Introduction
Scurvy is a pathology caused by vitamin C deficit, currently uncommon when it is compared to other nutritional disorders1,2 and it is rarely suspected leading to delay in its diagnosis3,4.
Scurvy is one of humanity's oldest diseases. It was first described in the Ebers papyrus, written approximately 1500 BC. Seeing whole groups of people in monasteries, within families, aboard ships, and armies afflicted with the disease, ancient writers developed multiple and varying theories regarding its etiology. Sailors were among the most affected victims, mainly in the 15th century with the beginning of long journeys5.
British navy doctors assumed that citrus fruits such as lemons and oranges treated the disease6, but it was not until 1931 that biochemist Albert Szent-Gyorgyi accidentally discovered a substance in lemons and oranges called “hexuronic” acid5,6. This was later related to the treatment of scurvy6.
Vitamin C (L-ascorbic acid or ascorbate) is an essential nutrient for all human beings and is closely related to the maintenance of intercellular connective tissues, osteoid, dentin, and collagen. It can regulate the inflammatory response, apart from the influencing of iron absorption4.
The clinical spectrum of scurvy is quite varied, including bone, hematological, dental, and dermatological manifestations such as petechiae and/or perifollicular purpura and follicular hyperkeratosis. The diagnosis is essentially clinical with detailed history, radiography, and laboratory tests to aid. Treatment consists of micronutrient replacement and dietary changes1,3.
In this case, we report a patient with poor eating habits with serious clinical repercussions who was later diagnosed with scurvy.
Case report
A 13-year-old female caucasian patient with a previous history of persistent ductus arteriosus treated as a newborn was admitted to the emergency room at “Hospital da Criança e Maternidade,” in São José do Rio Preto due to pain in the right hypochondrium, hypermenorrhea, and spots in the upper and lower limbs present for 3 weeks. Continued use of medications or allergies was denied. The patient is in good general condition, active, with adequate vital signs, and without alterations in the cardiopulmonary, abdominal, or neurological physical examination.
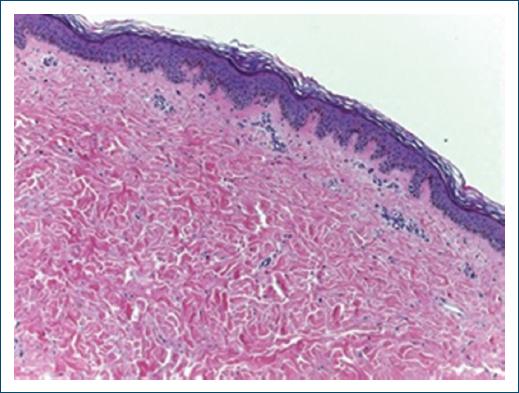
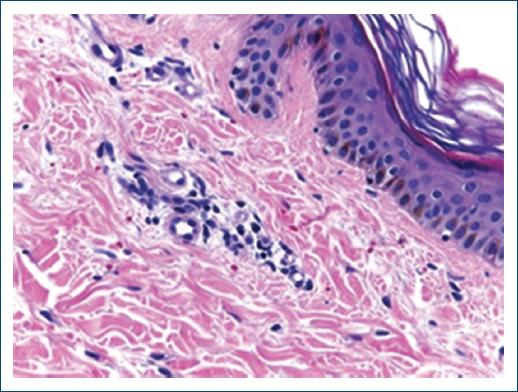
Upon dermatological examination, there were diffuse petechiae on the limbs, upper gingiva hypertrophy, and rough brownish punctiform papules disseminated on the face, limbs, and abdomen (Figs. 1-3). An incisional biopsy performed on the petechiae displayed a slight extravasation of red blood cells and hemosiderin deposits on the dermis and a mild lymphocytic inflammatory infiltrate around the vessels of the superficial plexus, compatible with non-inflammatory purpura (Figs. 4 and 5).
Complementary tests highlighted only hypochromic microcytic anemia and increased fibrinogen without any changes in platelets, coagulation or inflammatory parameters, liver and kidney function, and autoantibodies. A chest X-ray and an abdominal ultrasound showed no alterations.
The patient developed pain, ankle edema, and difficulty wandering, and bone X-ray showed tenuous rarefactions in the distal metaphysis of the tibia and fibula bilaterally and more subtle changes in the femur. Ultrasound of the ankles was suggestive of an edematous/inflammatory process of the skin and subcutaneous tissue.
The hematology team performed a myelogram to exclude a lymphoproliferative disease, which showed megakaryocytic hyperplasia suggestive of peripheral platelet destruction.
After a few days of hospitalization, the patient reported pain when eating and refusal of hospital food. On this occasion, the mother reported that the patient had an inadequate daily diet based on instant noodles and soft drinks. The nutritional assessment revealed an eutrophic child, but at nutritional risk with a very low serum dose of vitamin C: 0.08 mg/dL for the normal value of 0.50-1.50 mg/dL), thus diagnosing scurvy.
With vitamin C replacement, there was a gradual and complete resolution of the condition. In the first 2 weeks, cutaneous symptoms and almost all systemic symptoms cleared, whereas gingival hyperplasia showed partial improvement in the 1st month and resolution in 2 months. The patient continues to be monitored by the dermatology, nutrition, and pediatrics teams, with an improvement in dietary quality.
Discussion
Scurvy is a cutaneous and systemic disease caused by vitamin C deficiency, extremely rare nowadays, but it is one of the oldest diseases of humanity, with the first reports in ancient Egypt6.
L-ascorbic acid is an essential nutrient in the diet, found in vegetables and fruits, mainly in citrus fruits, green vegetables, potatoes, tomatoes, and cabbage. A daily intake of 10 mg/day of vitamin C is enough to keep body stores above 300 mg1,3. This nutrient participates in several physiological processes and its deficit can lead to inadequate wound healing, petechiae, follicular purpura that predominate in the lower limbs, corkscrew and curved hair, subungual hemorrhages, dental defects, and osteoblast function. It may lead to pseudoparalysis in children1,7.
Populations at risk of nutritional risk of vitamin C deficiency include the elderly, alcoholics, patients on restrictive diets, a total parenteral diet without supplementation, undergoing intestinal resections, or people who have malabsorption syndromes8,9.
The clinical diagnosis of scurvy is confirmed by the reduction of plasma levels of vitamin C below 0.2 mg/dL. Treatment consists of oral vitamin C replacement, with doses of 300 mg/g daily, until the resolution of the clinical picture1.
In a study by Blee et al., patients in the hospital or undergoing surgery may have borderline levels of vitamin C that can further decrease due to a lack of oral intake post-surgery or critical illnesses such as pancreatitis, sepsis, or multiple organ failure10. Furthermore, seven out of 12 patients who experienced widespread bleeding had poor oral nutrition before surgery.
Acute lameness, found in the pediatric population, maybe the musculoskeletal manifestation presented by scurvy due to severe malnutrition11, as in our patient. A systematic review conducted by Trapani et al. on scurvy in the pediatric population revealed that 90% of children suffered from musculoskeletal complaints such as arthritis and lower limb pain, whereas about 33% had a limp and/or refused to walk11,12. Ceglie et al. also reported three cases that began with leg pain, refusal to walk, and worsened over months. Two presented gingival hyperplasia and petechiae, another reported night sweats and gingival bleeding, but after the deficit was discovered and ascorbic acid was supplemented, there was an improvement in days with further improvement within weeks13, as in the present case.
In the current context, where consumption of ultra-processed foods with low nutritional value is increasing, scurvy is still a reality. It is a rare condition, but it must be remembered, especially if the risk factors are listed in the clinical history. Therefore, this report aims to recall the clinical and dermatological picture of scurvy. Classic findings in dermatological examination can help us with clinical reasoning, in addition to reinforcing the importance of questioning nutritional aspects in daily anamnesis.