A 75-year-old woman with arterial hypertension and dyslipidemia was hospitalized in the Gynecology Department after transvaginal hysterectomy with anterior colporrhaphy due to grade IV hysterocele and cystocele. One week after the surgical procedure, the patient developed constipation, associated with abundant rectal bleeding and hypotension (90/55 mm Hg), without associated tachycardia. The patient reported no abdominal pain. There was no history of antiplatelet or anticoagulant agents’ usage.
Analytically, a de novo microcytic anemia was detected, with hemoglobin levels of 8.4 g/dL (previously available value was 12.2 g/dL). Coagulation tests were normal.
In the setting of an acute lower gastrointestinal bleeding, an urgent colonoscopy after bowel preparation was conducted. Proctologic examination was normal. On digital rectal examination, a soft bulge was felt on the distal rectum, with bright blood being detected. On colonoscopy, a voluminous bulge (approximately 60 × 55 mm) with a congestive appearance was seen in the distal rectum, with a 10-mm orifice being evident on its surface (Fig. 1). Inside this orifice, there was abundant coagulated hematic content, which could not be aspirated. This bulge was passable by the conventional colonoscope, without resistance. There were no other relevant endoscopic findings throughout the colon.
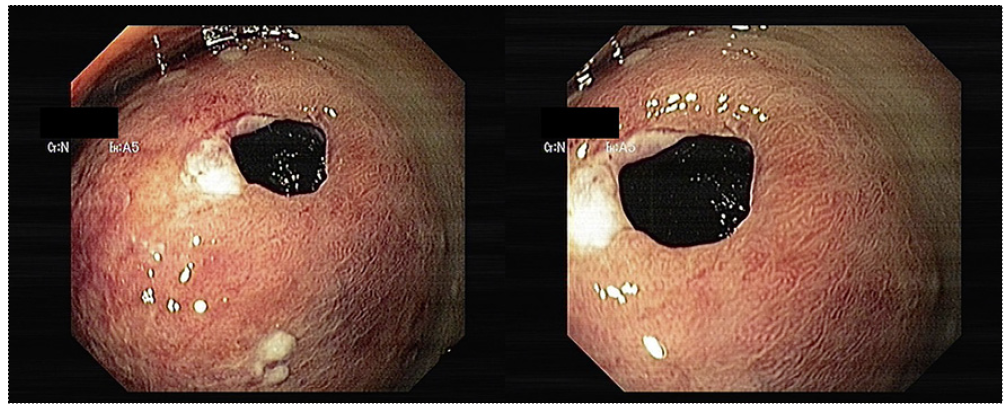
Fig. 1 Endoscopic images showing a voluminous bulge (approximately 60 × 55 mm) with a congestive appearance seen in the distal rectum, with a 10-mm orifice being evident on its surface, compatible with a rectal hematoma.
An abdominal and pelvic computerized tomography was performed, revealing an intramural collection containing hydroaeric levels in the right rectal wall, with a maximum diameter of 7 cm, compressing the rectal lumen (Fig. 2). The lower gastrointestinal bleeding and endoscopic findings were thus interpreted in the context of a rectal mural hematoma, communicating with the rectal lumen. The patient under-went conservative treatment, with complete reabsorption of the hematoma 2 months after surgery, which was confirmed by cross-sectional imaging and colonoscopy (Fig. 3).
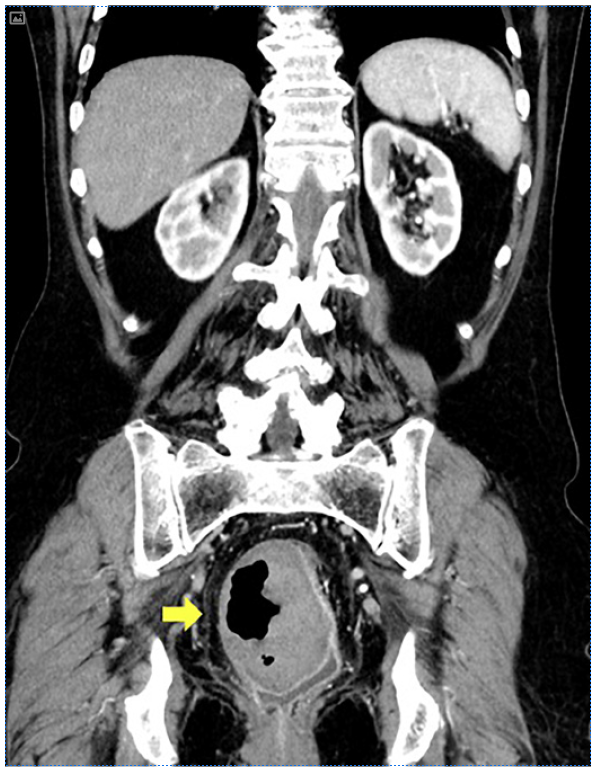
Fig. 2 Abdominal and pelvic computerized tomography revealing an intramural collection containing hydroaeric levels in the right rectal wall, with a maximum diameter of 7 cm, compressing the rectal lumen.
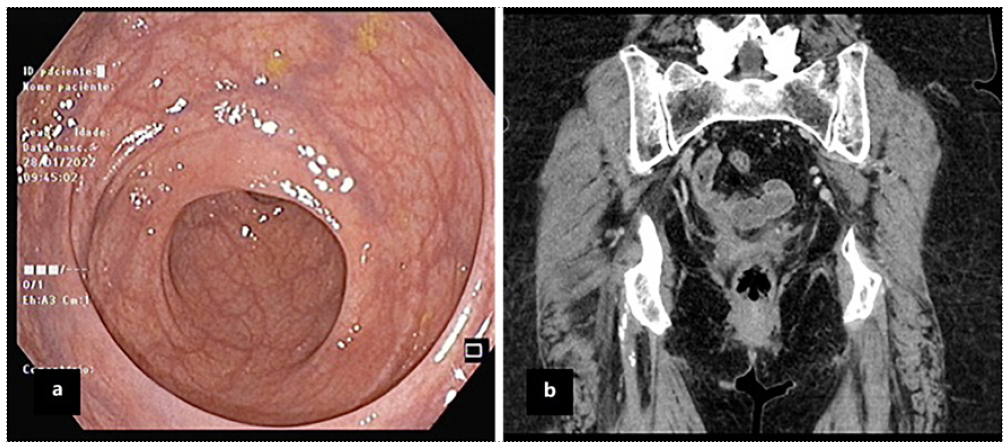
Fig. 3 Colonoscopy (a) and computed tomography (b) images confirming complete rectal hematoma resolution.
Small pelvic hematomas are a common finding after transvaginal hysterectomy, occurring in more than 25%of the performed surgeries [1]. Nevertheless, most of these are asymptomatic, being accidentally detected in scheduled follow-up ultrasounds. Furthermore, hematomas most frequently form in dependent areas, such as the pouch of Douglas, sub-vesical space, or ischium-rectal fossa [2]. Treatment consists of antibiotics if infected, with or without percutaneous or surgical drainage according to clinical evolution [1].
To our knowledge, this is the first case reporting a symptomatic rectal hematoma after gynecological surgery. With this clinical case, we aim to highlight an unusual etiology of lower gastrointestinal bleeding, associated with unique endoscopic findings, as well as to emphasize the importance of investigating medical and surgical history in patients with acute rectal bleeding.














