Introduction
Snakebite is rare in Europe, but can lead to potentially fatal complications.1 The estimated incidence is 0.4-1.1 cases/year per 100,000 inhabitants, causing approximately four deaths per year.1 Vipers are the most common species involved in snakebite poisoning in Europe.2 In pediatric age, snakebite mainly affects male children, and the most common site of lesions are the upper limbs, as the bites often occur in the context of playing and exploring the environment.3 Accidents involving venomous animals are a global public health problem that has received the attention of the World Health Organization in recent years.4,5 The increase in international mobility and access of travelers to more remote areas also contribute to an increase in the number of patients presenting to the Emergency Department with these injuries.6
Case report
A 17-year-old Portuguese male adolescent with no relevant personal history was bitten by a Vipera aspis on the left index finger while camping in Switzerland. He was admitted to the Emergency Department because of inflammatory signs on the left hand (second and third fingers) and forearm associated with severe pain. He was started on intravenous therapy with amoxicillin and clavulanic acid, hydrocortisone, and clemastine. Anti-ophidian serum was not administered. On the third day of therapy, the inflammatory signs worsened (mainly swelling) and extended to the entire left upper limb. Nevertheless, on the fifth day of hospitalization, the boy was discharged under oral amoxicillin and clavulanic acid for five days with the indication to complete 10 days of antibiotic therapy. He then returned to Portugal and was readmitted to the hospital the same day for uncontrolled pain. He presented with swelling, erythema, and necrosis of the left index finger and swelling and violaceous erythema of the left third finger (Figure 1). In addition, there were exuberant signs of inflammation over the proximal forearm, elbow, and arm (Figures 2 and 3). After evaluation by Pediatric Surgery, intravenous amoxicillin and clavulanic acid were restarted. The possibility of compartment syndrome was evaluated and ruled out. Due to clinical improvement, he was discharged on the fourth day of hospitalization (nine days after the bite) on oral amoxicillin and clavulanic acid for six days. On post-discharge assessment, the lesions showed good evolution and favorable epithelialization.
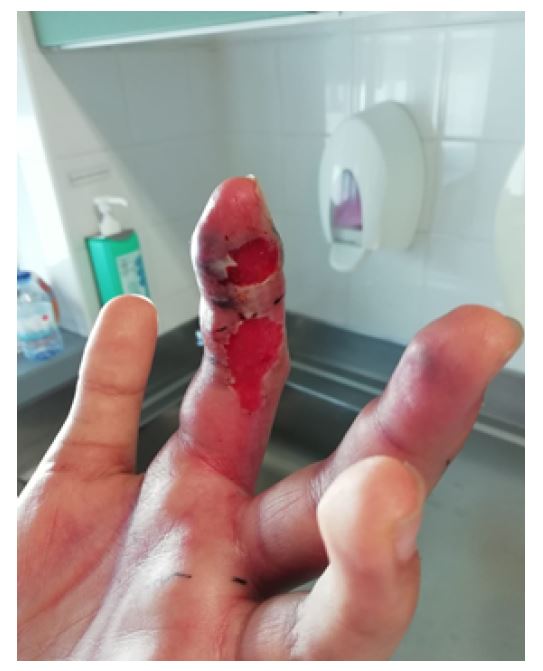
Figure 1 Left index finger with signs of swelling, erythema and necrosis and left third finger with swelling and violaceous erythema.

Figure 2 Inflammatory signs of the proximal forearm and axilla with swelling and violaceous erythema.
Discussion/conclusions
Although Europe has a high number of vipers, few cases are reported due to its favorable habitat.1 Reporting of viper bites is not mandatory in most countries, so the global incidence is underestimated.1 In Europe, only France and Sweden routinely record snakebites, and in 2017, the World Health Organization oficially listed snakebite poisoning as a priority neglected tropical disease.4,7 In Portugal, there are three species of venomous snakes - Vipera latastei, Vipera berus seoanei, and Malpolon monspessulanus.8 Of these, the first two have the most active venom due to their hemotoxic and cytotoxic properties.6 They are distributed all over the country, mainly in the mountainous areas (Gerês, Monchique, Sintra, Guadiana Valley, and Mafra).8 Children are more likely to be exposed to the potentially fatal consequences of snakebites, especially due to their lower weight-to-venom ratio.8,9
Studies have reported some risk factors for progression to severe envenomation, such as female sex, bites to the upper extremities, and extreme pain in the first minutes after the bite.10 Regarding clinical manifestations, these can be local and/or systemic.6 Initially, there are some manifestations due to sympathetic nervous system activation related to the stress of the event, which may include nausea, tachycardia, vasoconstriction, and sweating, and must be distinguished from systemic manifestations resulting directly from the envenomation.6,8 Local manifestations include frequent identification of erythematous patches approximately 1 cm apart (fang marks), pain, erythema, heat, edema, ecchymosis, lymphangitis, blistering, and occasionally cutaneous and/or muscular necrosis.6,8 In the absence of local inflammatory signs in the first 30 minutes after the bite, it is very unlikely that venom has been inoculated (dry bites).2,8 Systemic manifestations usually occur a few hours after the bite and may include gastrointestinal symptoms (vomiting, diarrhea, abdominal pain), headache, or dizziness.6 More severe manifestations include hypotension, tachycardia, dyspnea, and syncope.8 Most complications result from the hemotoxic effects of the venom, which can cause gastrointestinal, genitourinary, and central nervous system hemorrhage.8 In more severe cases, multiple organ failure, cardiogenic shock, pulmonary edema, and disseminated intravascular coagulation may occur.10 All patients admitted for snakebite should be closely monitored for the first 24 hours because of the potential for rapid venom spread and deterioration of the patient's condition.5,11 The severity scale developed by Boels et al. (Table 1) determines the administration of anti-ophidian serum for grade 2 or 3 lesions.12 Treatment should be initiated within the first 72 hours, and its effectiveness is maximized if administered within the first 10 hours after the bite.8,12
Table 1 Clinical grading of viper envenomation, adapted from Boels et al. (2012).12
| Grade | Envenomation | Clinical manifestations |
| 0 | “Dry bite” | Fang marks, no local signs |
| 1 | Minor | Local swelling, pain, erythema No general symptoms |
| 2 | Moderate | Regional pain, edema, and/or hematoma (in most of the bitten limb) Moderate general symptoms (mild hypotension, nausea, vomiting, abdominal pain) |
| 3 | Severe | Extensive edema involving the trunk and/or severe general symptoms (severe hypotension, shock, severe coagulopathy, anaphylaxis) |
The patient in this case had a grade 2 lesion, but no serum was administered at the hospital where he was initially admitted. A possible explanation for this is that the inflammatory signs did not worsen until the third day of hospitalization. In Portugal, the antivenom available is Viperfav®, which contains purified F(ab’)2 fragments of equine antibodies that neutralize the venom inoculated by the viper.8,12 The dose to be administered is 4 mL diluted in 100 mL of 0.9% NaCl, initially at 50 mL/h, and if there is no immediate reaction, the remainder is infused over one hour.7,8 Although intramuscular administration is possible, the intravenous route is preferred because it allows for greater antivenom bioavailability.7 There is no need to adjust for weight, as the snake injects the same amount of venom in both adults and children.7
The administration of a second dose of anti-ophidian serum is controversial. Some authors recommend the administration of a second dose after five hours if systemic symptoms are not controlled, while others have shown no benefit in terms of shortening hospital stay and improving functional impairment and hematoma.8,9,12 In all cases of snakebite envenomation, it is always advisable to contact the antivenom center for proper advice, including how to obtain antivenom serum if it is not available at the health facility where the patient is located. Antivenom serum is safe and improves the prognosis of viper envenomation.12 The major adverse effect of anti-ophidian serum is anaphylaxis, which occurs more frequently in the first three hours after infusion.6 If an anaphylactic reaction occurs during infusion, it must be stopped and intramuscular adrenaline must be administered immediately.6 After recovery from an anaphylactic reaction, the clinical indication for anti-ophidian serum should be reevaluated. If the indication remains, intravenous administration should be resumed slowly until the full dose is administered.6 Intravenous hydrocortisone can be administered, but its onset of action is slow and does not prevent the risk of recurrence.6 There are no absolute contraindications to the administration of anti-ophidian serum.6,7 Patients with a previous allergic reaction to anti-ophidian serum or a personal history of severe atopic disease are at high risk for severe reactions and the need for anti-ophidian serum should be weighed.6 Another adverse reaction is the occurrence of fever during the infusion, which should be treated with antipyretics.6 Antibiotic prophylaxis is not routinely recommended. In the presence of cellulitis or abscess, antimicrobial treatment should be initiated, taking into account the coverage of the commensal flora of the snake oral cavity and human skin.6 The most indicated options are amoxicillin and clavulanic acid, a third-generation cephalosporin, and metronidazole or piperacillin/tazobactam.6 Fifty-seven percent of pediatric patients may deteriorate in the first few hours after the bite, and even after an initial serum response, systemic symptoms may recur within 24 to 48 hours (due to absorption of venom from the bite site after perfusion has improved and shock/hypovolemia has been corrected), requiring hospitalization for grade I or II lesions and Intensive Care Unit admission for grade III lesions.6,8 Monitoring during hospitalization includes continuous assessment of vital signs, electrocardiographic monitoring, urine output, and surveillance for systemic complications.8 Analytical assessment should be performed every eight to 12 hours (six hours in the case of coagulopathy).8 If anti-ophidian serum is administered, at least 24 hours of observation is mandatory, and discharge depends on the clinical evolution and complications.8 Although rare, snakebites in pediatric age can result in medical and surgical emergencies.1 It is therefore essential that health professionals are aware of these cases and are able to recognize and treat these patients quickly. In some Portuguese centers, there are protocols for the management and treatment of snakebite poisoning. However, it would be important to have a more effective reporting system. A national database would improve the care of snakebite victims. In addition, it is essential to invest in more effective, safe, and easily accessible antivenoms, which are often only available in tertiary hospitals, far from the rural areas where most of these accidents occur.
Key points:
Snakebite is a neglected public health problem in Europe, and children are more severely affected due to their small body mass.
Anti-ophidian serum is a safe and effective therapy and should be administered to patients with grade 2 or 3 lesions.
An effective reporting system and national database would be important to improve knowledge and care of snakebite victims.
















