A 55-year-old man refers to edema in his right thigh for one year. He underwent resection of myxoid liposarcoma in his right thigh 13 months ago. Subsequently, he performed 33 sessions of radiotherapy and twelve sessions of chemotherapy with doxorubicin and ifosfamide. He treats diabetes mellitus with a diet. He states that the thigh edema worsens during the day, improving when sleeping, presenting together with intermittent pain of mild intensity since the eighth session of chemotherapy - after finishing radiotherapy and less than four months after initiation of the chemotherapy. Physical examination shows the darkening and thickening of the skin in the medial region of the thigh without pain on palpation. He has difficulty flexing the hip and knee, having difficulty in crouching, and performing movements with pain.
In the first test after radiotherapy and chemotherapy, magnetic resonance imaging (MRI) demonstrates an extensive collection between the semimembranosus and adductor Magnus muscles. It also demonstrated a slight high signal of the vastus medialis, adductor longus, adductor Magnus, sartorius, gracilis, semimembranosus, and semitendinosus muscles, being compatible with radiation-induced myositis (Figure 1). He started treatment with corticoids, and sixteen months later, he had no symptoms and the MRI was normal (Figure 2).
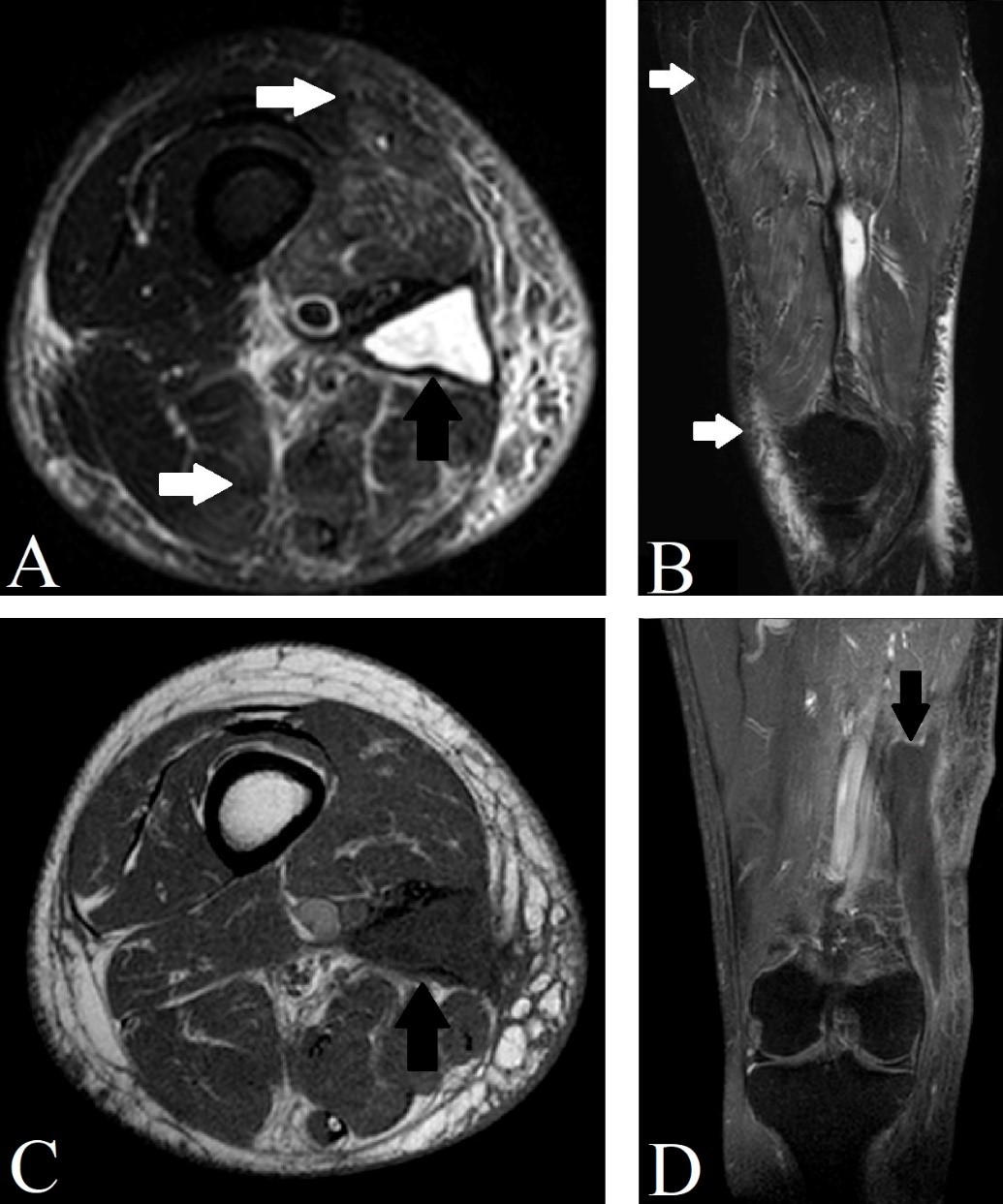
Figure 1: T2 STIR sequence MRI in axial (A), and sagittal (B) sections demonstrating a radiation-induced myositis (white arrows) and collection (black arrow). T1 sequence MRI in axial section (C), and T1 SPIR with contrast coronal section (D) demonstrating the collection (black arrow).
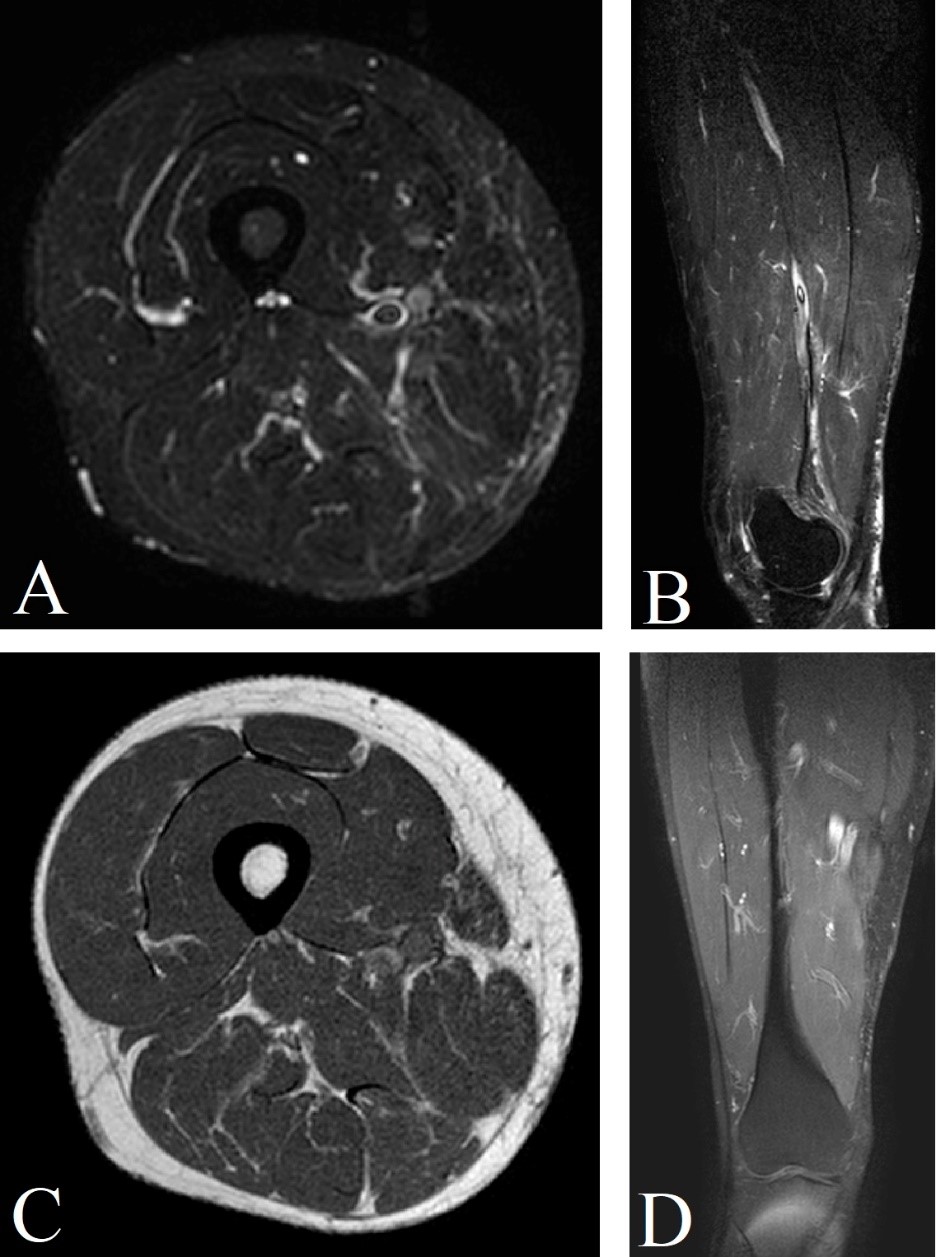
Figure 2: T2 STIR MRI in axial (A), and sagittal (B) sections, T1 axial section (C), and T1 SPIR with contrast coronal section demonstrating a normal thigh after appropriate treatment.
The detail of radiation recall pathophysiology remains to be elucidated. Peritumoral normal tissue is, surely, irradiated during radiotherapy. It also depends on the area and dimensions of the target volume as well as the accumulative dosage.1 Relying on the temporal period after irradiation, acute, subacute, and chronic changes are reported in co-irradiated normal tissue that can be identified by imaging.1 Radiation injury can be temporary or constant.1
Radiation-induced muscle injury is rarely reported in the literature.2 A possible determinant of radiation-related muscle injury is a 'high' dose per fraction, but lesions usually (but very occasionally) occur at a total dosage of over 50 Gy.1 Radiation recall is a rare phenomenon, defined as an acute inflammation triggered by subsequent chemotherapy that develops in a previously irradiated field.2 A several range of drugs utilized in the treatment of cancer is correlated with radiation recall.4 It is not possible to determine the true incidence.3 On the other hand, the antineoplastic drugs with which radiation recall reactions have been most commonly reported include the: 3
Anthracycline doxorubicin
Taxanes docetaxel and paclitaxel
Antimetabolites gemcitabine and capecitabine.
The critical differential diagnosis is post-therapeutic tumor recurrence.1 Typical latency periods, location and matching with the radiation field are essential differentiation criteria as well, depending on the tumor biology and the radiation technique.1
The treatment involves rapidly stopping the use of a chemotherapeutic agent and treating with corticosteroids, analgesia, topical creams, or no therapy until symptoms improve.2 It remains a poorly understood phenomenon, but increased awareness may aid in early diagnosis and appropriate management.3 There are no identifiable features of drugs that cause radiation recall.3 Therefore, there is a chance that any drug is used after radiotherapy, including those from new drug classes.3
The radiologist must be aware of the characteristic imaging morphology of radiogenic tissue modifications to detour erroneous interpretations during follow-up studies.1















