The new European guidelines on cardiovascular disease prevention 1 have been prepared by thirteen European scientific societies and have introduced notable innovations. These are more complex guidelines than the previous ones because they seek a more personalized approach, which certainly reflects the diversity of patients we see in general practice.
The therapeutic goals for LDL cholesterol, blood pressure, and glycaemia have not changed compared to the previous guidelines, but the way of controlling them has been modified, recommending a stepwise approach (step 1 and step 2). This approach is not conceptually new and attempts to reflect the usual clinical practice of progressive intensification of therapeutic strategies, as part of a shared decision process between health professionals and patients. It is recommended to always reach step 2, and the intensification of treatment will depend on the 10-year and lifetime risk, the benefit of treatment, comorbidities, frailty, and patient preferences.
The guidelines present for the first time a new model for calculating risk - Systematic Coronary Risk Evaluation-2 (SCORE2) 2 and Systematic Coronary Risk Evaluation-2 Old Person (SCORE2-OP) 3 - which has been calibrated for four regions of Europe according to vascular mortality rates, with Spain belonging to the countries with low cardiovascular risk and Portugal to the countries with moderate cardiovascular risk. This tool allows the calculation of the risk of cardiovascular morbidity and mortality in the next ten years (myocardial infarction, stroke, and cardiovascular mortality) in men and women between 40 and 89 years of age. It can be calculated through the App of the European Society of Cardiology (ESC) or the tool available on the web (https://www.-prevent.com). Through these applications, it is also possible to calculate the lifetime cardiovascular (LIFE-CV model) and the benefits of treatment in terms of years of life gained without cardiovascular disease. In addition, there are specific tools for calculating risk in people with diabetes (ADVANCE risk score or DIAL model) and with established cardiovascular disease (SMART RISK score or SMART REACH model).
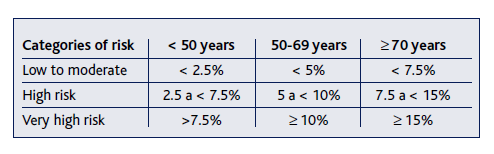
Another substantial novelty is the establishment of different risk thresholds depending on age, as shown in Table 1, to avoid undertreatment in young people and overtreatment in the elderly.
Three different algorithms for calculating cardiovascular risk and treatment of cardiovascular risk factors for apparently healthy people, patients with diabetes, and patients with atherosclerotic vascular disease are shown in the guidelines.
Much more emphasis is placed on health policies as a population prevention strategy. In the guidelines it is proposed the most cost-effective interventions at the population level are to create environments that promote healthy lifestyles, modifying risk factors such as physical inactivity, unhealthy eating, tobacco and alcohol consumption, exposure to air, and noise pollution, and acting on climate change. In addition, different methods (government, media, and education, labeling and information, economic incentives), settings (schools, workplace, community), and actions are described for each of them, supported with a level of evidence and a class of recommendation.
Now it is time for the implementation in clinical practice, to see the advantages and disadvantages, potential barriers and how can we overcome them.