Introduction
Iliac artery aneurysms (IAA) are frequently associated with coexisting abdominal aortic aneurysms (15% to 25%).1 Isolated IAAs are less common, with an incidence rate ranging from 0.4-1.9 % of intra-abdominal aneurysms.2
Most isolated IAAs are asymptomatic and are detected incidentally on imaging studies performed for other indications. In rare cases, patients present with rupture, distal embolization, thrombosis, and symptoms of visceral or neurologic compression.2
The natural history and treatment outcomes of IAA are poorly understood due to their low incidence. The current consensus is that elective repair should be considered in low-risk patients for IAAs greater than 3.5 or 4cm in maximal transverse diameter.3,4
Treatment of IAA has evolved significantly in the last decades, and nowadays, there is a variety of open surgical (OS), endovascular treatment (ET), and hybrid options. The traditional OS for common or external iliac artery aneurysms is graft interposition with internal iliac artery aneurysm ligation if necessary. Regarding ET, treatment options evolved from common or external iliac artery aneurysm exclusion with stent grafting and internal iliac artery aneurysm occlusion with coil embolization to several more complex strategies to preserve internal iliac artery flow. Multiple strategies include iliac branch devices (IBD), bell-bottom flared iliac stents, and hybrid or snorkel/sandwich procedures.5,6 Anatomic considerations are paramount in endovascular management considerations, particularly the following: (1) the presence and quality of proximal and distal landing zones (e.g., location and length of non-aneurysmal inflow and outflow arteries), (2) the presence of concomitant internal iliac artery involvement, (3) the presence of bilateral or unilateral iliac disease, and (4) the presence or absence of concomitant aortic aneurysm.
Studies comparing outcomes after ET and OS for IAAs are limited to date. The aim of this systematic review was to compare the outcomes of ET versus OS for patients with IAA.
Methods
This study was undertaken according to the “Preferred Reporting Items for Systematic Reviews and Meta-Analysis” (PRISMA) statement.7
Manuscripts on IAA treatment were searched in the Medline database. On January 31st, 2023, the literature search was updated last. The following query was searched in PubMed using MESH terms: “aneurysm, iliac” AND (“endovascular procedure” OR “Open repair” OR “open surgery” OR “treatment”). Two authors (MM and AC) independently undertook the database research. Additionally, reference lists of eligible studies were examined manually to identify more potentially eligible studies by backward citation.
We searched for manuscripts reporting outcomes comparing ET with OS for patients with IAA published in the last ten years (starting in January 2014) when presenting a cohort of at least five patients. Portuguese and English articles were included. Non-English articles were included when an English abstract with extractable data was provided.
Inclusion criteria were described as follows: (i) patients with IAA of atherosclerotic/degenerative etiology; (ii) treatment of the IAA by endovascular and surgical means; (iii) at least intraoperative and/or early extractable results (at least one of the following outcomes: peri-operative complications, length of stay and 30-day mortality). Patients with previous open or endovascular repair of aortic aneurysms, who subsequently developed IAA were considered.
Exclusion criteria included: (i) IAA of etiology other than atherosclerotic/degenerative, such as post-traumatic, post-dissection, infection, or connective tissue disease; (ii) inclusion of aneurysms only of the internal or external iliac artery (iii) inclusion of IAA only followed clinically, not treated (iv) inclusion of IAA only treat by endovascular or surgical means.
Reber's classification was used to classify the iliac artery aneurysms included in the studies.3
Extracted data were: study design (type of study, publication type, retrospective/prospective data analysis, type of treatment), population characteristics (number of patients, number of IAAs, follow-up length, symptoms and timing of treatment), baseline demographics (age, gender), early and late related complications and reinterventions. Non-deducible data were labeled as “not reported” or “non extractable,” as appropriate.
The pre-defined primary outcome was 30-day mortality; Secondary outcomes included length of hospital stay, peri-operative and late complications and reinterventions.
Quality assessment
The methodology of the studies and risk of bias were systematically assessed by two independent reviewers (AC and MM). Study quality evaluation was performed with the “Newcastle-Ottawa “(NO) scoring tool. The total scores ranged from 0 (worst) to 9 (best), with a score of >= 6 indicating high quality. Authorship of the studies was unblinded during the review. Discrepancies between the reviewers during the search, selection, and quality assessment were resolved by discussion.
Statistical analysis
The software Review Manager 5.4 (REVMAN) was used to analyze data. Categorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations. Odds ratios (OR) and 95 percent confidence intervals (CI) were used to compare dichotomous variables and mean differences (MD) with 95 percent CI for continuous data. Statistical heterogeneity was assessed by Cochran's Q test, defined as a measure of the variability of outcomes between studies. The H2 test (Higgins and Thompson) was used to quantify the magnitude of heterogeneity. The parameter I2 retrieved from the H2 test was used with a cut-off of 25% for low, 25-50% for intermediate, and above 50% for high heterogeneity. A fixed-effects model was used when heterogeneity (I2) was inferior to 50%, and a random-effects model was used when heterogeneity (I2) was high. All reported p-values are two-tailed, with a p-value of ≤0.05 indicating statistical significance.
Results
Manuscript search and selection
The database search identified 418 articles, of which 414 records were excluded by screening by title/abstract. Five studies were included (one was included through cross-referencing). Figure 1 displays a flow chart of this search.
Manuscript characteristics and quality assessment
All included studies were retrospective observational analyses. Table 1 summarizes their characteristics.
Quality assessments were conducted on the included studies using Newcastle-Ottawa scale, Table 2.
Table 1 Summary of the five studies included in the systematic review
| Study | Year | Design | Total N | N ET | N OS |
|---|---|---|---|---|---|
| Igari et al. | 2015 | Retrospective, single-center | 32 | 12 | 20 |
| Zhorzel et al. | 2019 | Retrospective, single-center | 106* | 40 | 66 |
| Mendes et al. | 2019 | Retrospective, single-center | 67 | 44 | 25 |
| D'Oria et al. | 2020 | Retrospective, single-center | 593 | 283 IBD, 118 colis | 192 |
| Jalalzadeh et al. | 2020 | Retrospective, single-center | 851 | 618 (100 IBD) | 205 |
*106 aneurysms were reported in 94 patients. ET - Endovascular treatment; OS - Open surgery; IBD - Iliac branched device
Table 2 Quality assessments of the studies included in the systematic review (Newcastle-Ottawa scale).
| Igari et al. | Zhorzel et al. | Mendes et al. | D'Oria et al. | Jalalzideh et al. | |
|---|---|---|---|---|---|
| Selection | |||||
| Representativeness of exposed cohort | * | * | * | * | * |
| Selection of non-exposed cohort | * | * | * | * | * |
| Ascertainment of exposure | * | * | * | * | * |
| Outcomes not presented at the start of the study | * | * | * | * | * |
| Comparability |
Patient’s characteristics
A total of 1837 patients were included. The estimated mean age was 71.38+-8.71 years (73.01+-8.67 in ET and 69.06 +/- 8.25 in OS group, P < .05). Male sex represented 84.73% of the population, with no difference between both groups (OR:1.21, 95% CI: 0.78-1.86).
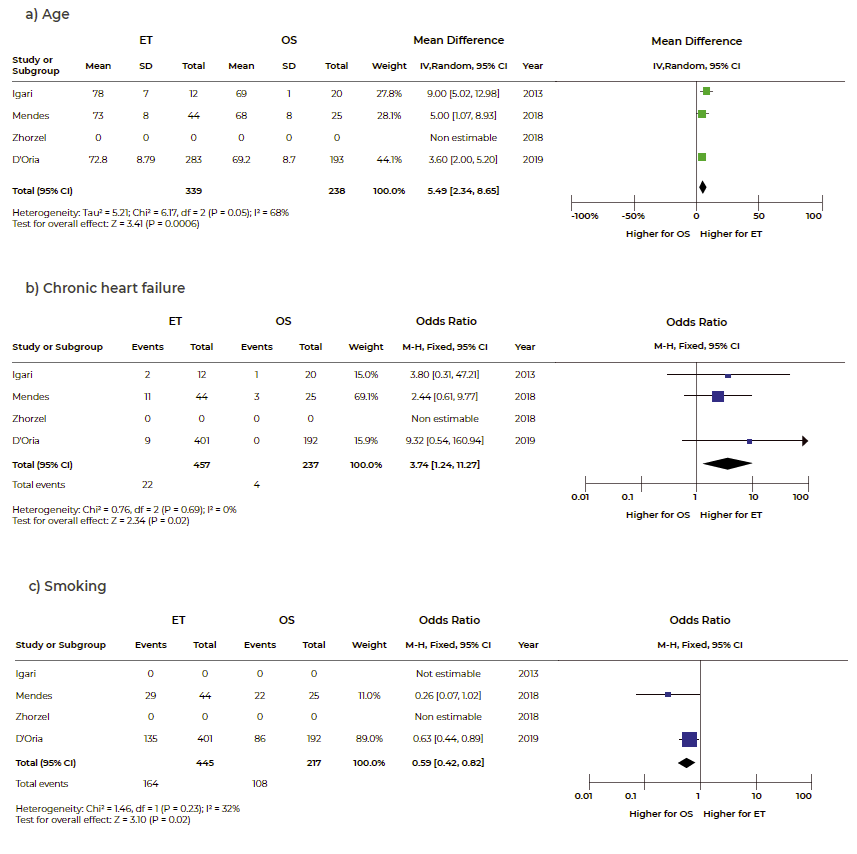
The individual studies included in the systematic review showed no differences in patients´ pre-operative characteristics between the two groups. However, the pooled forest plots showed that compared with OS, patients undergoing ET were significantly older (MD: 5.49, 95% CI: 2.34 to 8.65) and more likely to have congestive heart failure (OR: 3.74, 95% CI: 1.24-11.27). Patients undergoing OS were more often smokers (OR: 0.59, 95% CI: 0.42-0.82), Figure 2.
Aneurysm characteristics
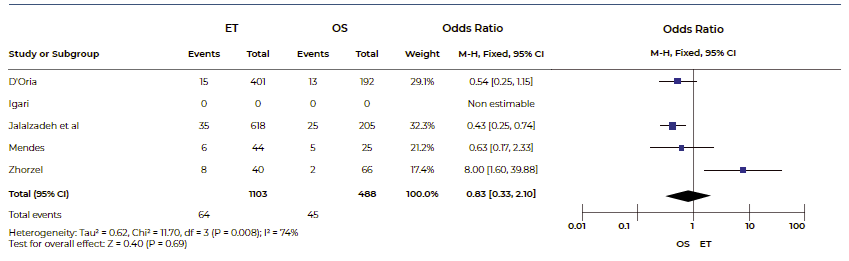
Of the five articles included, three included aortoiliac aneurysms (Doria et al., Jalalzadeh et al., and Mendes et al.) and two isolated iliac aneurysms (Igari et al. and Zhorzel et al.). 1.40% of patients were symptomatic. The mean diameter was 51.42±14.43 mm (50.7±13.36 in ET group and 52.56±15.99 in OS) with no difference between both groups, Figure 3.
Two studies didn´t include information about location of aneurysms.4,5 The other three studies included 168 type I; 21 type III; 53 type II aneurysms according to the Reber classification.
Treatment
OS was performed in 29.02% (442/1523) and ET in 70.58% (1075/1523).
Only three studies1,2,3 described the type of OS, particularly 27 aorto-common iliac bypasses; 6 aorto-common iliac bypasses+ AII ligation; 31 ilio-iliac bypasses with AII preservation; 4 iliofemoral bypass; 9 AII ligation; 14 IIA bypass.
Regarding the type of ET, they were as follows: 15 EVAR with IIA coil embolization, 138 iliac stent-grafting and internal iliac artery embolization, five iliac stent-grafting only, 414 iliac branch design grafts (IBD/IBE/EVAR+ IBD) and five IIA anterior divisional branch embolization and repair extension into the posterior divisional branch.
The mean length of surgery was 159.5+- 92.02 minutes for ET and 376.89+-176.82 for OS.
The mean follow-up length was 9.86+-9.1 months for ET and 18.7+-13.1 months for OS.
Length of stay and Intra- and post-operative outcomes
The mean total length of hospital stay (LHS) was 4.89±6.33 days with significantly longer stays for OS (2.91±4.47 in ET vs 8.68±7.53 in OS; MD: -4.68, 95% CI: -6.43 to -2.92).
In 8.73% of cases, intra-operative complications were reported (4.51% in ET vs 4.22% in OT). Regarding post-operative complications, 2.16% had surgical site infection (1.09% in ET vs 4.22% in OS), 2.01% had renal failure (1.18% in ET vs 3.89% in OS), 3.84% had a respiratory infection (1.98% in ET vs. 8.53% in OS), 1.28% had leg ischemia (0.73% in ET vs. 2.36% in OS), and 0.96% had bowel ischemia (0.97% in ET vs. 0.94% in OS).
OS presented with a significantly higher risk of surgical wound infection, renal failure, and respiratory infection (OR: 0.31, 95% CI: 0.10-0.94; OR: 0.37, 95% CI: 0.18-0.75 and OR: 0.19, 95% CI: 0.11-0.33, respectively). No difference was attained regarding buttock claudication and leg and bowel ischemia, Figure 4.
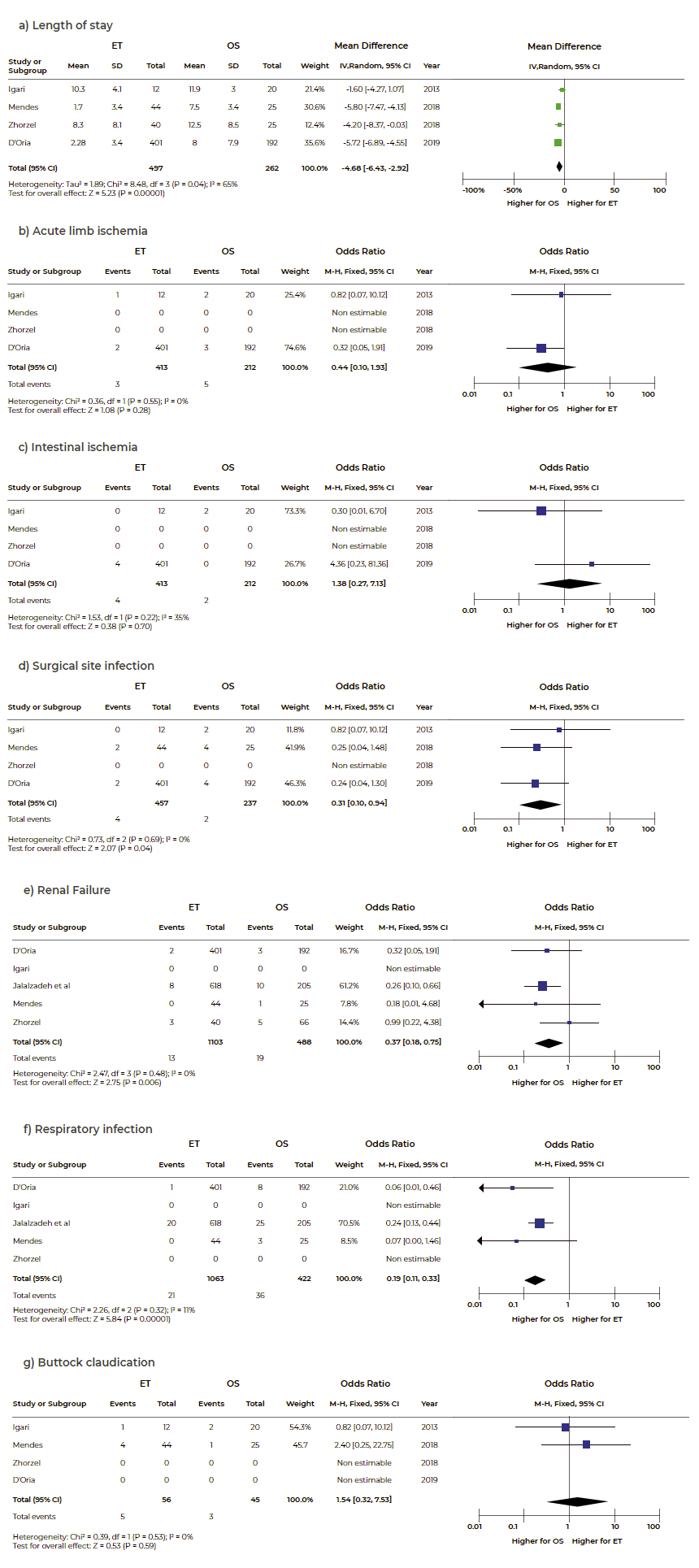
Figure 4 Forest plot for length of stay (a), acute limb ischemia (b), intestinal ischemia (c) surgical site infection (d), renal failure (e), pneumonia (f) and buttock claudication (g)
Estimated overall 30-day mortality was 3% (2% (95%CI 1.2-3) and 5.6% (95%CI 3.5-7.7) after OS or ET, respectively), being significantly higher for OS (OR 0.34, 95% CI 0.19-0.61), Figure 5.
At 30-day follow-up, reintervention rates were not significantly different for OS and ET (10.1%, 95% CI 7.3-12.9 and 5.1%, 95% CI 3.7-6.5, respectively), Figure 6. Erectile dysfunction and readmissions were analyzed only in one study and were not included in the meta-analysis.
Discussion
Regarding quality assessments of the included studies, three of five studies had a score of >= 6 in the Newcastle-Ottawa scale, indicating high quality. None of the studies scored on the comparability criteria since all studies were retrospective, and therefore, the selection of cases and controls wasn´t controlled by any factor. The two studies5,6 classified with 5 points didn´t describe follow-up methods. Only one study included a five-year follow-up length (7 points).2
In the previous literature, no other meta-analysis compared the results of OS and ET, notably including the new endovascular techniques (iliac branch design grafts). The current meta-analysis suggested that ET was associated with a lower risk of surgical wound infection (OR: 0.31, 95% CI: 0.10-0.94), renal failure (OR: 0.33, 95% CI: 0.11-0.98), and respiratory infection and consequently associated with a shorter postoperative LHS when compared with OS.
As expected from the minimally invasive nature of ET, wound complication was less common in the femoral or percutaneous approach than transperitoneal or retroperitoneal approach, which is in accordance with our results. However, according to Xiang et al.8 there were no differences between groups (OR: 0.52, 95% CI: 0.20-1.36), including wound infection and healing disorder. This might be due to a selection bias of healthier subjects for OS intervention or possibly under-reporting of minor complications. Also, according to Xiang et al. ET was associated with a lower risk of blood transfusion (OR: 0.22, 95% CI: 0.08-0.58) and a shorter postoperative LHS. Due to the avoidance of deep pelvic dissection, ET had no risks of visceral, genitourinary, or pelvic venous iatrogenic injuries.8 Two studies also suggested that ET had significantly less intraoperative blood loss. These findings were overlapping with abdominal aortic aneurysms treated with OS or ET.
The current review showed no differences regarding the risk of leg ischemia or intestinal ischemia. However, according to Xiang et al. ET was associated with a higher risk of postoperative ischemic complications (PICs) (which were defined as ischemic symptoms that related to the procedure, such as buttock claudication, bowel ischemia, and erectile dysfunction) although in five of the included studies none of them reported a significant difference between groups, the pooled forest plots showed that compared with OS, ET was associated with a higher risk of PICs (OR: 3.24, 95% CI: 1.05-10.02) which could be explained due to evaluation of ET techniques, which in our study represent more than half on ET.8
Regarding postoperative mortality, as we observed in our metanalysis, in a review conducted by Buck et al., the in-hospital mortality was higher in OS (17.9% vs 6.7%; P < .001).9 However, Xiang et al. reported no differences between the two groups (OR: 0.73, 95% CI: 0.15-3.54).8
In this current metanalysis, at 30 days follow-up, reinterventions rates were not significantly different for OS versus ET (6.5%, 95% CI 4.0-10.2 and 5.8%, 95% CI 3.9-8.38, respectively). Comparing with Xiang et al., two studies reported freedom from reintervention, one of which suggested the freedom from reintervention was significantly higher for OS than for ET at one- and five-year (P< .01), while another one found a non-significant trend.8
Following these results, ET has become a first-line therapy in many vascular centers if applicable to the given anatomy due to the potential for high morbidity and mortality associated with OS.2,3
When the distal seal zone diameter exceeds 25mm, or aneurysmal degeneration extends into the proximal internal iliac artery, the seal zone may be extended into the external iliac artery (EIA) with or without coil embolization or plug occlusion. In the studies included in this review, most cases in which the internal iliac artery wasn´t preserved were treated with concomitant embolization. Papazoglou et al. conducted a study with 137 patients. They found no significant difference in the occurrence of postoperative buttock claudication between the two groups (13.4% for stenting alone and 12% for stenting with coil embolization). After a four-year follow-up, there were also no differences in cumulative survival or the need for secondary interventions between the two groups.10
Preserving internal iliac artery flow is essential in patients with contralateral internal iliac artery occlusion, bilateral common IAAs, or those who are otherwise perceived to be at high risk for spinal cord ischemia. Strategies to preserve internal iliac artery flow include iliac branch devices/endoprosthesis (IBD/E), chimney/snorkel procedures, and hybrid/banana procedures.
Regarding IBD Cook®, Karthikesalingam et al. reported in a review that included nine series reporting the use of the Cook IBD in 196 patients that early technical success was between 85% -100%.11 The review also revealed a postoperative IBD limb occlusion rate of 12% (and half of these patients developed buttock claudication). The reported rate of combined type I or III endoleak was only 1.5%, and the reintervention rate across all series was 6%. Simonte et al. reported experience with the Cook IBD used in 149 patients over a ten-year period with technical success of 97.5%, freedom from reintervention of 91.8% at nine years and hypogastric patency of 90.4% at ten years.12 Regarding The Gore Excluder IBE, data from the IBE 12-04 US pivotal trial (28 centers) and Global Registry for Endovascular Aortic Treatment (GREAT registry, 14 centers) revealed 100% freedom from new buttock claudication symptoms at six months and 90% iliac branch patency over two years.13 Although gaining favorable usage, further long-term results are needed to fully evaluate the longer-term durability of this and other similar devices. Besides, based on the current criteria for IBD use, up to 52% of patients won´t be suitable for these devices.14,15 In patients unfit for IBD/E, a “chimney” type graft can extend into the common or EIA or the “sandwich” technique may be employed. According to Lobato et al., in a series with 40 patients treated with chimneys to EIA and IIA, technical success rate was 100%, primary patency rate was 93.8% (three IIA occlusions occurring early in the study).16 Early and late related mortality rates were 0%, and late unrelated mortality rates were 2.5%.
There were some limitations of this review. As with any systematic review, our conclusions are based on available data from published studies. All studies were retrospective and therefore did not incorporate precise protocols for data collection and analysis. Consequently, follow-up data were inconsistent in most studies and many studies did not report various outcomes of interest particularly the location and anatomical features of the aneurysm. Also, the level of complexity of treating different types of aneurysms is important and introduces heterogeneity in the analysis of the results. Due to the rarity of this clinical entity, the different types of IAA (Type I-IV) and different methods of treatment it is difficult to obtain homogeneous groups to compare.
Although the authors initially included only isolated iliac aneurysms as an inclusion criterion in order to reduce the heterogeneity of the cases included, given the rarity of this pathology and the absence of a significant number of articles found with this criterion, it became imperative to exclude this criterion and the inclusion of series with aortoiliac aneurysms. Another limitation is the duration of follow up, only one study included >30 months of follow-up, which is considered short given the durability of these endovascular repairs.
Conclusion
To the best of our knowledge, this is the first meta-analysis comparing OS and ET, including the results of the newest endovascular techniques of internal iliac artery preservation.
ET can reduce peri-operative complications, length of stay, and 30-day mortality, and so has gained favor over OS as the initial approach of choice for patients with suitable anatomy. Knowledge of all current devices and techniques allows the treatment of almost any patient, regardless of anatomic limitations, when applied creatively and innovatively.
The possible differences in long-term reintervention and mortality rates between the two treatment strategies are still unknown. This information will be crucial for providing appropriate recommendations for managing IAA.