Introduction
In recent years, several studies focusing on improving self-care in long term conditions after an acute event, as a stroke or trauma from fall (Greaves & Campbell, 2007; Meleis, 2010) have shown that the potential for regaining the ability to self-care should not be limited to the bodily processes.
The person's motivation, attitude towards dependence, self-determination, and perception of self-efficacy are examples of conditioning factors that also play a decisive role in achieving autonomy gains (Lourenço, 2015; Riegel et al., 2019).
The concept of autonomy is often associated with independence; however, they have different meanings. Independence refers to the ability to perform daily life and self-care activities, while autonomy means the individual's ability to take care of oneself (Moilanen et al., 2021). While independence is associated with physical processes, autonomy is more related to mental dispositions (Ferreira et al., 2012). Dependence is viewed as a change, manifesting itself when a person is unable to meet his/her self-care needs due to lack or loss of physical, psychological or intellectual autonomy. The World Health Organization defines self-care as “the ability of individuals, families, and communities to promote health, prevent disease, maintain health, and to cope with illness and disability with or without the support of a healthcare provider” (WHO, 2009). The terms self-care and self-management are sometimes used interchangeably, however, self-management is understood as a component of the broader self-care continuum (Greaney & Flaherty, 2020).
Confining the question of a person's recovery potential to the level of bodily processes does not allow to explain why people with the same type and intensity of neuromuscular disorders have different levels of recovering over time (Hubbard et al., 2017). Emotional and attitudinal impairment is a strong predictor of the person's answer face the self-care recovery process (Lourenço, 2015). The psychological processes, such as awareness, self-esteem, self-efficacy, anguish, and hopelessness, are key factors in the recovery process of the person with limitations to self-care activities (Riegel et al., 2019).
Recognising the effect of changes is a core process in reconstructing autonomy in self-care (Lourenço, 2015). This process begins only after the person becomes aware of the changes that have occurred, which is frequently triggered when the person realizes that he/she is not able to perform a specific self-care task (Meleis et al., 2000). An attitude is associated with an intention to perform an action, being understood as an indicator of a behaviour (Ajzen, 2020). Attitudes are a multidimensional construct that combines the emotional component (e.g., beliefs, feelings), cognitive (e.g., the knowledge and the beliefs about something), and the behavioral (e.g. tendency to act according to the attitude) (Ajzen, 2020). If a person adopts a passive attitude (they do not take action but let clinical staff make decisions for them), his/her involvement will most likely be limited. The subsequent lack of commitment will eventually lead to the person’s withdrawal, with the nurse replacing this person in carrying out basic daily life activities. A responsible person shows a positive orientation towards the future, more initiative, more confidence, and is easily involved in the reconstruction of self-autonomy (Parente et al., 2021). Attitudes and intentions do not determine health behavior by itself but are generally indicators of how a person tends to act when experiencing a particular event (Ajzen, 2020). The degree to which people have control over behaviour depends on their ability to overcome barriers and the presence of facilitating factors such as experience, self-control and assistance provided by others (Ajzen, 2020).
The nurses play a pivotal role in a person's involvement in performing self-care. Therefore, this professional needs to understand the person’s actions and reasons to act and the meaning that he/she attributes to each achievement (Backman & Hentinen, 1999). It is crucial to understand the person's expectations and fears and encourage the rehabilitation process by enhancing the efforts while transmitting confidence and providing gradual assistance (Pryor, 2009). Several authors point out the potential of reconstruction of autonomy in self-care activities and the factors influencing it (Riegel et al., 2019). However, to date, no structured instrument has been developed to assess, in a multidimensional approach, this important topic in clinical practice. The purpose of the present study was to develop an instrument that allows the assessment of attitudes and emotional factors with the greatest impact on recovery, of a person dependent on basic self-care activities, the Attitudes Assessment Scale towards the Recovering Self-Care process after an acute event (AAS-RecSC), developed by a group of experts, and to analuse the psychometric properties. The AAS-RecSC is a wide-range instrument that assesses the emotional aspects and attitudes that significantly affect the recovering self-care process following an acute event.
1. Methods
A methodological study was performed in two phases. The first phase (Silva, 2019) involved the design of the instrument according to Hinkin´s et al (1997) and the selection of items. The second phase tested the scale and analysed its psychometric properties. Based on the theory of planned behaviour, a group of experts reached a consensus on the selection of 40 items that assess cognition, behavioral dispositions, emotion, willingness to learn, previous experiences, and meanings.
Sample: Twenty researchers in the field of self-care and advanced nurses of recognised merit, working in hospitals and long-term care units, were the group of experts. These experts were specialized in identifying attitudes and emotions that influence the recovery process of a person with an inability to self-care after an acute event. The Boateng et al. (2018) recommendations to consider an expert were followed. A convenience sample of 118 participants, recruited from two services of a general hospital, and two long-term care units in the North of Portugal, was selected for the second phase of the study. The hospital units and the long-term care units have the same clinical profile patients. The inclusion criteria were being given a nursing diagnosis for self-care deficit, 18 years older or over, having more than four years of schooling, being able to understand and answer the questionnaire, and accepting to participate freely and in an informed way. The exclusion criterion was all persons that presented a verbal behavioural response indicative of confusion or a marked and severe cognitive impairment. The clinical staff of the health units was responsible for assessing this criterion.
Material: Based on the Nursing Outcomes Classification (NOC) (Moorhead et al., 2013), a set of indicators (evaluated by a Likert-type scale ranging from 1- never or almost never to 5- almost always or always) were developed to assess the attitudes and emotions that influence the recovery process of a person with an inability to self-care. A total of 40 items related to cognition, behavioural dispositions, emotion, willingness to learn, previous experiences, and attributed meanings are selected. Coping, belief and volition are concepts ontologically related to attitudes in health (ICNP, 2017). The emotion was understood as a psychological process characterized by the presence of conscious or subconscious, pleasant or painful feelings likely to increase with stress or illness. Hope, confidence and negative emotion (anxiety, insecurity, sadness, despair, depressed mood, fear, helplessness, and loneliness) are within the emotion spectrum. Involvement is one of the intrinsic factors highlighted as enhancing self-care (Committee on the Learning Health Care System in America & Institute of Medicine, 2013; Webber et al., 2013). Attributed meanings, represents positive or negative emotions attributed to the person according to his/her situation or towards assistive devices that could be used to facilitate adaptation. Feeling useless or a burden are meanings reported when impairment in autonomy is observed. On the other hand, attributing a positive meaning to the condition of dependency means that the person is learning new ways of dealing with the situation (Kralik et al., 2010).
Self-care activities were assessed through the Self-Care Dependency Assessment (SCDA) (Parente et al., 2021). The SCDA domains are structured according to the ICNP® (version 1.0). The items of each domain were based on the NOC (Moorhead et al., 2013). The study of the metric characteristics revealed a high level of reliability (Parente et al., 2021). In the present study, the SCDA presented an alpha coefficient of Cronbach of 0.80. Higher values mean increased independence in the activities of daily living.
Ethical considerations: The study had the approval of the Ethics Committees of the involved institutions (2019.059.051-DEFI/052-CE). The gathering of information was carried out by the first two authors. The participants were informed of their right to withdraw from the study at any time.
Procedures and data collection: The participants were approached during hospitalization after being referred by the head nurse responsible for the inpatient service. Data collection was carried out by one experienced nurse from the ward, who was previously trained. The sample size followed the recommendations of Hair et al. (2018) and the aim was to reach a minimum of 5 to 10 participants per scale item. The Exploratory Factor Analysis (EFA) was used to define the structure of the data matrix and determine the number and nature of the latent variables (factors) that better represented the observed variables. The EFA analyses the inter-relationship structure of the observed variables and defines the factors that better explain its covariance (Hair et al., 2018). The Kaiser-Meyer-Olkin test (KMO) and Bartlett's test of sphericity were used to evaluate the data adjustment and the quality of the existing correlations between the variables to carry out the factorial analysis (Pestana, & Gagueiro 2014). Values of KMO greater than 0.7 and Bartlett's values <0.05 were used as a reference (Pestana & Gagueiro 2014). The confirmation of the number of factors considered the following criteria: (1) eigenvalues >1; (2) exclusion of factorial loads <0.45, (3) each factor should explain at least 5% of the variance; (4) implementation of Horn's parallel analysis criteria through the graphical analysis of the variance curve and discontinuity principles (Hair et al., 2018).
The reliability of the measures was evaluated through the Cronbach's alpha coefficient that provides a measure of the scale's internal consistency and is calculated from the average of the inter-correlations between all items of the scale; for a good internal consistency, the alpha value should be higher than 0.80, but values above 0.60 are accepted (Pestana, & Gagueiro 2014).
The Confirmatory Factorial Analysis (CFA) was carried out through the AMOS program (version 26) to test the re-specified AAS-RecSC theoretical model. The variance was set at 1 to analyse the significance of each factor’s items and scale the factors. The covariance matrix was inputted using the Maximum Likelihood Estimation Method. The existence of outliers was assessed and normality by the asymmetry coefficient and univariate and multivariate kurtosis. The quality of the model adjustment was measured according to the indexes and corresponding reference values (Kline, 2016). The local adjustment was evaluated by the Mahalanobis squared distance, factorial weights, and individual item reliability. The Comparative Fit Index (CFI), Root Mean Squared residual (RMR), Root Mean Square Error Approximation (RMSEA), its confidence intervals (CI) and modification indexes were also considered. The model adjustment included theoretical considerations.
2. Results
The 118 participants under study, mostly female (59.3%), were recovering from a dependency-generating event (e.g., stroke, falls, chronic illness relapses) over the last six months. Respondents had an average age of 73.52 (SD=±12.04). Before the episode leading to hospitalization, 11% were still professionally active, and 27.1% were married. The participants' schooling was on average 4.93 years (SD=3.72), ranging from 4 to 18 years of successful school attendance. Most people had suffered an episode of stroke (49,6%), fractures of the lower limbs due to falls at home (26,5%) and only a few participants had experienced decompensation of chronic diseases (6%). All the 118 participants had a temporary loss of autonomy with the identification of potential recovery possibilities. A lower score represents greater dependence for self-care (Table 1). Limitations of self-care activities require seeking help, especially for bathing, dressing and undressing, walking, with participants demonstrating less commitment in activities such as feeding, transferring and turning around.
Table 1 Self-Care Dependency Assessment
| Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|
| Transferring/turning and lifting oneself | 1 | 4 | 2.64 | .71 |
| Walking | 1 | 4 | 2.14 | .96 |
| Using the toilet | 1 | 4 | 2.31 | .77 |
| Feeding | 1 | 4 | 3.31 | .96 |
| Getting ready | 1 | 4 | 2.62 | .94 |
| Bathing | 1 | 4 | 2.14 | .41 |
| Dressing | 1 | 4 | 2.15 | .59 |
To understand the behaviour of each item, a univariate exploratory analysis was performed, and no outliers were identified. Through the EFA, the behaviour of the 40 items of the scale under study was explored to determine the factorial loads and the allocation of the items to the factors. The first analysis identified nine components. Most of the items in the behavioral dispositions and willingness to learn were combined into one component. Additionally, most of the items of the emotions and meanings were combined into another component. For this reason, a new analysis was performed forced the model into four components. The results showed a large overlap with the six-based concepts.
The KMO statistic, used as an adjustment measure of the model, was 0.88, and Bartlett's test of sphericity showed a significant value of 0.01, indicating the appropriateness of the factorial analysis technique. Six items obtained communalities inferior to 0.50 (items 11, 15, 20, 22, 27 and 40). Three items were excluded for presenting a factorial load below 0.45 (20, 22, and 40).
The forced four-factor solution for the AAS-RecSC is presented in table 2. The first component with 19 items related to behavioral dispositions and willingness to learn. The second component groups the items related to cognition. The third component groups the items related to emotions and the items related to meanings, and the fourth-dimension groups the items of previous experiences. Altogether, the four components explain 57.16% of the variance of the measure.
Table 2 Principal Component Analysis. Factorial loads of the component matrix rotated from the AAS-RecSC.
| Components | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| 1. Keeps his/her attention focused | .50 | |||
| 2. Identifies his/her current health condition | .78 | |||
| 3. Recognises the limitations to self-care arising from the current health condition | .81 | |||
| 4. Asks for help when needed | .73 | |||
| 5. Recognises the meaning of an idea that is conveyed to him/her | .69 | |||
| 6. Identifies and explains the differences between two objects | .76 | |||
| 7. Can choose between two or more alternatives | .81 | |||
| 8. Recalls recent events or experiences accurately | .65 | |||
| 9. Recalls past events and experiences accurately | .50 | |||
| 10. Views the dependency situation as a harm/loss* | .50 | |||
| 11. Considers having the necessary resources available to face the challenge posed by the dependency situation | .58 | |||
| 12. Manifests a sensation of control and psychological comfort | .56 | |||
| 13. Shows positive response to external stimuli | .62 | |||
| 14. Believes that the recovery is mainly dependent on himself/herself | .57 | |||
| 15. Considers that his/her recovery will be more a matter of luck than work* | .49 | |||
| 16. Believes to be a resourceful person capable of solving problems easily | .68 | |||
| 17. Gives up easily when unable to perform a certain self-care task* | .56 | .47 | ||
| 18. Believes in his/her merit, is proud of oneself, and has a positive perception of his/her qualities | .68 | |||
| 19. Has a realistic expectation of his/her recovery possibilities 20. Cultural, spiritual, and religious beliefs and/or health issues may be hindering his/her involvement* | .61 | |||
| 21. He/she understands being able to have the necessary control over his/her actions to meet the established goals 22. Expresses the feeling of worthlessness in life* | .73 | |||
| 23. Demonstrates initiative and shows dedication in the performance of self-care activities | .75 | |||
| 24. Expresses feelings of hope related to his/her recovery | .79 | |||
| 25. Displays confidence in performing self-care tasks | .71 | |||
| 26. Reveals signs of anxiety, insecurity, sadness, and/or despair* | .62 | |||
| 27. Shows to be melancholic, with loss of appetite and/or insomnia* | .49 | |||
| 28. Expresses fear (of having a relapse, loneliness, falling, feeling pain, social stigma...) * | .65 | |||
| 29. Expresses helplessness and sadness associated with lack of company* | .66 | |||
| 30. Verbalizes willingness to learn | .66 | |||
| 31. Searches for information (from other patients with a similar health condition, professionals, internet...) | .73 | |||
| 32. Asks questions about the evolution of his/her health condition | .73 | |||
| 33. Establishes goals for the future | .69 | |||
| 34. Has previously lived an experience that is hindering the acquisition of self-care skills* | .88 | |||
| 35. Has knowledge or prior learning that is facilitating his/her recovery process | .91 | |||
| 36. Uses behaviours that help him/her to maintain the well-being based on a prior experience | .93 | |||
| 37. Expresses feeling a "burden" to the people on whom he/she depends on carrying out daily life activities* | .65 | |||
| 38. Admits that it is time for others to replace him/her in carrying out daily life activities* | .64 | |||
| 39. Gets visibly sad and/or says he/she is completely worthlessness when unable to perform a task by himself/herself 40. Reports having no problem in using technical help if this is needed to improve self-care | .60 | |||
* Inverted items
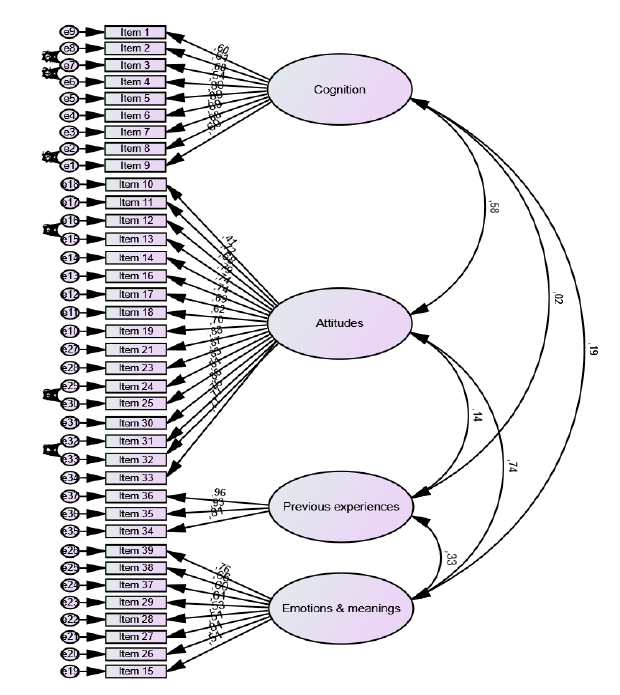
After excluding the items with a factorial load below 0.45 and analysing the differences between the results obtained and the theoretical baseline matrix, the theoretical model was reformulated and tested through the CFA. The results showed a poorness-of-fit of the measurement model with a value of X2 (623, N=118) = 1231.17, p<0.001, RMR=0.074, CFI=0.810, RMSEA=0.091, 90% CI [0.084, 0.099], p (RMSEA≤0.05) <0.001. The analysis of the parameter estimations revealed that the factors were highly correlated and that all standardized indexes saturated in the corresponding factor, with factorial weights ranging from 0.41 to 0.96 (all p < 0.001). The standardized residuals were analysed to identify possible sources of significant differences indicating the poorness-of-fit and the suggested modification indexes. The model was re-specified with the correlation of errors. The values of the final re-specified model showed indicators of better adjustment to the previously developed theoretical model (figure 1), with the following results: X2 (616.0 N=118) = 1028.951, p<0.001, RMR=0.072, CFI=0.890, RSMEA=0.076, 90% CI [0.068, 0.084], p(RMSEA≤0.05) <0.001. Cognition showed no significant statistical relation with previous experiences, nor with emotions and meanings. In addition, no statistical association was found between behavioral disposition and willingness to learn with previous experiences.
The internal consistency value of each sub-scale was assessed by the Cronbach's alpha coefficient (Table 3). All sub-scales showed good internal consistency values.
Table 3 Internal consistency values, mean and standard deviation of the AAS-ReSC sub-scales
| Sub-scale | Number of items | M(DP) | Cronbach alpha |
|---|---|---|---|
| Attitudes/willingness to learn | 17 | 2.74(0.76) | 0.96 |
| Cognition | 9 | 3.70(0.43) | 0.90 |
| Emotions/meanings | 8 | 3.28(0.64) | 0.84 |
| Previous experiences | 3 | 1.51(1.46) | 0.91 |
Cognition was the sub-scale scoring the highest mean values. Previous experiences sub-scale scored the less and showed greater variation. Age correlated negatively (r=-0.27; p<0.001) with the behavioral dispositions and cognition sub-scales (r=-0.29; p<0.001), showing that the older the participants, the greater the impairment of thinking and memory capacity, and less favourable attitudes towards the health recovery process. On the other hand, schooling showed a positive correlation with the attitudes sub-scale (r=0.19; p<0.05), suggesting that people with higher schooling had more favourable attitudes towards the process of recovering autonomy.
3. Discussion
Studies have demonstrated that following an injury, people with self-care deficit become more vulnerable, with feelings and emotions such as fear, hopelessness, discouragement, sadness for finding themselves dependent on others, strongly conditioning the attitude towards the self-recovery process (Schemitsch & Nauth, 2020; Whitson et al., 2016). Studies have been mainly focused on bodily processes as a predictive factor in recovering a person's self-care ability after an acute event. Research on attitudes and emotions associated with this process has been limited to the use of multiple and specific instruments. Thus, clinical practice would highly benefit from a broader instrument that allows professionals to extend the study of attitudes and emotions. When the person’s potential to recover independence is hindered by the feeling of fear (e.g., of falling again) because of the meaning attributed to the event that caused the injury, the intervention should primarily focus on the process of reconstructing the person’s self-confidence and self-efficacy, while physiotherapy programmes are initiated. This instrument allows a better evaluation of the emotional aspects and attitudes that significantly affect the recovering self-care process after an acute event. Thus, this methodological study aimed to validate the AAS-RecSC, currently developed by a group of experts. The use of two factorial analysis techniques with the same sample is rather unusual. Nevertheless, the EFA was conducted to eliminate the items with low factorial load, which poorly contributed to explain the factor and understand the items' behaviour according to the dimensions determined a priori. Moreover, the CFA was run to analyse the adjustment of the model to its theoretical basis.
Following this analysis, the allocation of three items was considered. All of the willingness to learn items were grouped with the items concerning behavioral dispositions. It also seems easier to accept that the willingness to learn is more likely a form of behavioral dispositions. Despite their intrinsic value and causal distribution, the items related to attributed meanings lead to emotions of dependency and burden. Thus, its reorganization into a component shared by two initial dimensions is more appropriate.
The older the participants, the more difficult it is for them to learn and embrace new treatments to regain their health (Ferreira et al., 2011). Studies show that the cognitive capacity decreases with increasing age and the presence of comorbidities (Ferreira et al., 2011; Ahn et al., 2021). Thus, these adults need more support and resources due to their dependence on self-care. Adults with higher schooling have better adherence to treatments and are more capable of taking advantage of available resources to acquire more autonomy. This perception of autonomy and independence gains and its recovery process helps dependent people reduce their negative perception of dependency and the stigma associated with resorting to technical help (Fraser et al., 2016).
This study had one important limitation. Due to the COVID-19 pandemic, the sample size was below what we expected since less than 200 participants accepted to participate. The recommendations for calculating the sample size based on the corresponding item ratio range from 5:1 (e.g., five participants per scale item) to 30:1 (Tsang et al., 2017). There are no absolute metrics to calculate the sample size needed to validate a questionnaire, but larger samples are always recommended (Tsang et al., 2017). Considering that a minimum of 100 participants is suggested when using a multivariate technique (Anthoine et al., 2014), further research is needed with extended samples to analyse the instrument behaviour. Considering the multidimensional format of this instrument, the authors recommend a more detailed study of this measure, namely the concurrent validity with other variables, its stability and the predictive validity.
Conclusion
A balanced model was identified with reasonable adjustment indexes, ensuring reliability, construct, and factorial validity in assessing the attitudes dimensions. However, further studies should be developed to explore other psychometric characteristics of the instrument and achieve greater robustness in its clinical application.