Sweet syndrome is an increasingly recognized disease belonging to the spectrum of neutrophilic dermatosis. It may be classical, malignancy-associated or drug-induced.
A 57-year-old female was admitted for acute intracerebral hemorrhage. Her medical history included epilepsy, intracerebral hemorrhage 9 years before, hypertension, dyslipidaemia, diabetes mellitus type 2 and depression. Two days following admission, carbamazepine 400 mg twice daily was initiated for epilepsy. After five days, she developed multiple erythematous round painless papules and plaques on dorsum of both hands and malar regions, some of them with local bullae and others with target-like appearance (Fig. 1 A-C), with no mucous involvement. No fever or other systemic signs were registered.
The unique medication introduced in the previous 6 months was carbamazepine, whose levels were 14.40 ug/mL (NR 4.00-12.00) when the dermatosis initiated. There was no leukocytosis/neutrophilia but a C-reactive protein of 80 mg/L (N<3.0). A cutaneous biopsy on a dorsal hand lesion yielded an acanthotic ulcerated epidermis and a neutrophilic inflammatory infiltrate with leukocytoclasia in the dermis (Fig. 2 A-C), but no signs of vasculitis. Bacteriological swab of an ulcerated lesion was negative, as well as bacteriological, mycobacteriological and mycological examination of the cutaneous biopsy.
Based on suspicion of drug-induced Sweet syndrome, carbamazepine was stopped once the dermatosis started. Oral prednisolone was initiated at a dose of 0.5 mmg per kilogram for 5 days, with a slow gradual tapering during the following 30 days. The patient evolved with complete remission of the lesions in 7 days, without recurrence after 6 months of follow-up. Epilepsy is currently under control with levetiracetam and there was no need to reintroduce carbamazepine. According to Naranjo’s method for estimating the probability of adverse drug reactions1, Sweet Syndrome in this specific case was probably induced by carbamazepine (6 points).
In order to diagnose a drug-induced Sweet syndrome, specific unique diagnostic criteria should be found, mainly the temporal relationship between drug ingestion and clinical presentation, as well as temporally-related resolution of lesions after treatment with systemic corticosteroids. The disease may recur after drug readministration. Multiple drugs have been implicated in Sweet syndrome, mainly colony-stimulating factors, all-trans retinoic acid, vaccines and miscellaneous drugs.2 Carbamazepine is also known to be a possible trigger, sometimes with bullous presentation, as shown in several large series of drug-induced Sweet syndrome.3,4However, it may be considered an uncommon cause, since some series did not find any case induced by carbamazepine.5
With this case report, we highlight the difficulty of clinical and histopathological evaluation of cutaneous lesions in a patient with multiple co morbidities and provide a new case of carbamazepine-induced Sweet syndrome. This iatrogenic disease may have substantial impact on the therapeutic options of epileptic patients.

Figure 1A-C Clinical features showing multiple erythematous round papules and plaques on dorsum of both hands (A,B) and malar regions (C).
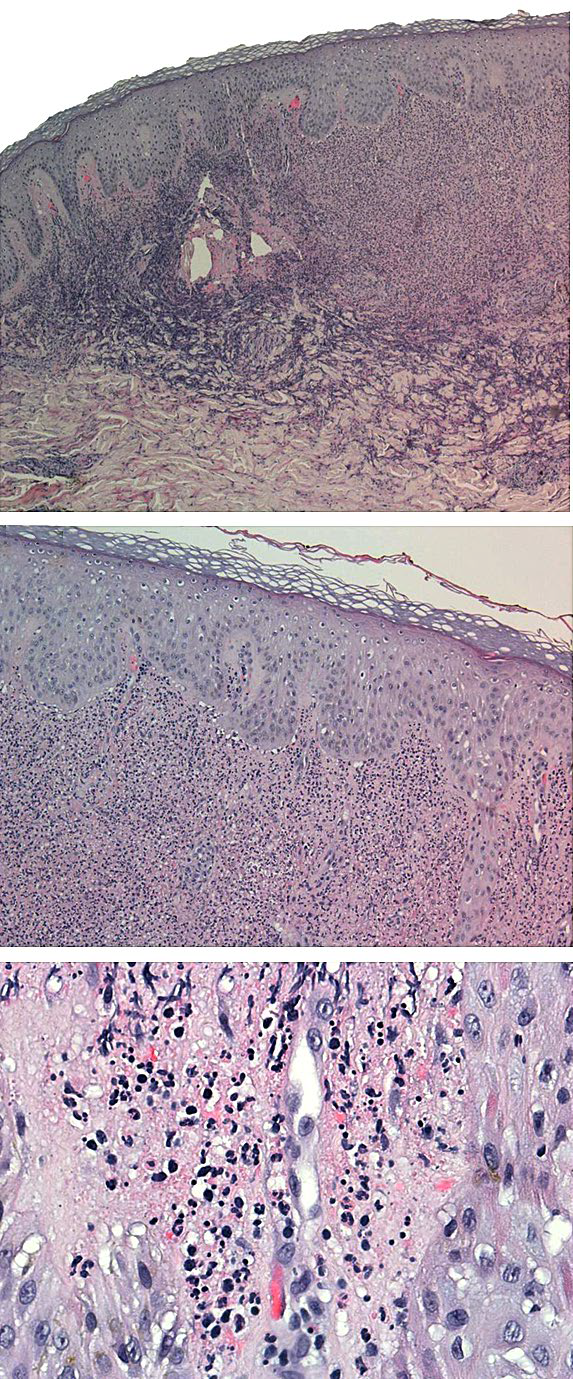
Figure 2A-C Histopathological features showing a dense infiltrate of mature neutrophils in the upper dermis and reactive changes of epidermis (A, hematoxylin-eosin stained slide, 40x); Highlight of the dermis with dense infiltrate of mature neutrophils (B, hematoxylin-eosin stained slide, 200x); Highlight of leukocytoclasia, with nuclear dust (C, hematoxylin-eosin stained slide, 400x















