ocaa072 [ Links ]
10. Hemingway JF, Singh N, Starnes BW. Emerging practice patterns in vascular surgery during the COVID-19 pandemic. Journal of Vascular Surgery. 2020;72(2):396-402. DOI: 10.1016/j.jvs.2020.04.492 [ Links ]
11. Farroha A. Reduction in length of stay of patients admitted to a regional burn centre during COVID-19 pandemic. Burns. Published online June 2020:S0305417920304137. DOI: 10.1016/j.burns.2020.05.028 [ Links ]
12. Nogueira PJ, De Araújo Nobre M, Nicola PJ, Furtado C, Vaz Carneiro A. Excess Mortality Estimation During the COVID-19 Pandemic: Preliminary Data from Portugal. Acta Med Port. 2020;33(6):376. DOI: 10.20344/amp.13928 [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: Antoniomduarte94@gmail.com (A. Duarte).