Introduction
Mycosis fungoides (MF) is the most common type of cutaneous lymphoma and can be classified into distinct subtypes. Folliculotropic mycosis fungoides (FMF) is characterized by the folliculotropic infiltration of the epidermis by atypical T-cells, usually CD4+1. It represents 10% of all cases of MF2, is more frequent in men, and usually diagnosed between 46 and 59 years of age1.
The clinical manifestations of FMF are ample, making diagnosis a challenge. Because of this, delayed diagnosis is usual, ranging from 18 to 48 months after onset of symptoms1,3, which is particularly concerning when considering that response to treatment is worse than classical MF and depends on staging.
Head and neck involvement is present in the majority of patients1-3, and supraciliary lesions and alopecia are characteristic. These findings, associated with the histopathological presence of epidermal folliculotropic infiltration, make trichoscopic assessment of lesions appealing. Even so, there are few published papers documenting these trichoscopic findings.
Clinical case
We present the case of a 50-year-old man with a medical history of hepatitis B and C, medicated with tenofovir, who presented with a pruriginous disseminated dermatosis, affecting the head, neck, trunk, and limbs, characterized by erythematous patches and plaques with fine white-grayish scale, madarosis and multifocal patchy alopecia of the scalp (Fig. 1), and painless inguinal lymphadenopathies. Symptoms had started 1 year earlier and the first lesions appeared on the trunk.
Trichoscopy of the scalp (Fig. 2) revealed a decreased number of pilosebaceous units, with several dilated follicular openings (some with milky-white globules) with perifollicular accentuation, black dots, and some vellus hair and dystrophic hairs. White scaling in a widespread distribution, areas with dotted vessels, and spermatozoa-like vessels was also noted.
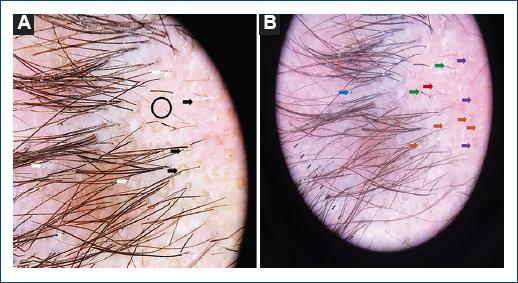
Figure 2 A: dilated follicular openings/yellow dots (black arrow), white scaling (white arrow), dotted vessels (black circle). B: decreased number of pilosebaceous units, milky white-globules (orange arrow), perifollicular accentuation (purple arrow), dystrophic hairs (green arrow), black dots (blue arrow), spermatozoa-like vessels (red arrow).
Hair and skin biopsies were compatible with FMF. Laboratory and imaging workup associated with lymph node biopsy led to a pT2bN0M0-IB staging. The patient was treated with acitretin and electron bath therapy and later with bexarotene and brentuximab. He later died of MRSA septic shock.
Discussion
Trichoscopy is an easy-to-use and non-invasive technique that allows the evaluation of the scalp and hair. At present, there is a lack of published data detailing these findings in FMF.
Sławińska et al.2 published a systematic review detailing the dermoscopic and trichoscopic findings of cutaneous lymphomas, including FMF. In MF, dermoscopy can reveal spermatozoa-like vessels (first described by Lallas et al.4), which seem to be a somewhat specific finding2. This type of vessel was also present in our patient and is thought to represent the proliferation of vascular cells in dermal papillae (translating, in dermoscopy and trichoscopy, into a round shape) and through the underlying dermis (corresponding to the linear portion of the vessels)5.
Gallo et al. published the biggest series of trichoscopic findings in FMF patients with scalp involvment6. This series of 18 patients, three of which with stage IB as our patient, and most with patchy-plaque alopecia, showed, in the majority of cases, a decreased number of pilosebaceous units, yellow dots, dystrophic hairs, vellus hair, dotted vessels, and spermatozoa-like vessels6. These findings translate follicular changes related to folliculotropic infiltration of atypical T-cells with disruption of the normal follicular cycle. Black dots and scale, which were readily identified in our patient, were less frequent findings6.
Gallo et al. also presented a subgroup analysis comparing findings in generalized alopecia and patchy-plaque alopecia, and in early stage and advanced FMF. Scale was more common in patchy alopecia (but statistical significance was not met)6; this was, indeed, a prominent finding in our patient. On the other hand, broken (dystrophic) hairs were more common in advanced FMF, but not exclusive to this subgroup6. Accordingly, we found dystrophic hairs in our patient, which probably relates to the fact that FMF (and MF in a broader sense) is an asymmetrical pathophysiological processes that manifest, in the same patient, with lesions in different stages of its natural story.
The coexistence of several different (and often unspecific) trichoscopic findings in FMF contributes to the difficulty of standardizing the examination of these patients. When considering isolated trichoscopic findings, differential diagnosis is extensive: yellow dots are present in alopecia areata and discoid lupus erythematosus; dystrophic hairs are commonly found in trichotillomania and tinea capitis; and white scaling can be found in different forms of eczema, dermatomyositis, and even pityriasis rubra pilaris. To consider FMF, one should take into account the constellation of supporting findings in trichoscopy and correlate them with clinical and histopathological aspects. Regarding the later, trichoscopy can also be useful by guiding biopsy site selection, as perifollicular accentuation reflects folliculotropism in histopathological examination7.
At this time, more data regarding the trichoscopic examination of FMF patients is needed; clinical algorithms based on larger series of patients and reports of findings in individual cases will contribute to help guide differential diagnosis and define the threshold to biopsy lesions, as early identification and treatment of these patients is of the utmost importance.















