Introduction
Hepatocellular carcinoma (HCC) is the number one malignancy of the liver, the fifth most common tumour worldwide and the third most common cause of death related to cancer [1]. Chronic liver disease and cirrhosis remain the most important risk factors to develop HCC [2]. Most cases of HCC are diagnosed at an advanced stage, and the tumour spreads most frequently to the lungs, peritoneum, adrenal glands, and bones [3]. Intra-cavitary cardiac metastases are very unusual in HCC, and when they occur, they usually invade the heart as an extension of intravascular metastasis or infiltration through nearby organs [4]. The prognosis is poor for metastatic HCC, but surgical treatment, especially in symptomatic intracardiac metastasis, may improve not only quality of life but also survival [5].
Herein, we present a case of an isolated metastasis of HCC to the heart, in which symptoms led to the diagnosis of the primary neoplasm. Informed consent was obtained from the patient’s relatives.
Case Report/Case Presentation
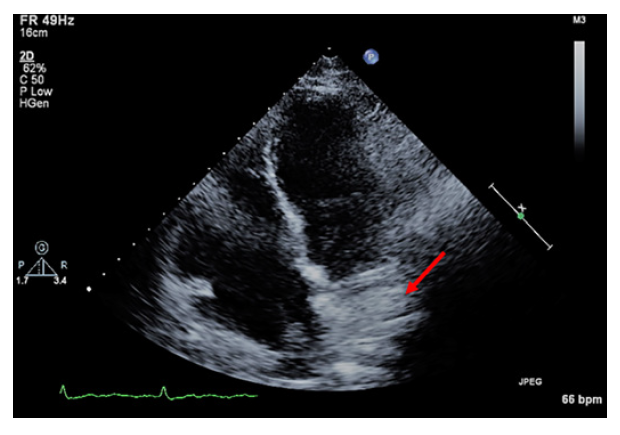
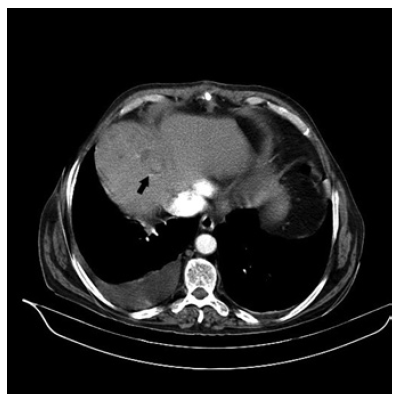
We present the case of a 68-year-old male with reported history of systemic arterial hypertension, hypercholesterolemia, benign prostatic hyperplasia, and alcoholic liver cirrhosis of Child-Pugh A with no recent follow-up, medicated with lisinopril, simvastatin and dutasteride + tamsulosin. He was a non-smoker but had sustained alcoholic habits, had no known allergies and his family history was irrelevant. He presented to the emergency department with dyspnoea, orthopnoea and lower limbs oedema of 4 months duration and acute aggravation. He was initially diagnosed with acute heart failure and medicated with furosemide. A transthoracic echocardiogram was scheduled to evaluate the cardiac function, which showed a mass comprehending almost the totality of the right atrium, obliterating its entrance nearly completely and impeding the normal auricular-ventricular flux, described as an auricular myxoma (Fig. 1). The patient was promptly transferred to cardiothoracic surgery and submitted to an urgent intervention to remove the mass completely. Macroscopically, it was not compatible with a myxoma, but rather with malignant metastatic tissue, which was why the patient was then transferred to internal medicine to investigate the location of the primary tumour, while waiting for the histological results. A multiphasic contrastenhanced computed tomography (CT) scan evidenced a 3.5-cm nodule in the IV segment of the liver, with arterial enhance-ment and subsequent washout on the portal phase, with no evidence of malignant disease elsewhere (Fig. 2).
The diagnosis of HCC with single heart metastasis was established with the aid of the histopathological result of the atrial mass, which showed an epithelioid neoplasm of solid and trabecular pattern with areas of necrosis, constituted of bulky cells of granular eosinophilic cytoplasm with round nuclei and with a prominent eosinophilic nucleolus. The immunohistochemical study showed diffuse and intense immunoreactivity of the neoplastic cells for HepPar-1, in the absence of expression of S100, vimentin, CD34, factor VIII, alpha fetoprotein and AE1AE3, compatible with metastatic hepatocarcinoma.
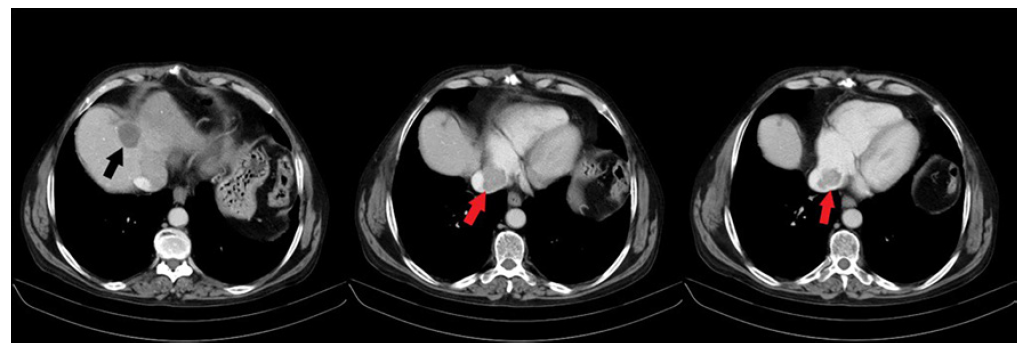
Considering that the single metastasis had been removed with no evidence of portal invasion or any other metastatic disease, it was decided that the patient should undergo radiofrequency ablation (RFA) followed by sorafenib 400 mg/day. During this period, the patient stopped consuming alcohol, having been medicated with oxazepam and baclofen without relapsing. One month after the RFA, the CT scan showed signs of complete response. Nevertheless, 1 year later, the patient recurred with a new liver lesion of 14 mm in the IV segment and was again submitted to RFA with complete response. One year later, on a control CT scan, the patient presented an invasion of the inferior vena cava by a tumoral mass with extension to the right atrium and an extensive lesion of the liver comprehending the IV and II segments (Fig. 3), after which referral to palliative care was decided.
He maintained sorafenib for another 2 years with progressive vascular invasion, that is, with portal vein thrombosis and extension to the medial and right hepatic veins. Progressive hepatic en-cephalopathy and increasing oedema led to his hospitalization and death. The survival time of this patient, from the date of diagnosis, was 4 years and 3 months.
Discussion/Conclusion
This unique case shows the development of single metastatic disease of the heart in a patient with previous alcoholic liver cirrhosis who missed the follow-up. Although HCC may metastasize to various extrahepatic organs, metastases with cardiac involvement are rare [6], generally occurring in advanced stages of the disease with invasion of the portal vein and evidence of portal thrombosis [4], which were both absent at diagnosis in this particular case report.
The prognosis of HCC with cardiac involvement is poor, and the median survival time at diagnosis is 102 days [7]. Our patient survived for 4 years and 3 months, most of them with good quality of life and autonomy, with a total of only 33 days of hospitalization in that period. This may be due to the initial and early surgical approach to metastatic disease.
Although we were initially optimistic about the patient’s evolution after the initial removal of the atrial mass and RAF of the first liver injury, the recurrence of HCC and metastatic disease in the inferior vena cava may indicate that haematogenous spread of the previous disease to the atrial implant had occurred, even in the absence of macroscopic invasion of the portal vein at the time of diagnosis.