Introduction
It is estimated that diabetes affects around 537 million people of adult age worldwide and is responsible for 11.5% of health expenditure.1 In Portugal, the prevalence of diabetes has followed the global trend, gradually increasing year on year, and in 2021 it was 14.1%.1
Despite the emergence of new classes of drugs, metabolic control targets are still laborious to achieve and often fall short of therapeutic goals. The chronic and acute complications of diabetes are still a reality and account for a significant share of both resource consumption and overall health expenditure. In 2021, national expenditure on hospitalizations by homogeneous diagnosis groups (DRGs) for diabetes was approximately 310 million euros.1
When analysing the investment made in new technologies (such as continuous glucose monitoring (CGM) systems and continuous subcutaneous insulin infusion (CSIP) systems), this amounted to 80 million euros.1 The discussion around the sustainability of health systems is pressing, but it is appropriate to ask the following question: is not it advantageous to invest more in technology if this results in a reduction in the cost of complications and an improvement in the quality of life for the population with diabetes?
More than 100 years after the discovery of insulin, there are still several barriers that prevent us from achieving adequate glucose control: individual factors, others related to health professionals and limitations attributed to health systems. Some socio-economic aspects can potentially add difficulty to addressing the disease, but these are not the only ones that should be considered. Socio-cultural, psychological and behavioural characteristics can also add limitations to clinical success. Diabetes is a chronic disease that requires persistence, resilience, dedication, discipline and method from those who live with it on a daily basis. Technology has been effective in overcoming some of these obstacles, improving adherence to drugs and lifestyle changes and supporting therapy management.
Concepts: Telehealth, Telemedicine and Digital Health.
The expansion of the technological world has also brought a new lexicon to medicine and new concepts have become part of scientific texts and organizational discussions. Due to the similarities in nomenclature, some definitions can be easily misunderstood and therefore deserve their own space for clarification.
Telehealth is a broad term that includes the widespread use of electronic information and communication technology to provide remote healthcare, training for other professionals and the community, carrying out public health studies as well as some logistical and administrative management procedures.2
Many other concepts are also included in the definition of telehealth. This is the case with telemedicine, which refers to clinical activity carried out at a distance, specifically by health professionals, who use information technology and telecommunications for this purpose. Some practical examples are teleconsultations, remote image evaluation, screening, rehabilitation programs, etc.2
Digital health or mobile health (mHealth) has been defined by the World Health Organization as a medical and public health practice supported by mobile devices, such as cell phones, continuous monitoring devices, digital assistants and other wireless wearable devices. These procedures are now very common in diabetes consultations.3
Digital Health and Diabetes
To date, out of half a million mobile health applications, those designed as additional tools to improve diabetes con-trol are among the most common. Their enormous potential is recognized, given that more than 2.5 billion people use smartphones.4
These apps can be divided into different types according to their characteristics.
Nutrition mobile apps contain tables with the composition of foods in terms of carbohydrates, proteins, fats and energy value. Some help with meal planning and insulin calculation.5
Glucose monitoring applications record and display graphs of glucose trends that allow the individual and the healthcare professional to manage diabetes control in addition to glycosylated haemoglobin (HbA1c).5With the advent of these technologies, other parameters have been taken into account and included in good clinical practice. Time in range (TIR) is the time spent with blood glucose values at the therapeutic target (between 70 and 180 mg/dL) and it has been determined that for most people it should be greater than 70%. The time below range (TBR) is the time spent in hypoglycaemia and should be less than 4%. The coefficient of variation of glucose measures the variability of glucose in a given individual and is considered to be equal to or less than 36%. Finally, through continuous monitoring it is possible to determine the glucose management indicator (GMI). The GMI uses the same scale as HbA1c (% or mmol/mol) but it is calculated exclusively from CGM data; it is based on average interstitial glucose data and it varies depending on the analysis period selected by the user.6 There are several factors that justify the differences found between GMI and HbA1c (±0.1% in 81% and ±0.3% in 51% of cases) and should be taken into account when analysing both parameters: the time of use/percentage of data captured by the sensor, the period of time being analysed, other concomitant pathologies such as anaemia or hemoglobinopathies, which can affect the haemoglobin glycation mechanism.7 Furthermore, these tools also represent safety models by incorporating alarm systems that warn the user in the event of hypoglycaemia or hyperglycaemia, thus avoiding extreme situations of acute diabetes complications. For the majority of people who use them, alarms also help to improve the quality of glycaemic control, increase time on target and reduce glucose variability.8
Insulin titration apps usually include insulin bolus calculators to help you decide how much insulin to administer at each meal or at times when you need to correct your glucose level. For this calculation to be carried out automatically, the healthcare team has to enter some information into the application: the insulin: carbohydrate ratio (i.e., the amount of carbohydrate in mg or portions metabolized by 1 unit of insulin) and the insulin sensitivity factor (ISF), which represents the amount of glucose in milligrams per deciliter corrected by 1 unit of insulin. Some of these applications are connected to PSCI systems and/or "smart" insulin pens, recording the insulin applied as well as interpreting this data.6
"Smart" insulin pens have also made an important contribution to both diabetes management and the quality of life of those living with the disease. A "smart" pen is an insulin delivery system that allows data to be transmitted from the insulin pen to compatible platforms used by healthcare professionals and people with diabetes. However, it also has other advantages: it allows users to confirm whether insulin has been administered, how many units of insulin have been applied and to count the time since it was administered. Trials have shown that its use reduces the number of unadministered boluses and late boluses.9 These pens connect via Bluetooth or nearfield communication (NFC) to CGM applications, allowing insulin to be correlated with the results obtained. To date, they do not incorporate bolus calculation systems, so it is necessary to calculate them individually or use other resources.10
Physical activity apps allow users to monitor their physical activity, count the calories they burn and set goals for exercise and weight control.11
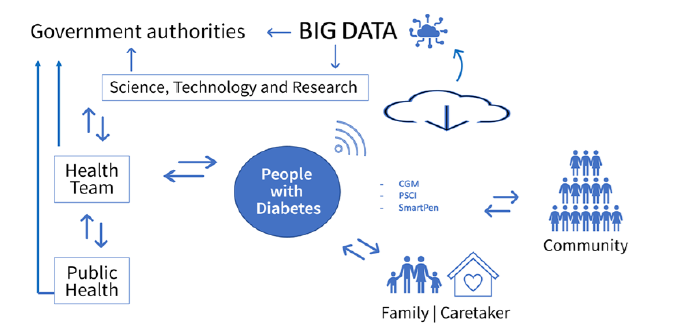
The advancement of digital technology and artificial intelligence in health and research has enabled significant progress in knowledge about diabetes and the people who live with this condition. As we have seen, its implementation is wide-ranging, from the individual use of electronic devices and mobile applications that help with decision-making and disease management, remote communication with the health team, family members or caregivers, data collection and interpretation, the existence of prevention programs, the design of early diagnosis algorithms and the creation of a networked ecosystem that allows professionals from different areas of work and/or different regions to connect.
As such, its practical application can be divided into two main areas - the primary use around an individual's health and the secondary use of data by government health authorities. The data generated by the devices used in diabetes, such as CGM, state-of-the-art glucometers, PSCI systems, "smart" insulin pens and others, allow for the creation of extensive electronic health records that can be processed through digital means, making it possible to draw conclusions with applicability at various levels. This data can be used to personalize the care provided to people and can also be aggregated at a population level and associated with other data that has an influence on health, such as education, employment and environmental data.12
In a recent systematic review of the literature, it became clear that big data analysis had moderate to high accuracy for diagnosing diabetes and its complications.13
However, despite the growing awareness of the benefits of big data in health and the methodological and technological advances, there has been caution in adopting approaches based on this data and artificial intelligence, related to aspects such as patient privacy and safety. The lack of political and financial support for these initiatives is also one of the limitations identified.14
In relation to the specific needs of people with diabetes in terms of interaction with technology, the promotion of digital health literacy (the ability to obtain and use electronic and digital tools applied to healthcare) is a determining factor in promoting adoption and long-term involvement. These strategies will only effectively contribute to changing the panorama of inadequate diabetes control, incidence of complications and subsequent loss of quality of life, if they manage to support empowerment and motivation to change lifestyles and self-care and self-monitoring practices.15 In this process, especially when mediated by digital tools, it has been shown that professionals can play a decisive role.16
The support provided by trained health professionals should cover digital health literacy skills and the wider user experience, taking into account the user's individuality, needs and motives for using the technology.
In order to promote a supportive environment for diabetes management that encourages participation, users need to get involved and take action, thereby creating environments that are conducive to their use.17
Real-life Examples
Taking the integrated diabetes care unit of the APDP (Portuguese Diabetic Protection Association) as an example, there was an obvious need to reorganize the provision of care in response to the COVID-19 pandemic, and our institution was able to maintain the number of scheduled appointments through a considerable effort in telemedicine and proactive contact. In fact, this initiative was singled out by the World Health Organization as good practice during the pandemic.18 A course was also developed for health professionals on new technologies applied to diabetes.
In terms of interoperability and participation in the national digital health ecosystem, APDP recently became the first external organization to join the National Health Service's Electronic Health Record. At an international level, APDP participates in benchmarking activities with international clinical registry networks, such as SWEET for paediatric diabetes and ENDO-ERN for rare forms of diabetes.
At the same time, APDP was part of a European consortium, which aimed to develop a digital solution in co-creation with people with diabetes and analyse the impact of its use on metabolic and weight control. The project involved 200 people with type 2 diabetes and 50 health professionals who accompanied them. A user-centred digital diabetes self-management solution with an integrated glucometer, scale and sphygmomanometer system was provided. The digital solution provided access to information, sent motivational messages and enabled interaction with professionals. Both groups of participants showed good adherence to the digital solution. Regarding the results, there was weight loss (median between 1.4 and 3.5 kg) and a reduction in HbA1c in 70% of people (on average 1%), both of which were statistically significant. The professionals stated that the digital solution facilitated communication and shared decision-making.19
In an attempt to investigate the impact of continuous monitoring on people with type 2 diabetes, a longitudinal study was also carried out, which followed a cohort of 102 people with type 2 diabetes using CGM for 12 months. It was found that the use of continuous glucose monitoring, albeit sporadically but in a structured way, contributed to improving metabolic control and the relationship between professionals and people with diabetes. The discussion of the values obtained and the different aspects of the treatment, the visualization and understanding of the data helped to increase satisfaction with the treatment.20
Bearing in mind that the person with diabetes plays a fundamental role in the entire therapeutic process, it is essential to find out about the impact of technology on their lives. Also recognizing that health professionals are crucial to therapeutic success, the APDP held focus groups to give a voice to those who experience first-hand the challenges presented by the use of technology.
The different groups highlighted the need to simplify its use, as well as recognizing its importance for management and monitoring (data in the process of being published).
At the same time, and in line with this notion of participatory processes and empowerment for self-management, in response to a challenge from the DGS's National Diabetes Plan, the APDP designed an interactive digital platform capable of demonstrating effectiveness in empowering people with diabetes and their informal caregivers to take care of their health, namely proper nutrition, physical activity, adherence to pharmacological therapy, monitoring and control of the disease, also including digital health literacy.17
The Future - Artificial Intelligence in Diabetes
Artificial intelligence (AI) integrates computer systems that enable tasks to be carried out which normally require human intelligence, such as understanding and interpreting language, making decisions or learning, using data sets and algorithms. Today, there are many situations in which we already use conversational interfaces to communicate with other devices using natural language instead of the usual interfaces such as key-boards or switches. This happens through chatbots, voice assistants or messaging apps.
Transferring this concept to its clinical application, the use of AI in the diagnosis and treatment of diabetes can currently be categorized into four fundamental areas: risk stratification, diabetic retinopathy screening, treatment support and disease self-management.
Some studies have compared the predictive performance of statistical models and artificial intelligence models. However, at present it cannot be concluded that the latter outper-forms conventional statistical analysis in predicting diabetes diagnosis. Some of these studies have been able to demonstrate high prediction in trained teams, but their accuracy drops significantly when applied to the real world. Despite these limitations, more efficient models are being developed that aim to incorporate data from omics databases (proteomics, genomics, metagenomics and metabolomics) into existing nformation in order to increase the ability to predict diabetes diagnosis before it occurs.21
In 2018, the U.S. Food and Drug Administration and later, in 2023, the European Union, approved the use of the IDx-DR device produced by Digital Diagnostics Inc. for retinopathy screening, which uses AI technology to analyse retinography images and automatically detect the presence of retinal and macular change.22
As far as support for diabetes treatment is concerned, the first intelligent therapeutic decision support system was approved in the United States in 2018: Dreamed Advisor Pro is a software designed to integrate data from PSCI and CGM pumps, providing remote information to healthcare professionals on the recommended insulin adjustment. The results of the ADVICE4U study showed that time on target and hypoglycaemia in patients treated using AI were not lower compared to the control group treated using manual insulin titration by healthcare professionals.23
With regard to the last point, which concerns the use of AI to support disease self-management, the system analyses biometric data and the continuous evolution of glucose in a given individual, while simultaneously generating alerts and making recommendations on measures to be taken to correct the trend or glucose value.
These functions, which have traditionally been carried out by healthcare teams, could be complemented on a daily basis by AI technology, providing continuous and uninterrupted support in diabetes self-management. However, AI applied to biosensors and continuous glucose monitoring makes it possible to go further. Individual data from CGM, the PSCI system, food intake and physical activity records are collected and grouped together in a system and processed by calibration and control algorithms, which in turn lead to machine learning that will generate decision lines and automatically modify insulin administration. This data processing and the resulting decisions are applied in glucose prediction systems, mobile applications, closed-loop systems or artificial pancreas. These automation systems allow people with diabetes to live safer, with fewer complications and a better quality of life. Healthcare professionals will have to adopt a supervisory position, which can be carried out remotely, which could contribute to reducing the pressure on healthcare systems.24
Conclusion
Rapid global technological evolution is capable of transforming the reality we know. We are getting closer and closer to smart health cities. The intersection of the various areas of science with the multiple fields of engineering is leading us to a new world of medicine. Due to its epidemiological and individual characteristics, diabetes is one of the chronic diseases that arouses the greatest interest from the point of view of scientific and technological research.
Currently, the ecosystem already allows for remote communication, training, education and information sharing between different teams, people with diabetes and/or health professionals. Therapy, combined with smart devices and greater autonomy, could enable better decisions to be made on an individual basis, contributing to better glucose control, fewer complications, a better quality of life, less expenditure on the disease and a better overall level of health for society. Some examples of good clinical practice were cited which have shown positive results and deserve to be replicated in other centres. It is important to invest in the digital literacy of the community and health professionals, in order to maintain equal access across the board for the entire population.
The data generated by the devices used by people with diabetes and by professionals will make it possible to create extensive databases that will provide access to information on the characteristics of the disease and the population, work on diabetes prediction algorithms, identify therapies for early reversal and adopt public health measures with a social impact.
We are living in the era of the digital revolution and artificial intelligence, which will surely go down in history as one of the transformative moments in diabetes, health and human life.