Introduction
Cervical cancer (CC) is the third most common neoplasia and is one of the main causes of death due to cancer among European women of reproductive age (15-49 years old) 1. In Portugal, the age-standardized mortality rate due to CC was 3.2/100,000 women in 2020 and, although there has been a decrease among young women, there is no evidence of decreasing mortality due to CC among women aged 50 years or more 2.
The main determinant of CC is the infection with oncogenic types of human papillomavirus (HPV) 3. Although a large proportion of HPV infections are transient, the persistent infection will result in cervical intraepithelial neoplasia and, if left untreated, these lesions will progress to invasive CC 3. Advanced stages of CC and their treatment are related to low survival rate 4, severe outcomes that compromise the quality of life among survivors 5 and high economic burden related to medical care costs 6.
Screening can detect low-grade cervical intraepithelial neoplasia that can be monitored or even easily treated a long time before the development of invasive CC 7, playing a valuable role in the field of public health. The available evidence supports the effectiveness of cervical screening in reducing the incidence of advanced CC 8 and the mortality due to CC, having been estimated that 83% of deaths could be prevented if everyone attended screening regularly 9. Therefore, the access and the adherence to regular cervical screening have a relevant impact in reducing the incidence of and mortality due to CC.
Population-based CC screening programmes have been implemented in Portugal covering 70% of eligible women in 2016 10. Between 2014 and 2016, CC screening adherence rates observed in Portugal increased from 50% to almost 90%. However, such rates present large variability between geographic regions, with the lowest rate in Northeast Portugal (61%) 10. Low rates of adherence to population-based CC screening programmes suggests that there is a proportion of under-screened or even unscreened women.
According to the new European Guidelines for Quality Assurance in Cervical Cancer Screening, women should be screened with cervical cytology every 3-5 years or every 5 years by HPV testing up to age 60 or 65 years 11, 12. In Portugal, population-based CC screening programmes have been carried out following these new recommendations 10.
As regular attendance to CC screening is the main factor in preventing CC 8, 9, no use or underuse of CC screening is a matter of concern and should be prevented. On the other hand, the overuse of screening increases healthcare costs without improving patient outcomes and it should also be avoided 13.
Beyond sociodemographic characteristics, such as age 14, parity 14-16, marital status 14-16 or education level 14, the women’s knowledge about risk factors and prevention of CC has been considered an important issue in increasing the rate of adherence to CC screening 15-18. However, women’s behaviour towards CC screening has also been related to the access to healthcare services and to the attitude of primary care providers with regard to screening uptake 19-21. Furthermore, invitation and reminder letters from primary healthcare services have been effective in increasing CC screening adherence 19,21. Understanding how such factors affect the underuse and the overuse of CC screening is an important issue in improving the effectiveness of CC screening where there is low adherence to guideline-consistent CC screening.
Therefore, we aimed to come to know the predictors of being never/under-screened and over-screened in CC screening among patients of two primary healthcare services in Northeast Portugal.
Materials and Methods
Study Setting and Sampling Procedures
This is a part of a larger cross-sectional descriptive survey carried out in two public health centres in Northeast Portugal, serving a population of 35,341 inhabitants from which 52% (n = 18,375) are women, 43% of them (n = 7,856) being at reproductive age 22. Similar to other Portuguese regions, there is a population-based screening programme 10. However, there is also a private healthcare market, with services mainly offered by gynaecologists.
The study took place between October 2017 and June 2018. Nursing students on duty were previously trained as focal points and they were responsible for sampling procedures and data collection.
For this survey, a convenience sample was assembled. All women aged between 18 and 70 years with an appointment as a patient or as the companion of a patient, in each one of the public health centres, were eligible for the study. Women were invited to participate, they received an explanation about the protocol of the study, and those who signed the informed consent (n = 1,093) were enrolled in the study. According to the Portuguese Ministry of Health, the target population for organized CC screening are women aged between 25 and 60 years 10. Therefore, 764 women were included in this analysis, after excluding participants aged less than 25 years (n = 266) or more than 60 years (n = 43) and those with data missing for age (n = 20).
The study was approved on 25th October 2017 by the Ethics Committee of the Unidade Local de Saúde do Nordeste, Bragança, Portugal, where the study was conducted (number 006485).
Data Collection
Data collection was based on a face-to-face interview to fill a structured questionnaire prepared for this proposal. The questionnaire covered the following topics: (1) sociodemographics, (2) use of health services, (3) frequency of CC screening and reasons underlying such frequency, (4) assessment of CC health literacy, and (5) satisfaction with organized CC screening. The analysis reported here was based on topics 1-4. The CC health literacy was assessed by using the Cervical Cancer Literacy Assessment Tool (CCLAT), which is a 24-items instrument 23. The answers to each one of the items were classified as a correct or incorrect response. The participant received one point for each correct answer and zero points for incorrect answers. Therefore, the total score ranged from 0 to 24 with higher scores indicating higher CC health literacy. Permission to use the CCLAT was approved by the author of the questionnaire.
Variables
The outcome of interest is the frequency of CC screening. Women were classified according to the frequency of CC screening into 5 groups: never having CC screening, irregular/sporadic CC screening, regular screening interval of 3 or more years, regular screening interval less than 3 years with no previous suspicious screening and regular screening interval less than 3 years with previous suspicious screening. Reasons underlying the frequency of CC screening were obtained. Following guidelines 10-12, for statistical analysis, women were regrouped by frequency of CC screening into 3 groups: guideline-consistent screened (regular screening interval of 3 or more years and those with regular screening interval less than 3 years but with previous suspicious screening), over-screened (regular screening interval less than 3 years with no previous suspicious screening) and unscreened/under-screened women (which includes those never having CC screening as well as women who reported sporadic/irregular screening).
The following factors were used as possible explanatory variables of the frequency of CC screening: age, marital status (with and without a companion), education level (<10, 10-12 and >12 schooling years), previous pregnancies (none and at least 1), frequency of consulting primary care physician (never/irregular and regular visits), family planning attendance (yes or no), being beneficiary of health subsystem other than national health system (yes or no), who recommended/prescribed CC screening (primary healthcare physician, primary healthcare nurse, primary healthcare physician and nurse, gynaecologist, or primary healthcare and gynaecologist), screening through health centre invitation (yes or no) and level of CC health literacy assessed by CCLAT (score ranges between 0 and 24).
Statistical Analyses
A descriptive analysis of the sample was performed. Two multivariate logistic regression models were conducted to assess the effect of the explanatory variables on the outcome of interest. One model assessed determinants of being unscreened/under-screened and the other model assessed determinants of being over-screened. In both models, the comparison group included women with guideline-consistent CC screening. All possible explanatory variables were entered into the logistic regression model assessing determinants of being over-screened, but the variables “who recommended/prescribed CC screening” and “screening through health centre invitation” were not considered when assessing determinants of being unscreened/under-screened because such information was not applicable to unscreened women. A backward deletion procedure was carried out to retain those variables that were significant. The significance level was set at 0.05. Adjusted odds ratio (OR) and respective 95% confidence interval (95% CI) were obtained.
Results
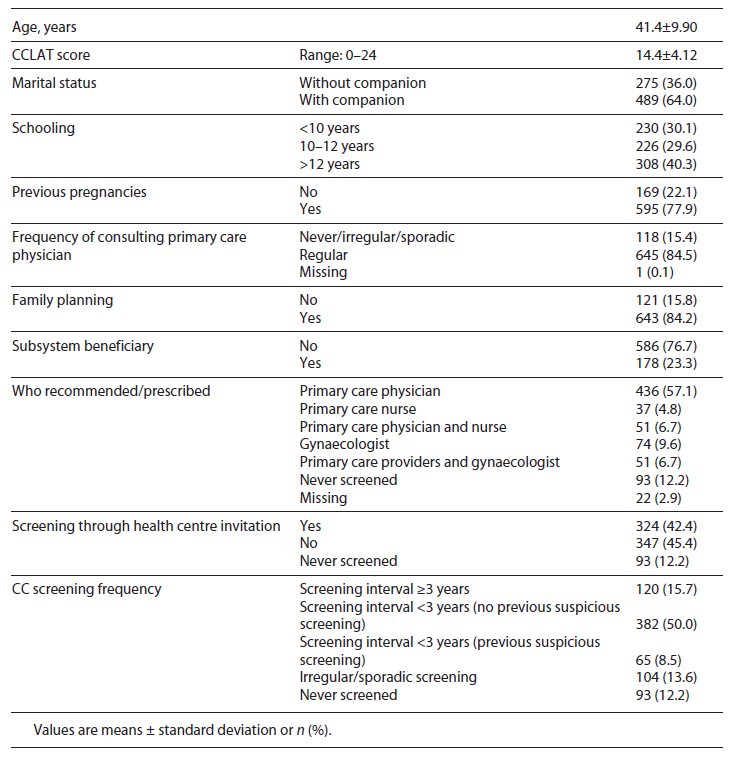
Table 1 shows the demographic characteristics and the pattern of healthcare services usage among the participants included in the present analysis. Out of all 764 women included in the present analysis, 93 (12.2%) reported that they had never undergone a CC screening during their lifetime, 104 (13.6%) reported underuse and 382 (50.0%) reported regular screening interval less than 3 years with no previous suspicious screening. The mean age of the participants was 41.4 (±9.90) years and the mean score of CCLAT was 14.4 (±4.12). The majority of women reported to have a partner (n = 489; 64.0%), a previous pregnancy (n = 595; 77.9%), regular frequency of consulting a primary care physician (n = 645; 84.5%), family planning attendance (n = 643; 84.2%) and CC screening recommendation/prescription by a primary care physician (n = 436; 57.1%).
With regard to the reasons underlying attitudes towards CC screening (Fig. 1), 52.2% of over-screened women and 44.2% of under-screened women reported that their screening frequency was based on healthcare provider prescription. Women with previous suspicious screening corresponded to only 15% of women with regular screening intervals less than 3 years. Moreover, 60.2% of unscreened women reported that no one prescribed the CC screening.
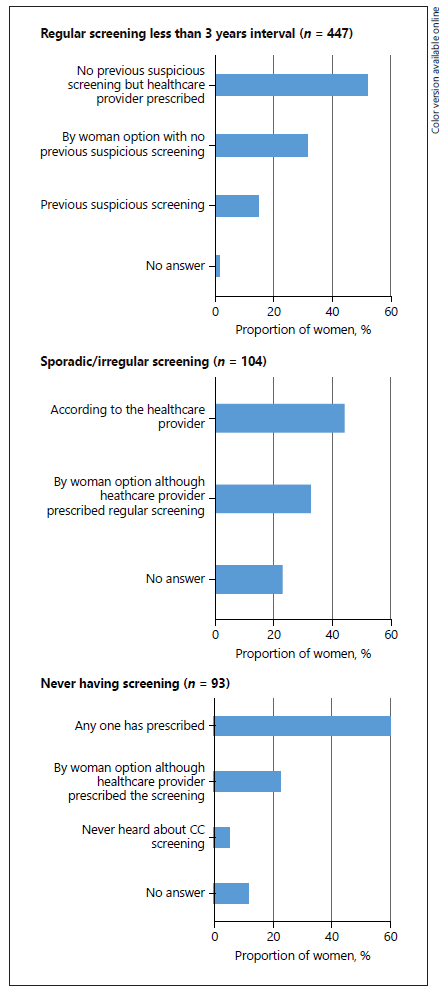
Fig. 1 Distribution of women according to the reasons underlying their attitudes towards CC screening.
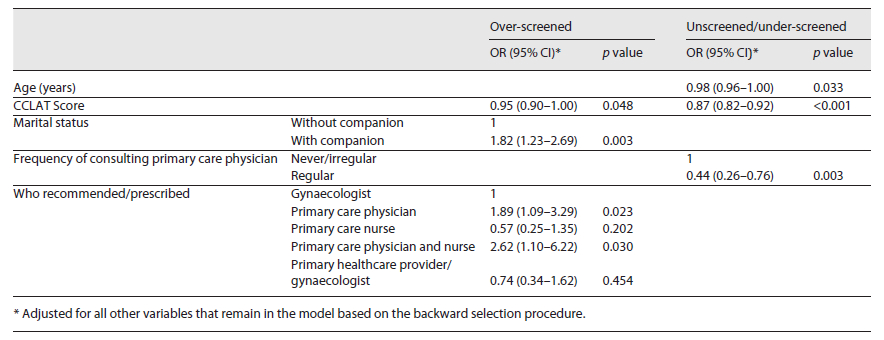
The results of multivariate regression models are presented in Table 2. Regular visits with primary care physicians (OR = 0.44; 95% CI: 0.26-0.76) and higher age (OR = 0.98; 95% CI: 0.96-1.00) reduced the odds of being unscreened/under-screened. On the other hand, women who reported to have a partner (OR = 1.82; 95% CI: 1.23-2.69) and those who received prescription/recommendation for CC screening from primary care physicians (OR = 1.89; 95% CI: 1.09-3.29) or both primary care physicians and nurse (OR = 2.62; 95% CI: 1.10-6.22) were more likely to be over-screened than those who received prescription/recommendation from the gynaecologist. The increase in CCLAT score has a protective effect for being unscreened/under-screened (OR = 0.87; 95% CI: 0.82-0.92) and for being over-screened (OR = 0.95; 95% CI: 0.90-1.00).
Discussion
This study aimed to understand the factors underlying the underuse/no use and the overuse of CC screening among women aged between 25 and 60 years. A noteworthy finding is that 25% of women reported never having or having sporadic/irregular CC screening. The majority of women never having CC screening reported that no one prescribed the test. Furthermore, a large proportion of under-screened or over-screened women reported that their CC screening frequency was based on healthcare provider prescription. A regular visit with a primary care physician appeared as a protective factor against never/under-screening. On the other hand, women who reported prescription/recommendation of CC screening by primary care physicians were more likely to be over-screened. A higher level of CC health literacy appeared as a protective factor for being unscreened/under-screened and over-screened in CC screening.
Primary healthcare is crucial to improving the level of care in the community, based on equitable distribution of healthcare along the continuum, from health promotion and disease prevention to treatment and rehabilitation 24. The skill mix profile of primary care is based on multidisciplinary teams where the primary healthcare physician plays an essential role in addressing generalized whole-person care based on patient-centred care models 25. Previous research has reported that women’s CC screening adherence is influenced by primary healthcare providers 19-21. Women invited by their general practitioner are more likely to undergo screening 20,21, and women who have no access to primary care physicians are more likely not to have recently been screened 14. Following previous research, our findings highlight the protective role of regular visits to family physicians against being unscreened or under-screened.
However, our findings also showed that the majority of unscreened women did not undergo screening because no one prescribed it and a large proportion of under-screened women stated that their screening frequency was based on healthcare provider prescription. According to these findings, there is room for improvement of adherence to regular CC screening through primary care providers. Indeed, out of all unscreened or under-screened participants, 70% reported regular visits with primary care physicians and family planning attendance. Therefore, primary healthcare providers should increase awareness for prompting women regarding regular screening.
Current guidelines recommend screening at every 3 or every 5 years, depending on the type of test (cervical cytology or HPV testing). The decrease in screening interval did not improve the protection against CC but increased the demands for screening, the risk of anxiety and overtreatment due to the false-positive results, also increasing health costs 13. However, our findings showed a high proportion (50%) of participants having regular screening intervals less than 3 years with no previous suspicious screening (over-screened women). Previous research has reported that defensive medical practice is one of the main reasons underlying the overuse of medical procedures, therapeutic approaches and diagnostic tests, and it has a strong impact on health costs 26. It has also been reported that physicians tend to overestimate the benefits and underestimate the harms of medical interventions, including cancer screening, leading to an increase in such procedures 27. Fear of missing an invasive CC, patient concerns, as well as the limited time to explain the risk and benefits of increasing the time interval between screenings are barriers to following CC screening guidelines 28,29. Further research is important to know whether such factors could explain the high rates of being over-screened that we observed, as one-half of these participants reported that their screening frequency was according to the healthcare provider prescription.
According to our results, the women reporting recommendation/prescription of CC screening by primary healthcare physicians were more likely to be over-screened. Previous research conducted in other settings has reported that general practitioners could have concerns with regard to patient preferences to reassure the patient 30, and sometimes they could feel pressured because of an increasing request from patients for medical examinations 31. Such circumstances drive clinical options 30,31 and they could be possible reasons underlying our results.
Our results showed that the increase in CC health literacy prevents women from being under-screened as well as from being over-screened. These findings are in line with previous research where the level of knowledge on CC risk factors and CC prevention procedures appeared as a driver of women’s adherence to CC screening, with important implications for public health 15,16,17 18. The role of health literacy in increasing people’s involvement to make more informed decisions about their health has been highlighted 32. A preventive strategy focused on increasing women’s knowledge seems to be a key issue to improve the use of CC screening. Primary healthcare providers could play a valuable role in this task.
Our study has some limitations. First, our analysis was based on a convenience sample. The sample was obtained by asking women who went to the health centre due to an appointment for them or their relatives, rather than by randomly drawing them from all women registered in each health centre. As younger women are more likely to take care of children, parents, or other relatives, the mean age we observed in our sample was lower than we would expect in the whole population. Second, the rate of regular screening reported by the participants was higher (75%) than the rate reported by the official data for the region (51%) 33. This is a usual problem in studies of attendance, probably because more conscientious women and those who participate in screening programmes are also more prone to participate in a survey 16. However, this could also be explained based on the convenience sample we used. Third, our data relies on self-reported information that could be inaccurate and sometimes could vary according to women’s literacy. Fourth, our sampling procedure makes the inclusion of women who are not patients of primary healthcare services unfeasible. Therefore, the representativeness of our sample was compromised. In spite of these limitations, to the best of our knowledge, this is the first study assessing the underuse and overuse of CC screening in our setting and may give insights into factors underlying such attitudes.
Conclusion
In summary, we observed concerning rates of over-screened and unscreened/under-screened women in our setting where a population-based CC screening programme has been implemented according to the European guidelines. Public health campaigns focused on increasing CC health literacy are needed to maximize the use of CC screening. Primary healthcare providers should be available to give information and to motivate patients with regard to a guideline-consistent use of CC screening.
Acknowledgement
We thank the Directors of both public health centres for their support in women’s recruitment and data collection. We thank the nursing students who were responsible for the women’s recruitment and face-to-face interviews.
Statement of Ethics
This study protocol was reviewed and approved on 25th October 2017 by the Ethics Committee of the Unidade Local de Saúde do Nordeste, Bragança, Portugal, where the study was conducted (number 006485). Written informed consent to participate in this study was obtained from all participants.