Introduction
Preeclampsia is a pregnancy disorder that typically occurs after 20 weeks’ gestation and is associated with new-onset hypertension, often with new-onset proteinuria.1 In the absence of proteinuria, the diagnosis of preeclampsia should be established when hypertension is accompanied by new-onset thrombocytopenia, renal failure, impaired liver function, pulmonary edema, medication-unresponsive frontal headache, or visual symptoms.2 Eclampsia is the convulsive manifestation of hypertensive disorders of pregnancy and is defined by new-onset tonic-clonic, focal, or multifocal seizures or even coma in the absence of other causative conditions.2 The prevalence of eclampsia is estimated to be 5-7 per 10,000 deliveries in developed countries and is an important cause of perinatal morbimortality, particularly in developing countries, where its incidence may be higher.3,4
Posterior reversible encephalopathy syndrome (PRES) is characterized by a variety of neurological signs and symptoms (including headache, seizures, visual disturbances, and other focal neurological deficits) and distinctive neuroimaging findings reflecting subcortical vasogenic edema, particularly in the posterior regions, which are typically reversible (clinically and radiologically) within days to weeks.5,6 Although the pathophysiological changes underlying PRES are not fully understood, endothelial dysfunction is a key factor, caused by a rapid increase in arterial blood pressure leading to an hypertensive emergency or by circulating toxins that directly induce endothelial dysfunction, as seen in patients presenting with PRES in the context of preeclampsia, sepsis, or treatment with cytotoxic or immunosuppressive agents.5,7 These lead to breakdown of the blood-brain barrier and subsequent brain edema.5
The frequency of PRES associated with eclampsia is unknown, with some studies suggesting that PRES should be considered a core component of the pathogenesis of eclampsia.8 Herein, two clinical cases of PRES in the setting of eclampsia are presented.
Case reports
Case 1
A 26-year-old pregnant woman with a history of previous eutocic delivery was admitted for labor induction at 41 weeks’ gestation. The patient had adequate monitoring for a low-risk pregnancy except for suspected fetal macrosomia. A cesarean section was performed for dynamic dystocia. On postpartum day 2, the puerperal woman complained of persistent frontal headache associated with high blood pressure (maximum values of 170 mmHg systolic and 100 mmHg diastolic). In addition, she developed resting dyspnea and desaturation within a few hours, and pulmonary auscultation revealed evidence of pulmonary stasis.
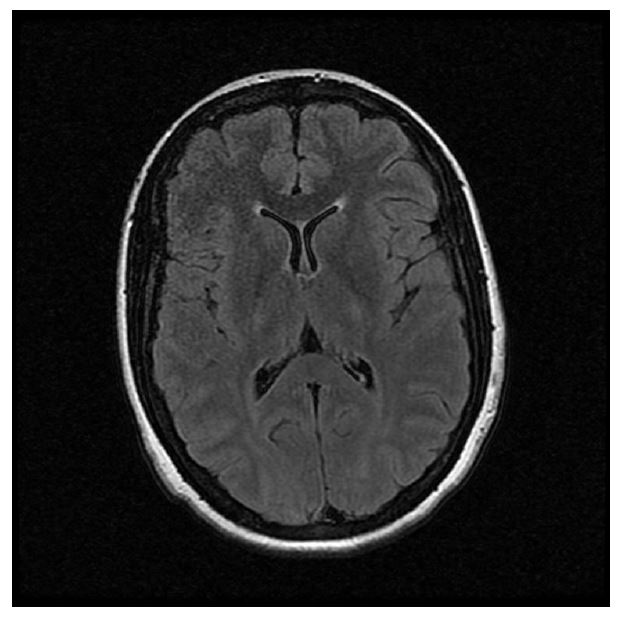
Approximately seven hours after the onset of these symptoms, the patient complained of amaurosis and presented with two generalized tonic-clonic seizures. At the postictal phase, the patient was confused and agitated with persistent amaurosis. Chest computed tomography (CT) scan showed evidence of pulmonary edema. Blood samples showed elevated aspartate transaminase (twice the normal range), hyperuricemia (8.4 mg/dL), and significant proteinuria (protein/creatinine ratio of 1.2), supporting the hypothesis of an eclamptic event. Bilateral areas of hypersignal in cortico-subcortical topography were observed in the parieto-occipital transition on brain magnetic resonance imaging (MRI; T2 FLAIR; Figure 1).
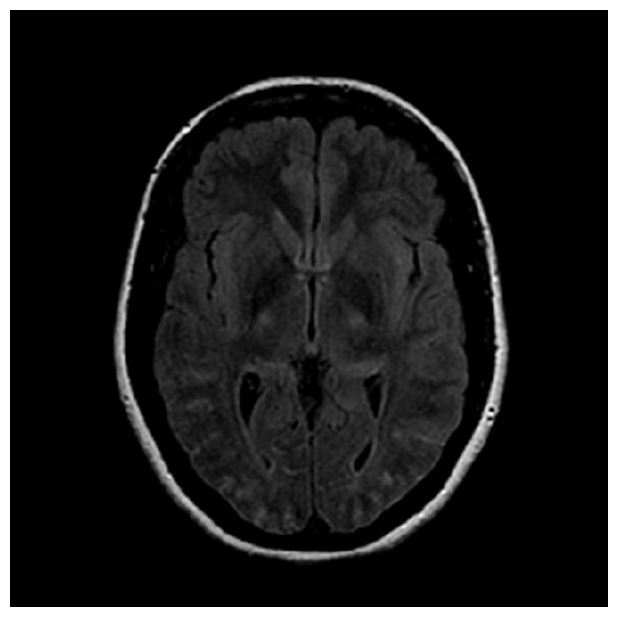
Figure 1 Case 1: Brain MRI (T2 FLAIR) showing bilateral areas of hypersignal in cortico-subcortical topography at the parieto-occipital junction.
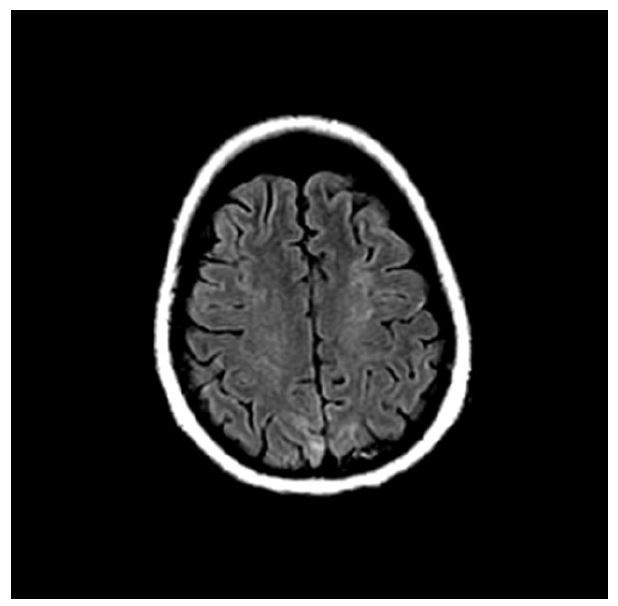
After a few days, these findings were no longer present at the control examination (Figure 2). No abnormal contrast uptake or enhancement was observed after contrast administration. This type of presentation is typical of PRES and also shows its reversible nature.
The next day, the amaurosis had resolved and the fundoscopic examination was normal. The patient completed a magnesium sulphate protocol and remained hypertensive in the following days, requiring the administration of labetalol for blood pressure control and nimodipine to reduce brain edema. She was discharged nine days after delivery on lisinopril 5 mg/day for blood pressure control. Approximately three months after the event, she presented with normal blood pressure without medication.
Case 2
A 34-year-old pregnant woman with a history of previous cesarean section, iatrogenic hypothyroidism after total thyroidectomy, and gestational diabetes was admitted for labor induction at 40 weeks’ gestation. High blood pressure was noted at the time of epidural catheter placement, and borderline blood pressure values were observed throughout labor induction. Cesarean section was elected after unsuccessful instrumentation.
On admission to the operating room, the patient presented with tonic-clonic seizure and tongue biting. Emergency cesarean section was performed immediately and the baby was born with Apgar score >7 at 5 minutes. Magnesium sulphate protocol was initiated as well as bicarbonate perfusion for metabolic acidosis. Blood samples showed only mild elevation of liver enzymes.
A few hours after the event, the patient presented with a normal level of consciousness without any signs of neurological deficit, headache, or visual disturbance. Brain MRI (T2 FLAIR) performed two days later showed hypersignal areas in the brainstem region with bilateral, predominantly right, pontine hypersignal (Figure 3), as well as left frontal and bilateral cortical-subcortical parietal enhancement (Figure 4), representing a much rarer form of imaging presentation of PRES. No abnormal contrast uptake or enhancement areas were observed after contrast administration, further supporting the diagnosis of PRES. Blood pressure control was achieved five days postpartum with nifedipine 30 mg/day, and the patient was discharged from the hospital eight days after delivery.
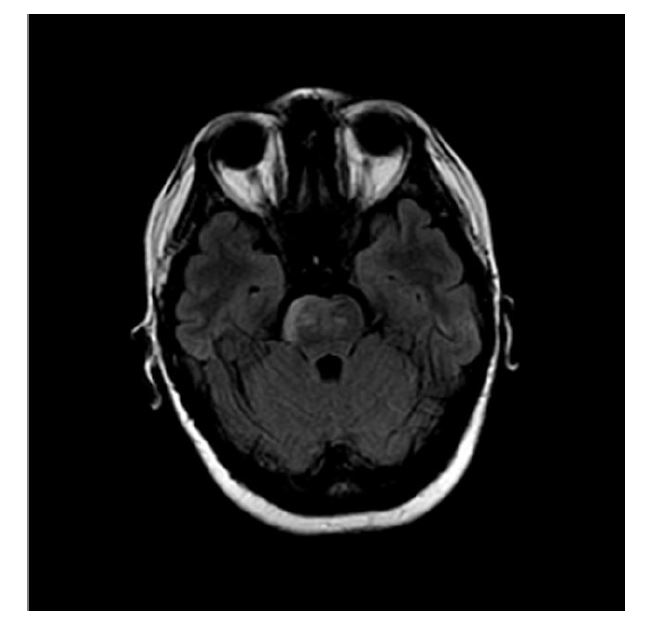
Figure 3 Case 2: Brain MRI (T2 FLAIR) showing hypersignal areas in the brainstem region with bilateral, predominantly right-sided, pontine hypersignal.
Discussion
The clinical presentation of PRES in the context of eclampsia is heterogeneous.9 According to Fugate, PRES is characterized by a variety of neurological symptoms, usually associated with elevated arterial blood pressure. Onset may be acute or subacute, with symptoms developing within hours to several days or even weeks. As most of the literature on the syndrome consists of retrospective observational studies, the frequency of symptoms varies depending on the sample size and population.5 In a 2013 retrospective study of 47 patients, Brewer et al. also reported headache and visual impairment as common symptoms of eclampsia and PRES, occurring in 87% and 51% of patients, respectively.8 In 2015, Kurdoglu et al. described headache associated with visual impairment as the main symptom of PRES (60.0%) in women with eclampsia and this syndrome.10
Many studies have contributed to the hypothesis that PRES is the primary central nervous system injury in patients with eclampsia.8 This statement was supported by the results of a Mayo Clinic study, in which all patients with eclampsia who underwent imaging assessment had clinical and radiologic findings of PRES. Brewer et al. also stated that MRI and/or CT scan indicated the presence of PRES in all patients with eclampsia included in their 2013 study.8 More recently, in 2019, Sardesai et al. conducted the largest study of neuroimaging in eclampsia to date, and their results showed that PRES was the major component in 100% of patients with eclampsia on MRI/CT. However, they stated that neuroimaging should not be routinely used in patients with eclampsia because the diagnosis based on symptoms (such as headache, visual disturbances, hypertension, and convulsions) was quite sensitive.11
The cases presented show two very different presentations of eclampsia associated with PRES. In Case 1, the patient developed typical headache and visual disturbance symptoms before and after the seizure episode, whereas in Case 2, none were present. In Case 2, clinical suspicion was raised and neuroimaging helped to establish the diagnosis. Additionally, none of the MRIs showed areas of abnormal hyperenhancement of gadolinium, which favored the diagnosis.