To the Editor:
We read with interest the article “Cutaneous metastasis as the presenting sign of urothelial carcinoma”.1 We present a case that further illustrates the bad prognosis associated with skin metastases in patients with renal and urothelial neoplasms.
A 68-year-old woman presented to our dermatology department with a 3-month history of a rapidly enlarging, asymptomatic nodule in the occipital region. Past personal history was relevant for a clear-cell renal cell carcinoma (RCC) and left radical nephrectomy 5 years prior to presentation; the margins were then deemed clear of tumor. One month after surgery, bilateral pulmonary metastatic disease was detected through computed tomography (CT) scan and histopathologic examination. Since then, the patient had been under immunotherapy with Nivolumab, with regular follow-up and stable disease. She denied fatigue, fever, weight loss, abdominal pain, or other symptoms. Physical examination revealed an exophytic, pedunculated, firm, oval, 3 x 2 cm erythematous nodule in the occipital region (Fig. 1A). No other skin lesions, lymphadenopathy, or abdominal masses were detected, and the remaining physical examination was unremarkable.
Surgical resection was performed. Histopathologic examination revealed a dermal nodular growth with a predominant solid architecture and a regular network of small, thinwalled blood vessels (Fig. 1B). It was composed of epithelioid cells with clear cytoplasm and distinct cell membranes, with inconspicuous nucleoli. PAX8 was expressed in a nuclear distribution, supporting the diagnosis of metastatic RCC (Fig. 1C). Specimen margins were free of neoplasm. A postoperative positron emission CT scan revealed brain nodules with metabolic activity suggestive of metastatic disease. Systemic treatment was switched to axitinib, however disease progression ensued, and the patient died six months later.
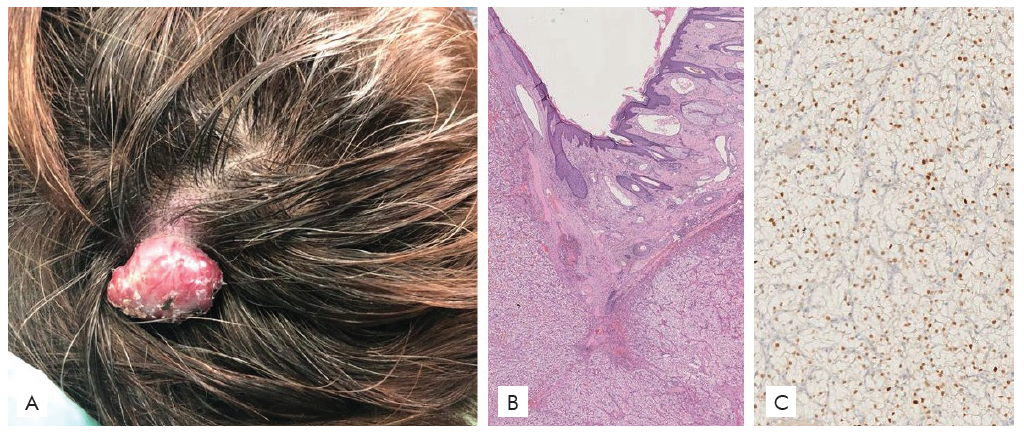
Figure 1 (A) Exophytic, pedunculated, firm, oval, 2.5 x 2 cm erythematous nodule in the occipital region. (B) Histopathologic examination revea-led epithelioid cells with clear cytoplasm and irregular nuclei. (C) Immunohistochemical stain for PAX8 was positive.
Cutaneous metastases of RCC are considered a rare phenomenon, occurring in 3% of cases of metastatic RCC.2 Single or multiple, rapidly growing, asymptomatic, erythematous-violaceous nodules or tumors are typically observed.2 The most common locations are the face and the scalp.3 Arteriovenous shunts are thought to facilitate tumor dissemination to the head.3
RCC metastases on the skin can have a vascular appearance, and therefore be mistaken for a pyogenic granuloma, Kaposi sarcoma, angiosarcoma, or other vascular tumors.3 Although they are generally detected within 5 years from the primary tumor diagnosis, skin metastases occasionally develop decades later.4
The preferred approach for single, isolated skin lesions consists in surgical removal.5However, in up to 90% of cases, concomitant visceral metastases can be found, which explains why cutaneous metastases of RCC are associated with a poor prognosis, and a tumor-specific survival of less than six months.6
RCC cutaneous metastases frequently herald the development of visceral RCC metastases, which emphasizes the role of skin examination in the follow-up of patients with this malignancy.3















