The ovarian fibromatosis (OF) is a rare, benign, cause of ovarian enlargement, which affects young women,(1,2) and is usually unilateral, but there are bilateral reports.(1,2) Ovarian enlargement is characterized by diffuse fibrosis(2), which determines menstrual irregularity, abdominal pain, and less commonly, hirsutism and virilization.(1,2)
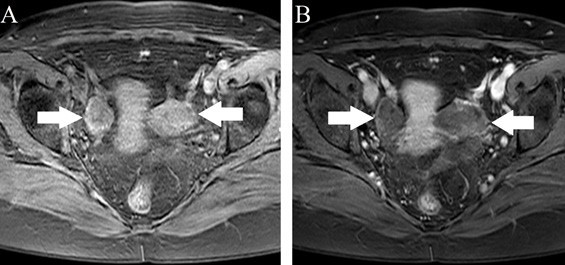
32.Magnetic resonance imaging (MRI) assists in the diagnosis, showing adnexal lesions with hypointense signal on T1 and T2 sequences, and an appearance of solid mass (resembling other pathologies, such as fibroma, tecoma, desmoid tumors and massive ovarian edema);(1) it may present an image similar to a black wreath on the T2 weighted sequence, attributed to fibrous tissue´s low signal intensity,(2,3) that helps distinguish it from other pathologies.
33.In ultrasonography, its echogenicity is variable, with preserved ovarian follicles in the periphery.(3) In computed tomography, the image is relatively hyperdense, homogeneous and solid, and may present calcifications.(3) The pathogenesis of ovarian fibromatosis is not fully understood due to its rarity.(1) According to Lalwani et al,(3) it is believed that this may be a consequence of a long-standing ovarian edema. Microscopically, there´s proliferation of spindle cells(1,2) and an abundant collagen matrix between normal structures are seen,(1,2,3) with no infiltrative pattern.(1,2) This fibrous tissue is also found in other neoplastic diseases such as fibroma, tecoma, Brenner, Krukenberg and desmoid tumors, which are differential diagnosis of ovarian fibromatosis.(1,3) Due to ovarian enlargement and similar clinical picture, another differential diagnosis is the massive ovarian edema, but microscopically we are able to differentiate it: its histopathology shows stromal cells separated by edema fluid, along with dilation of lymphatic and vascular vessels.(1)
34.There have been described associations of ovarian fibromatosis with omentum fibrosis, idiopathic sclerotizing peritonitis and intraperitoneal fibromatosis,(1) the latter more related to androgenic manifestations.(1)
35.The therapeutic approach will depend on patient’s age and MRI findings. However, a more conservative one, in order to preserve fertility and ovarian function, should be prioritized. Oophorectomy or salpingo-oophorectomy should be reserved to extreme cases.(1)
36.We report the case of a 46-year-old woman, in a routine consultation, who underwent transvaginal ultrasonography, which demonstrated bilateral adnexal, lobulated and heterogeneous mass (Figure 1). Informed consent was obtained from the patient. She was asymptomatic, and had no medical conditions background. She reported menarche at 11 years old, and premature menopause at 37 years old. Physical examination was unremarkable. She performed an MRI, which demonstrated both ovaries of increased dimensions, with its fibrous edges thickening that traps follicles, along with heterogeneous contrast enhancement (Figures 2 and 3). Such findings were consistent with bilateral ovarian fibromatosis, and the patient has been followed up on an outpatient basis ever since, with no further clinical or surgical interventions.
37. 38.
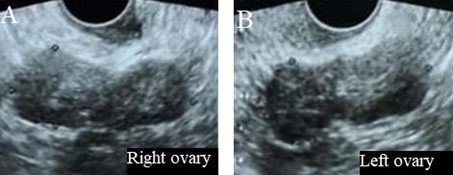
Figure 1: Ultrasonography demonstrating a lobulated and heterogeneous mass in the right ovary (A) and in the left ovary (B).
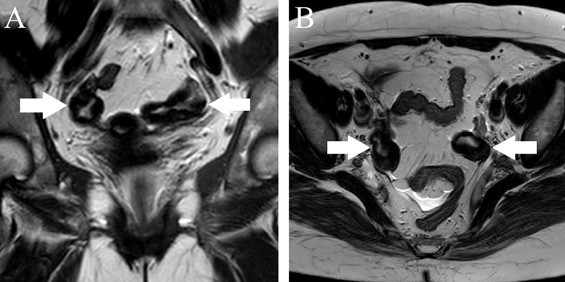
Figure 2: MRI in T2 weighted sequence (A, coronal image; B, axial image) demonstrate increased ovarian size, fibrous thickening with its trapping follicles (white arrows).