Case
A 45-year-old woman, housekeeper, was sent to the Rheumatology appointment for pain and functional limitation in extension and flexion movements of the fingers, accompanied numbness in the 4th and 5th finger of the right hand. This clinical depiction had 2,5 years of evolution, with progressive worsening. The physical exam showed pain at palpation of ulnar nerve in the ulnar fossa of the right elbow. Blood tests and electromyography studies did not show any significant changes. Ultrasonography of the elbow revealed no changes of the median and radial nerves. The Ulnar Nerve (UN) presented without any anomalies in its entire course, except being bipartite in a small portion immediately proximal to the ulnar fossa, returning then to its unique configuration. (Fig. 1). This anatomic variation was then confirmed by Magnetic Resonance Imaging (MRI) as illustrated in Figure 2. The patient was referred to Plastic Surgery and submitted to an ulnar nerve surgical decompression at proximal level. Two weeks after surgery a sustained marked improvement of the numbness was confirmed.
Discussion
Anatomical variations of the UN can occur in all its course however, the ones occurring along UN proximal course are rarely described in the literature.1
Although there are descriptions of peripheral neuropathies associated with bipartite median nerve,2 our research did not find a similar description of bipartite UN at a proximal level. Olave et al have previously described a variation at a more distal level in which the UN divides in two branches proximal to the distal wrist crease, reuniting again distal to the distal wrist crease and forming the common palmar digital nerve of the 4th interosseous space.3
This case demonstrates the importance of deep anatomy knowledge in the evaluation of peripheral neuropathies and motor deficits, that overlooked can result in delays of diagnosis.
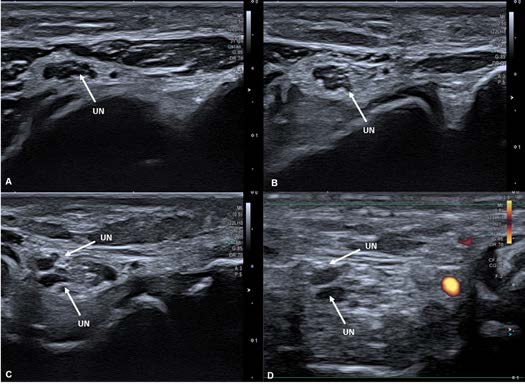
Figure 1: Right Elbow Ultrasono- graphy Transverse Cut: Ulnar nerve at different levels of its course going distal to proximal (1A to 1D). It starts with its usual unique configuration (1A and 1B) and then starts to split (1C). Through Fig. 1D it is possible to distinguish the ulnar nerve (without Power Doppler signal) from blood vessels (with Power Doppler signal).
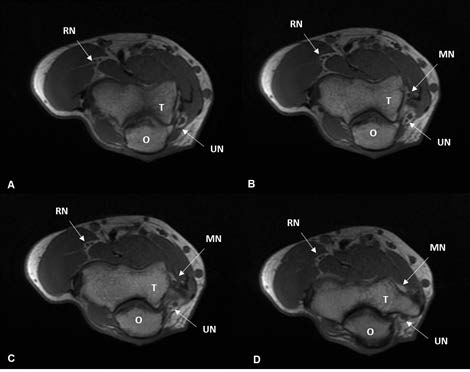
Figure 2: Right Elbow MRI T1 Wei- ghted Axial Cut: ulnar nerve at different levels, going from distal to proximal (2A to 2D). It is possible to observe the bi- partite ulnar nerve in a small portion of its path (2B and 2C) and then it returns to its unique configuration (2D). Abbreviations: MN - Median Nerve, O - Olecranon process, RN - Radial Nerve, T - Trochlea, UN - Ulnar Nerve.















