An 80-year-old Caucasian woman was hospitalized with a 2-month course of intermittent fever (max. 38 ° C), asthenia, weight loss (12%), anorexia and nausea. Her medical history includes breast cancer submitted to radical mastectomy and axillary lymph node dissection, papillary thyroid carcinoma and pulmonary and ocular tuberculosis that had been treated more than 5 years previously. She had heart failure, arterial hypertension, dyslipidaemia and obesity under treatment.
Physical examination showed obesity and left upper limb lymphedema. Abdominal and rectal examinations were unremarkable. A laboratory study revealed iron deficiency anaemia with haemoglobin 10 g/dL and ferritin 10 ng/mL (normal = 10-120 ng/mL), elevated lactate dehydrogenase 1,379 U/L (normal <247 U/L), aspartate transaminase 59 U/L (normal <31 U/L), alkaline phosphatase 185 U/L (normal = 30-120 U/L), C-reactive protein 21.9 mg/dL (normal = 0-0.5 mg/dL) and a normal procalcitonin value. A bacterial, mycobacterial, viral or fungal infectious disease was excluded by blood, urine and sputum cultures. A thoracic abdominal and pelvic computerized tomography (CT) scan as negative for malignant disease.
During hospital stay she presented with intense nausea and vomiting during most meals. A red blood cell transfusion was necessary due to progressive decrease in haemoglobin. Upper endoscopy was performed showing multiple black nodular lesions in the stomach and duodenum (Fig. 1). Narrowband imaging revealed the presence of black patches on the top of these nodular lesions (Fig. 2). Histopathological examination showed an epithelioid malignant injury with intense and diffuse HMB45 expression suggestive of pigmented melanoma (Fig. 3). The diagnosis of gastrointestinal metastatic melanoma was made. A positron emission tomography/CT scan revealed the presence of bone, cervical and mediastinal lymph node metastases. BRAF gene mutation was not present. The primary tumour was not found. Due to the patient’s limited functional status no treatment was initiated, and death occurred 4 months after diagnosis.
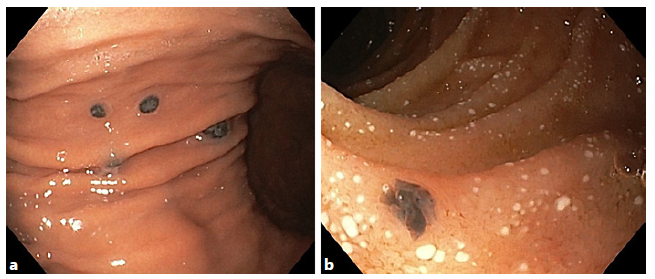
Fig. 1 a In gastric mucosa, multiple black nodular lesions were identified with white light. The two largest lesions of 5 mm were present on the distal body. These lesions were suggestive of melanoma metastasis. b Similar black nodular lesion of 3 mm on the duodenum.
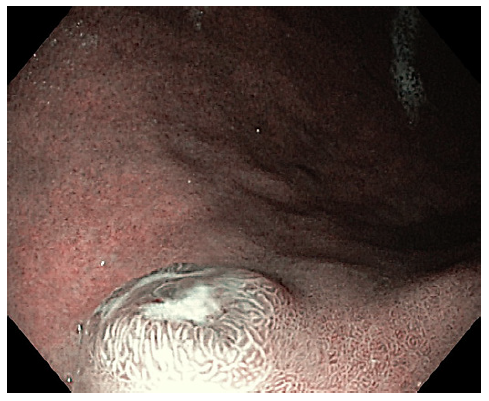
Fig. 2 Narrow-band imaging: black patches present on the summit of elevated lesions. The lesions’ base showed an enlarged regularly placed oval and elongated pit pattern in contrast to a small pit pattern of the surrounding normal gastric mucosa.
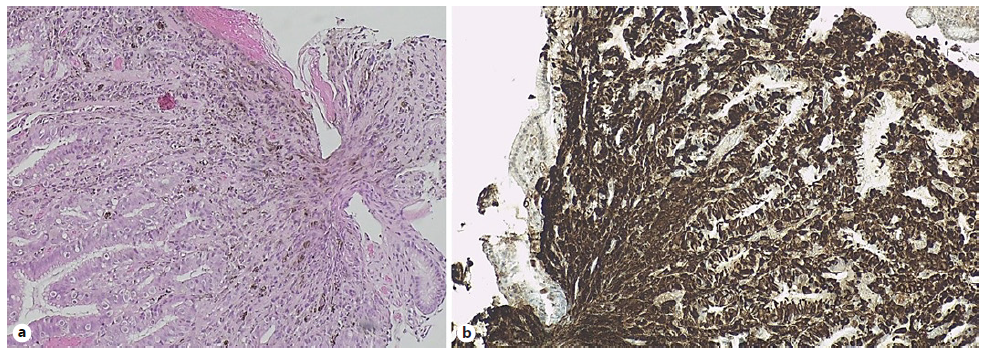
Fig. 3 a Lamina propria diffuse infiltration by epithelioid malignant neoplasia. Haematoxylineosin staining. ×40. b Tumoural cells show intense and diffuse expression for HMB45. HMB45. ×40.
We present a metastatic gastric melanoma in an elderly woman without any history of melanoma with a very rare presentation. Melanoma gastrointestinal metastases are rare and represent a late stage of malignant disease. Its incidence in clinical and autopsy series varies between 0.2 and 0.7%, and it has been reported that only 7% of gastric metastases are due to malignant melanoma [1]. Primary tumours commonly occur in the skin but can also develop from other tissues containing melanocytes such as the meninges, gastrointestinal tract and eyes. Primary or metastatic malignant melanoma of the gastrointestinal tract is an uncommon entity, and more than 90% of cases are identified only during autopsy. The most common gastrointestinal metastatic sites are the jejunum and ileum, followed by the colon, rectum and stomach [2]. The diagnosis is difficult due to non-specific symptoms. Symptoms are present in only 1-4% of patients, and they are related to complications such as haemorrhage, obstruction and perforation [3]. Imaging studies have low sensitivity for diagnosing, and CT sensitivity is only 60-70% in detecting metastases [4]. Gastrointestinal endoscopy allows the diagnosis [3]. Depending on the patient’s functional status, treatment includes surgical resection, immunotherapy, targeted and radiation therapy. The average life expectancy following diagnosis is 4-6 months [5].














