Case report
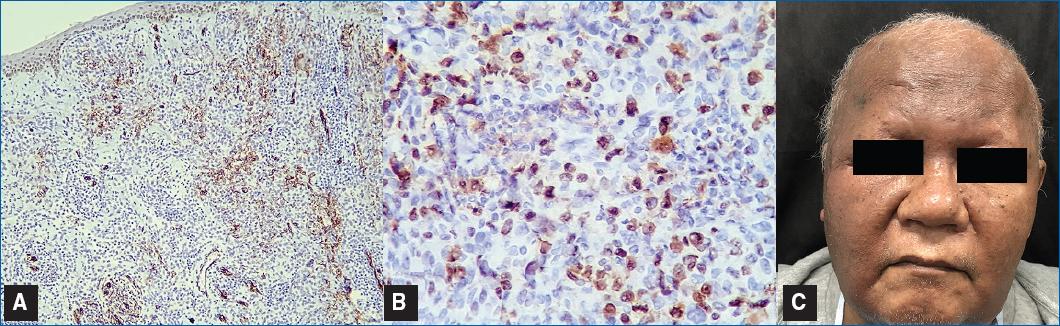
A 72-year-old man with hypertension and Parkinson’s disease under oral anticoagulants presented with erythematous papules and periorbital edema on the right hemiface associated with an hyperchromic and pruritic infiltrated plaque in the right frontotemporal region (Fig. 1A), which began two months after a fall and local trauma. Within about one month after the first observation, the lesion progressed with nodule formation, extensive erythematous and violaceous infiltration involving the whole right hemiface and neck, with eyelid edema causing loss of visual capacity (Fig. 1B), but with no associated local or systemic symptoms.
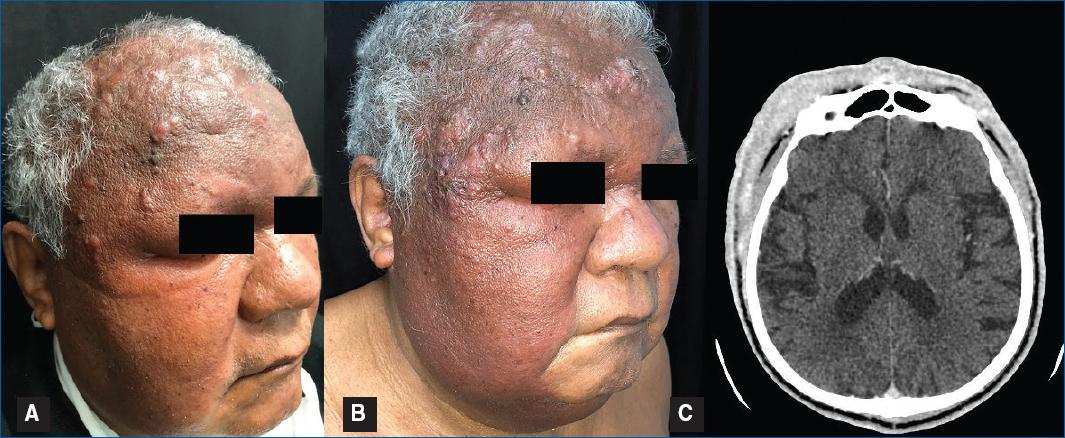
Figure 1 Erythematous-violaceous infiltration on the forehead that evolved to the entire face with the aspect of cellulitis (A, B), that on CT showed proliferation of extracranial soft tissues (C).
All routine laboratory tests were normal. Differential diagnoses could be Virchowian leprosy with lepromas, facial cellulitis, persistent hematoma and mycosis fungoides. Computed tomography (CT) of the neck did not detect cervical lymphadenopathy. Parotid CT scan did not reveal any atypical findings. Cranial CT revealed an increase in soft tissues associated with skin thickening, affecting the frontotemporal and nasoperiorbital regions, especially on the right, with no evidence of collections in the contrast-free study (Fig. 1C).
Histopathology revealed preserved epidermis and diffuse proliferation of atypical epithelioid cells forming masses in the dermis, in addition to vascular channels with bizarre shapes and atypical endothelium (Fig. 1A,B,C). Histopathological differential diagnoses included metastatic carcinoma, sarcoma, melanoma, anaplastic large cell lymphoma, angiosarcoma and other vascular neoplasms. Immunohistochemistry was positive for CD34 (clone QBEnd/10) in multiple vascular channel endothelium and strongly positive for ki67 (clone MIB-1) (Fig. 2A,B) and negative for Cytokeratin Pan (clone AE1AE3), Protein S-100 (clone POLYCLONAL), Carcinoembryonic Antigen–CEA (clone II-7), P63 (clone DAK-P63), and Smooth muscle actin (clone 1A4), therefore confirming the diagnosis of epithelioid angiosarcoma.
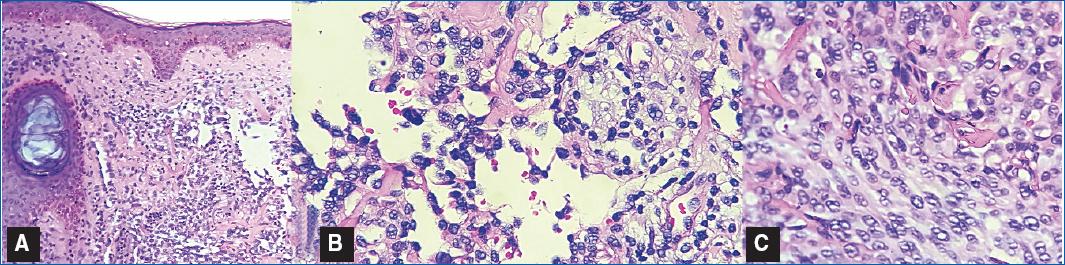
Figure 2 Histopathology showing irregularly shaped anastomosing vascular channels with the presence of atypical endothelial cells infiltrating the dermis (H&E-10x) (A) and proliferation of slit-like vessels filled with neoplastic endothelial cells (B). Detail of atypical multinuclear endothelial cells (H&E-40x) (C).
Thoracoabdominal and pelvis CT did not identify metastasis. The patient underwent chemotherapy with paclitaxel (175mg/m2) every 21 days, resulting in a significant improvement in quality of life with return of visual acuity after 2 sessions. After the first cycle, the patient suffered total alopecia and there was a cutaneous bacterial facial infection, with no laboratory alterations, controlled with oral antibiotics. The patient reported nausea and vomiting as the most common adverse event. We have observed a good clinical response after the third cycle of chemotherapy (Fig. 3C). The patient had a significant improvement after completing six chemotherapy cycles and unfortunately died of COVID-19 infection.
Discussion
Epithelioid angiosarcomas are rare and rapidly progressing malignant neoplasms that may clinically resemble hematoma. They may present as erythematous and violaceous nodules, papules, and plaques that can bleed or ulcerate. They typically appear in sun-exposed areas, mainly on the scalp and face, mostly in caucasian men, older than 70 years old. Angiossarcomas can also be associated with chronic lymphedema (Stewart-Treves syndrome) and radiotherapy, particularly in patients undergoing breast cancer treatment1,2.
Tumor genesis is associated with TP53 tumor suppressor gene suppression and mutations in the PTPRB and PLCG1 genes, which promote angiogenesis. New studies are trying to correlate UV exposition to angiosarcomas development.
The prognosis is poor, with a low five-year survival rate. Generally, patients who have smaller lesions that can be treated with surgical resection and prospective radiotherapy have the best overall survivor rates. However, there are available treatments, with doxorubicin-based regimens and other immunotherapeutic and chemotherapeutic drugs. Furthermore, there are reports of success with paclitaxel, isolated as in the present case, or associated with bevacizumab with or without associated with the use of propranolol3. Moreover, propranolol appears as a possible drug to be associated during treatment as it plays a role in stopping tumoral growth. The use of paclitaxel plus propranolol and radiotherapy seems to be one of the best options to treat extensive angiosarcomas nowadays4,5. Bevacizumab and other immunotherapeutic drugs appear as a secondary line of treatment and their clinical importance still needs to be evaluated in biggest studies6.