Introduction
End-stage liver disease (ESLD) is associated with high mortality [1], with compensated cirrhosis survival estimated to be 10-13 years and about 2 years in decompensated patients [1]. This mortality is comparable to other organ insufficiencies such as heart failure [2] and chronic obstructive pulmonary disease [3]. The need for palliative care (PC) in patients with ESLD is presumed to be very relevant - a high prevalence of symptoms has been described, with about 80% of ESLD patients with at least one symptom of moderate to severe intensity and an average of 4.1 severe symptoms/patient [4]. These needs are also in line with similar symptom prevalence in other organ insufficiencies in advanced stages, namely for pain and dyspnea. In addition to physical needs, other needs - such as psychological, social, and even spiritual - may arise in patients with ESLD. These are often associated with chronic consumption of alcohol or other drugs, in a population that often is in full active life, and specific guid-ance would be beneficial for the patient, family, and care-givers [5].
Previous studies suggested benefits of PC in patients with ESLD, such as reduced hospital readmissions [6-8], less invasive treatments, shorter hospital length of stay [9, 10], and higher rates of advanced care planning [11]. In Portugal, in the only identified study [12], more than 80% of patients hospitalized with ESLD due to a decompensation episode had NECPAL CCOMS-ICO© [13] criteria for PC. The needs they referred and their transplantation perspective status were not specified.
PC referral rates in these patients remain very low, and the available data are scarce in this regard [9]. Very few studies addressed PC in ESLD patients with transplantation prospect, none including Portuguese population. In one of the few known studies, only 10% of patients excluded from the transplant list were referred to PC [14]. Low rates of advance care planning discussions persist among liver transplant candidates [15], and the current growing trend, of older age and with more comorbidities, poses greater complexity of their needs and care [16]. This subgroup of patients is also frequently the target of more aggressive treatment proposals and, consequently, at risk of greater complications and greater needs. Transplant candidates should not be excluded from PC studies [17].
The purpose of this study was to evaluate what are the specific PC needs of ESLD patients, including those with transplantation perspective, and to investigate whether there are significant differences in this subgroup. Given the coexistence of cancer may have an impact, hepatocellular carcinoma (HCC) as a comorbidity was also considered.
Materials and Methods
Patient Selection
This is a single-center prospective study that included all consecutive adult patients (>18 years) diagnosed with ESLD who underwent hospital admission related to their liver disease (for acute decompensation or HCC treatment) at Centro Hospitalar e Universitário do Porto (Porto, Portugal), between November 2019 and September 2020. Patient identification was carried out twice a week by systematic search of the list of patients admitted to the Departments of Gastroenterology, Medicine, Hepato-Bilio-Pancreatic Transplant and Medical-Surgical Intermediate Care Units. Patients aged <18 years, with previous liver transplantation, or with isolated acute liver failure or with another terminal disease (except HCC) were excluded.
Data Collection
Demographic, functional (through the Palliative Performance Scale (PPS) [18]) and clinical characteristics were registered. Patients were screened for PC criteria using NECPAL CCOMS-ICO© [13]. It is an instrument capable of both identifying patients in need of PC and accurately predicting mortality, thus facilitating planning for end-of-life care [19]. NECPAL CCOMS-ICO© is a validated physician screening tool which combines the Surprise Question with additional indicators (request or need for PC, general clinical indicators of severity and progression, including comorbidity and resource use, and disease specific indicators, including ESLD). Patients with positive Surprise Question (if physician would not be surprised if the patient were to die in the next 12 months) were also considered NECPAL positive when they presented at least one additional parameter from the NECPAL tool. The questionnaire was answered by an internal medicine resident and reviewed by an internal medicine specialist with PC competence. Specific PC needs were assessed through the IPOS questionnaire [20]. This is also a validated instrument widely used globally and specifically developed for use among patients with advanced diseases including ESLD. IPOS questionnaire is a concise but comprehensive instrument, assessing not only symptoms (pain, shortness of breath, weakness or lack of energy, nausea, vomiting, poor appetite, constipation, sore or dry mouth, drowsiness, and poor mobility), but also extending to communication needs, practical concerns, anxiety or low mood, family anxieties and overall feeling of being at peace. IPOS has ten questions (17 items), for the majority of these, five response options are provided. The overall IPOS score is the sum of the scores from each question, ranging from zero to 68. It has two versions, to be completed by healthcare professional or patient, the last one was considered in the present study. When patients presented with encephalopathy (with West Haven grade II or more [21]), IPOS questionnaires were answered by the caregiver considered to be his/her legal representative. Sub-group comparative analysis was performed between ESLD patients with and without HCC and patients with a transplantation perspective (under evaluation or already awaiting liver transplantation) and patients without transplantation perspective (without evaluation or already excluded for transplantation). The local ethics committee considered this study favorably and written informed consent was collected for all patients included, prior to data collection.
Data Analysis
Statistical significance was set at p < 0.05. Statistical analysis was performed using IBM SPSS Statistics 26. Baseline characteristics, PC criteria, and specific PC needs were compared between sub-groups by the Mann-Whitney test.
Results
Study Population
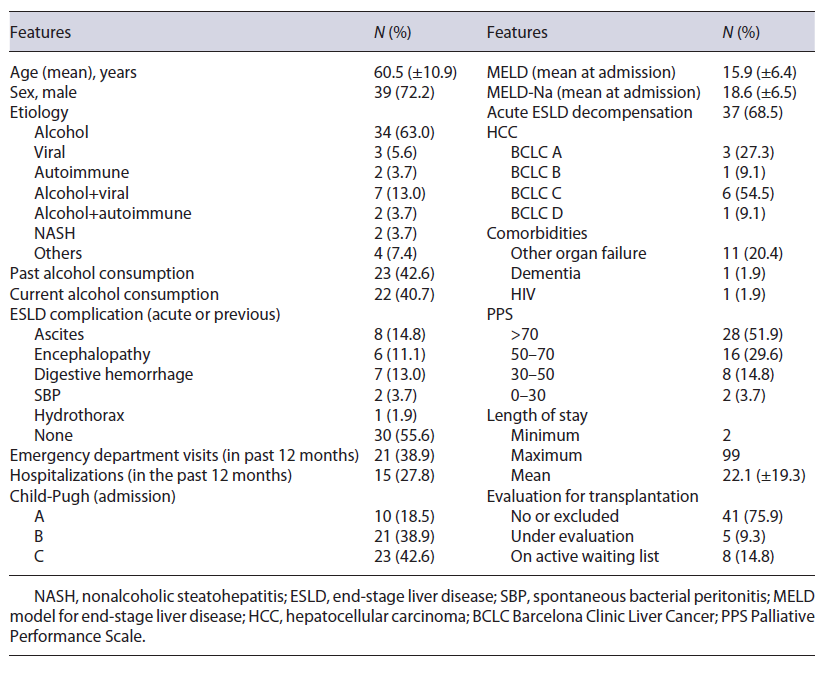
From initial 73 patients considered, 54 were included (Table 1), with a mean age of 60.5 years. Nineteen patients were excluded because of previous liver transplantation (n=7), isolated acute liver failure (n=2), another terminal disease (n=7) or impossibility of completing the assessment (n=3). Alcohol was the most frequent etiology of ESLD patients (79.6%, n=43), nine of these in association with another etiology. Twenty-two patients were consuming alcohol (40.7%). Twenty-four patients (44.4%) presented at least with one current or previous ESLD complication, most frequently ascites (14.8%, n=8), followed by gastrointestinal bleeding (13.0%, n=7) and encephalopathy (11.1%, n=6). Three patients presented encephalopathy West Haven [20] grade II or more, and their IPOS questionnaires were answered by their legal representative. Twenty-one patients (38.9%) had at least one emergency department visit in the past 12 months, and 27.7% (n = 15) had at least one hospitalization in the same period. About 2/3 of the patients (68.5%, n = 37) were admitted with acute decompensation episode of ESLD. Regarding prognosis scores, 81.5% (n = 44) were admitted on Child-Pugh B or C, with a mean of 9.0 ± 2.4 points and with a Model for ESLD (MELD) of 15, 9 ± 6.4 points, and MELD-Na of 18.6 ± 6.5 points, respectively. Eleven patients (20.4%) had HCC, almost 2/3 in Barcelona Clinic Liver Cancer (BCLC) stages C-D (n = 7). As to comorbidities, 11 patients (20.4%) presented with another associated organ failure (cardiac, renal, or respiratory). Most patients (51.9%, n = 28) presented PPS >70, even though 18.5% (n = 10) presented with significant level of dependence (PPS <50). Length of stay was on average 22.1 ± 19.3 days (minimum of 2 and maximum of 99 days).
Evaluation for Transplantation
Of the 54 patients, more than 3/4 had no evaluation for transplantation or had been already excluded from this proposal (n = 41, 75.9%), five (9.3%) were on active waiting list for transplantation and 8 (14.8%) under evaluation. One patient had been withdrawn from the list due to the development of multifocal HCC.
PC Needs Assessment
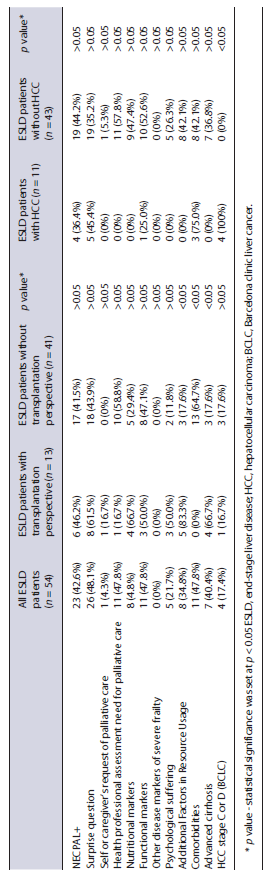
Regarding the Surprise Question “Would I be surprised if the patient died in the next 12 months?”, in almost half of the patients (48.1%, n = 26), the clinician would not be surprised (Table 2). NECPAL CCOMS-ICO© questionnaire identified 23 patients (n = 42.6%) as benefiting from PC. In those patients, the assessment of PC needs by clinicians, functional markers, and significant comorbidities were the most frequent criteria (47.8%, n = 11). PC recognition by patient versus by clinician was significantly higher in the latter (p<0.05), particularly in patients without transplantation perspective (0% vs. 58.8%).
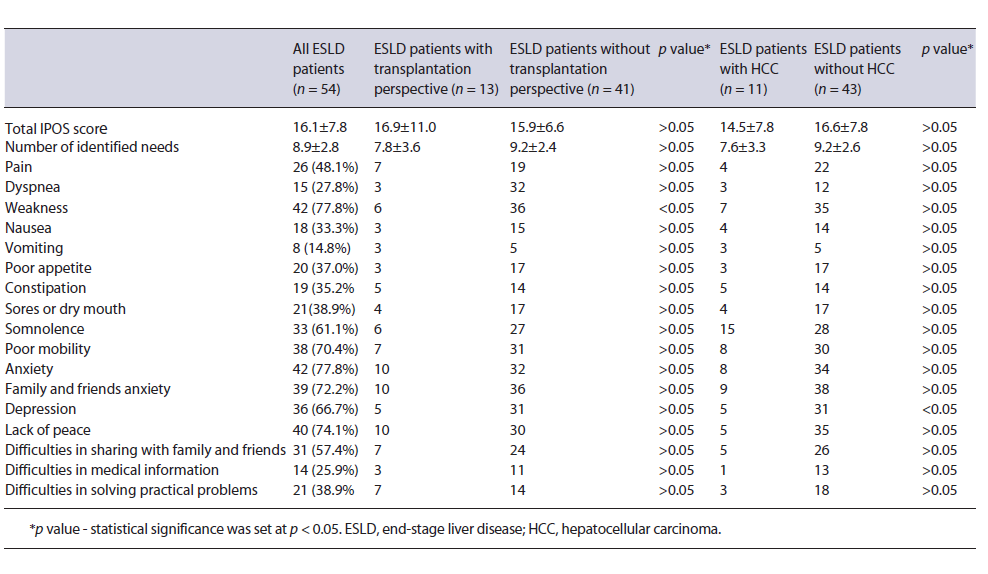
The IPOS questionnaire also revealed a different sort of needs (Table 3). On average, each patient identified about 9 needs (8.9 ± 2.8). Psychoemotional symptoms, as a group, were the most prevalent, firstly due to patient's anxiety (77.8%, n = 42), followed by family/friends’ anxiety (72.2%, n = 39) and depression (66.7%, n = 36). Concerning physical symptoms, weakness was the most prevalent (77.8%, n = 42), followed by reduced mobility (70.3%, n = 38), somnolence (61.1%, n=33), pain (48.1%, n = 26) and poor appetite (37.0%, n = 20). Regarding other needs, emphasis was placed on the lack of peace (74.1%, n = 40) and the difficulty in communicating with family/friends (57.4%, n = 31). In contrast, the difficulty in communicating with the medical team (25.9%, n = 14), assessed by access to medical information, was one of the least prevalent needs. Intensity evaluation of needs revealed that 43 (79.6%) patients had at least one severe need (intensity 3), and 19 (35.2%) at least one very severe (intensity 4). Finally, given that both questionnaires, NECPAL CCOMS-ICO© and IPOS, are based on different methodologies, it was found that patients with positive NECPAL CCOMS-ICO© had an average IPOS of 19.7 ± 8.5 (minimum of 7 and maximum of 41), while those with a negative NECPAL CCOMS-ICO© presented an average IPOS of 13.5 ± 6.2 (minimum of 1 and maximum of 26).
ESLD with and without Transplantation Perspective
Global PC needs assessed by NECPAL CCOMS-ICO© and IPOS revealed no significant differences between ESLD patients with and without transplantation prospect (Tables 2 and 3). However, regarding specific PC needs applying NECPAL CCOMS-ICO© questionnaire, the presence of comorbidities, advanced cirrhosis, and emergency department visit in the last 12 months were significantly more frequent (p<0.05) in patients without transplantation prospect. The IPOS questionnaire revealed a total score marginally higher in patients with transplantation prospect (16.9 ± 11.0 vs. 15.9 ± 6.6). Prevalence of specific needs according to this questionnaire came out as globally similar between groups, with weakness or lack of energy being the only ones significantly higher in patients without prospect for transplantation (p <0.05).
ESLD with and without HCC
ESLD patients with HCC were less frequently identified with PC needs (p>0.05) by NECPAL CCOMS-ICO© (Table 2). None of these patients identified psychological distress as other groups did. Presence of HCC was the only PC need that stood out. Regarding IPOS, ESLD patients with and without HCC showed no difference on the total IPOS score (14.5 ± 7.8 vs. 16.6 ± 7.8, respectively, with vs. without HCC patients) or on the mean number of PC needs (7.6 ± 3.3 vs. 9.2 ± 2.6, respectively, with vs. without HCC patients) (Table 3). Depression was the only PC need significantly more prevalent in patients without HCC (p<0.05).
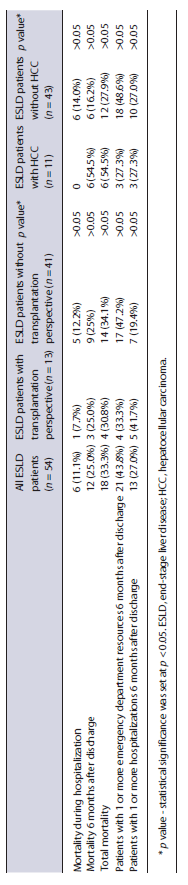
Subsequent Health Resource Use and Mortality Hospital mortality was 11.1% (n = 6), higher in the group of patients without transplantation prospect versus with (12.2 vs. 7.7%) and in patients without HCC versus with (14.0% vs. 0), but in both cases p> 0.05 (Table 4). Follow-up by the PC team occurred only in 4 patients, all of whom died during hospitalization. Six months after discharge, mortality increased to 33.3% (n = 18), particularly in the group of HCC patients (54.5%, n = 6). In the same period, 21 (43.8%) of the patients that were discharged alive went to the emergency department at least once and 27.0% (n = 13) required at least one subsequent hospitalization.
Discussion
All the ESLD patients included in this study, including ESLD patients with transplantation prospect, presented with PC needs, assessed either by the NECPAL CCOMS-ICO© or the IPOS questionnaires. The NECPAL CCOMS-ICO© questionnaire, which refers to information provided by the healthcare professional, reassured this through the Surprise Question, in which almost half of the patients (48.1%, n = 26) scored, and by 42.6% (n = 23) of patients that also had a positive final score. Regarding the criteria identified by this questionnaire, the recognition of PC needs by the clinician (47.8%, n = 11) stands out, as opposed to the recognition by the patients themselves (4.3%, n = 1) (p < 0.05). This difference might be a consequence of a lack of information about their prognosis or PC, insufficient communication with the health care team, or of limitations of the questionnaire itself to assess this dimension. Of the remaining criteria, the most frequently identified were the functional ones, followed by the presence of comorbidities and Child-Pugh C stage. IPOS questionnaire, which directly assesses PC needs by the patient or care-giver, identified psychoemotional needs as the most prevalent, namely patient's anxiety (77.8%, n = 42). Of the remaining needs, the spiritual dimension assessed through the feeling of peace was also relevant for 74.1% (n = 40). In contrast, communication with the health care team was a problem pointed out by only 25.9% (n = 14) of the patients.
This study broadens the knowledge about the PC needs of patients with ESLD, in different contexts, including patients with transplantation prospect as suggested by few other studies [9, 22]. Similar to the study published by Carvalho et al. [12], this study reassures, through the NECPAL CCOMS-ICO© questionnaire, a high prevalence of PC needs in the hospitalized ESLD patients. To our knowledge, no previous studies have suggested that patients with ESLD themselves fail to identify their need for PC, so these findings must be further researched. Through the IPOS questionnaire, this study also suggests the notion that more often several needs are dealt with simultaneously (average of 8.9 ± 2.8): more than – of the patients (79.6%, n = 43) had at least one severe need and about 1/3 (35.2%, n = 19) of the patients had a very severe one.
The symptoms identified more frequently - weakness (77.8%), reduced mobility (70.3%), somnolence (61.1%), and pain (48.1%) - are in line with those described by Peng et al. [4]. Similarly, the psychoemotional symptoms of depression (66.7%) and anxiety (77.8%) were very common, the latter more frequent than previously described by Peng et al. [4]. This result, combined with the needs identified in the spiritual domain, relevant in 74.1% (n = 40) of the patients, suggests an important psychoemotional and existential suffering in this population, an aspect that deserves to be better clarified and supported. Contrary to what was described by Low et al. [23], who identified the existence of significant communication difficulties among patients with ESLD, their families, and healthcare professionals, this was not observed in the present study, being pointed out by only 25.9% (n = 14) of the patients. However, this result must be carefully analyzed, namely if we consider the aforementioned psychoemotional and existential suffering described that can denounce communication deficiencies. A more careful assessment of communication needs may be justified. Comparing the results obtained by the two questionnaires, in addition to the fact that all patients with positive NECPAL CCOMS-ICO© scored in the IPOS questionnaire, it was also found that even patients with negative NECPAL CCOMS-ICO©, also scored at least one in the IPOS questionnaire, revealing that they had at least one need/problem that fits in the palliative scope. This result is not surprising given the different methodologies associated with each questionnaire, as well as the diversity of needs/problems identified, and their high prevalence also reported by Peng et al. [4]. The use of both these instruments might complement each other and suggests that frequently patients with still negative NECPAL CCOMS-ICO© might already present some PC needs, identified by IPOS.
Analysis by groups showed no statistically significant difference in the total scores of the NECPAL CCOMS-ICO© and IPOS questionnaires. These results suggest that even patients with ESLD with transplantation pros-pect also have important PC needs, as described by Baumann et al. [22], who showed the benefit of an early PC intervention in these patients. In the present study, there was a lower tendency for positive NECPAL CCOMS-ICO© and IPOS scores in the group of patients with HCC versus without. These results are probably because most of the patients with HCC have been admitted for elective procedures, without criteria for acute liver decompensation. Regarding specific criteria, the use of health care services in the 12 months prior to hospitalization, the presence of comorbidities, advanced cirrhosis, and symptoms like weakness and depression, were significantly higher in ESLD patients without perspective for transplantation. This is probably in agreement with greater clinical deterioration of these patients compared to patients with transplantation perspective. When comparing specific criteria of PC needs in patients with HCC versus without HCC, depression came out as the only significantly more prevalent symptom in patients without HCC, probably for the reason mentioned previously. Yet, these results suggest that ESLD itself poses no less need for PC than HCC associated to ESLD, as is sometimes supposed.
Limitations
This study presents some limitations. The sample con-sisted of patients admitted to a single hospital, even though it includes patients with some geographical diversity, as it is a liver transplantation center. The recruitment of patients was conditioned in terms of time and access to patients because it occurred in overlap with the SARS-CoV-2 pandemic, resulting in a prolonged recruitment period and in a sample of 54 patients. This sample also presented with a heterogeneous distribution among the subgroups considered, and this may also introduce some analysis bias. Finally, PC needs assessment, as it is evaluated in a single mo-ment, does not allow to reflect their dynamical nature.
Issues for the Future
For future research, it will be relevant to evaluate methodologies that allow for the access of different groups of patients with ESLD to PC, including patients with transplantation prospect, identifying the main needs and barriers to its implementation and allowing this access to occur as early as desirable [24].
Conclusion
The present study affirms important PC needs in patients with ESLD. It amplifies the knowledge about these, suggesting that most patients present several needs simultaneously, often of severe or very severe intensity and with wide diversity. Of the identified symptoms, psychoemotional ones stand out, as they are no less frequent than weakness, reduced mobility, and pain, which seem to be the most frequent physical symptoms. This study also found no relevant difference between the different subgroups of patients considered and, therefore, points out that PC is relevant in most patients with ESLD, including those with transplantation prospect.