Introduction
During the endodontic treatment, the overpreparation of mandibular premolars’ and molars’ root canals may facilitate further extrusion of the intracanal medicament (ICM) and/or root canal filling material from the root apices, causing neurological complications, such as Nicolau Syndrome also known as embolia cutis medicamentosa.1 Nicolau Syndrome consists of a cutaneous adverse reaction at the site of a particular drug application, such as hypoesthesia, dysesthesia, and anesthesia, in areas innervated by the inferior alveolar nerve (IAN).2 Injuries to the IAN during dental treatment are uncommon but represent a serious complication.3 Namely, they may result in permanent paresthesia, defined as a sensitivity loss lasting more than 6 months.4 Facial paresthesia is often felt via the mental, lingual, and IANs. The main symptom is a loss of sensation in the affected nerve area, although the patient may have also altered perceptions of hot and cold, tingling, itching, and numbness later on.5
Calcium hydroxide is used as an ICM during the endodontic procedure due to its high bactericidal effect and alkalinity.6 With Ca+2 and OH− ions, calcium hydroxide has an antibacterial effect and reduces the production of hard tissue.7 Moreover, some authors reported that it has an osteoblastic impact on inflamed tissue in the periapical region.8
Several possible mechanisms and treatment options exist when an endodontically treated tooth develops an atypical symptom.9 Possible injury mechanisms include pressure, neurotoxic effects, and mechanical trauma. Considering that trauma, pressure, and neurotoxicity during endodontic treatment procedures may cause nerve damage, the clinician should choose between eliminating and monitoring pain and inflammation and surgically removing the cause.10-13 However, some studies suggested a non-surgical approach for managing such complications.14-18
Pregabalin is a gamma-aminobutyric acid (GABA) analog with the same structure and action as gabapentin that is effective in chronic and neuropathic pain. It has an analgesic effect by reducing neurotransmitter release.19-21 The presente case report intends to debate the clinical condition of a patient who was presenting with pain and paresthesia caused by calcium hydroxide extrusion and who recovered completely with a non-surgical approach using pregabalin and steroids.
Case report
On May 27, 2019, a 45-year-old female patient attended na endodontic consultation with a chief complaint of pain and numbness over the left lower lip region for 2 months. The medical history and radiograph analysis revealed that a root canal treatment had been initiated on the mandibular left second molar (tooth 37). The patient had been experiencing left lower lip paresthesia since then. The periapical radiographic examination also revealed an apparent ICM extrusion on tooth 37 (Figure 1). Panoramic radiography was performed (Figure 2) to assess the degree of ICM extrusion, and the area of paresthesia was delimited by tactile exploration with the explorer (Figure 3). The patient was diagnosed with a previously initiated root canal treatment with symptomatic apical periodontitis associated with lower lip parestesia possibly provoked by ICM extrusion. The previous doctor later confirmed that the extruded material was calcium hydroxide. Root canal treatment continuation was recommended to the patient, associated with pharmacological therapy aiming to reverse the neurological damage. After the patient’s acceptance, anesthesia and isolation were performed, and acces to the canal space was re-established. The ICM (Ca(OH)2) was removed from tooth 37’s root canal system space with a saline solution using a 37 gauge needle. However, the extruded ICM in the inferior alveolar canal could not be removed. Root canal treatment was performed for tooth 37 according to the European Society of Endodontology’s 2006 quality guidelines. Root canal instrumentation was performed using the Protaper Universal system (Dentsply, Ballaigues, Switzerland). Following the manufacturer’s instructions, the mesial root canals were prepared up to F2 and the distal ones up to F3. Irrigation was performed with sodium hypochlorite at 5.25% and saline solution. The tooth was obturated with gutta-percha and Sealapex
(Sybron Kerr, Romulus, MI, USA) sealer with a continuous wave of condensation technique. Analgesics and antibiotics were prescribed for 3 days. Steroids (Predniheal 20mg SSR Healthcare, Nagpur, India; the dosage [two doses] was tapered and stopped in two weeks) and pregabalin (Lyrica 75mg Pfizer, Mumbai, India; 150 mg per day) were prescribed for 1 month. One week later, the root canal treatment was completed (June 2019).
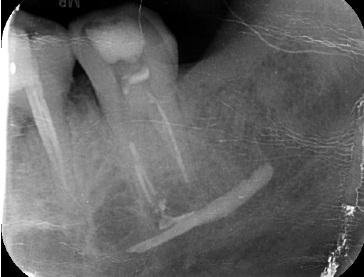
Figure 1 Pre-operative periapical radiograph evidencing the presence of an intracanal medicamente inside the mandibular canal
In an 8-month follow-up visit (February 2020), the area of paresthesia was reduced (Figure 4), and tooth 35 was extracted for reasons non-related to the present report. Due to the Covid-19 pandemic, the patient could not perform the following evaluation visit. However, in a telephone conversation, she mentioned being asymptomatic and wanting further clinical evaluation. In September 2022, because the patient was bedridden due to a road traffic accident, a home visit was performed to assess the degree of paresthesia. Clinical examination suggested complete resolution of the paresthesia, and a periapical radiograph revealed the absence of ICM near the root apices of tooth 37 (Figure 5). In a 4-year follow-up (June 2023), the patient was asymptomatic. Prosthetic rehabilitation was done (Figure 6), and the complete resolution of calcium hydroxide was evident in the panoramic radiography (Figure 7).
Discussion and conclusions
Paresthesia is the permanent or temporary sensation of tingling, tickling, or prickling.22Mechanical preparation with excessive root canal working length on mandibular molars and premolars and endodontic material extrusion are potential iatrogenic causes of IAN damage.23 Most cases of endodontic paresthesia result from an overpreparation or overfilling of the mandibular canal with endodontic materials.1,24 These cases of paresthesia occurring during and after root canal treatment of molars and premolars have been the subject of previous reports.25,26
At body temperature, calcium hydroxide has a low solubility. Serper et al.27 showed that calcium hydroxide may cause foreign body reactions, nerve inflammation, and bone necrosis.
In addition, when an excess of calcium hydroxide remains in the nerve tissue for more than 30 min, it may cause irreversible obstruction of nerve conduction, resulting in an imbalance in the nerve membrane potential. The first sign of calcium hydroxide extrusion in the mandibular canal is pain persisting after the anesthesia has disappeared.28 The literature shows that extrusion can induce transient inflammation ranging from mild to severe.29,30 It may be accompanied by pain on percussion and palpation due to local inflammation and lower lip or ear pain or numbness, which is a combination of signs of mechanical trauma and inferior dental neuritis.31 In some patients, anesthesia may persist.2,13,23,32
Pregabalin, an analog of the inhibitory neurotransmitter GABA, is mainly used in the treatment of trigeminal neuropathic pain and chronic pain.19,33 It is also often used in peripheral neuropathic pain.17,34 The United States Food and Drug Administration (FDA) (2004) has approved the use of two drugs for peripheral neuropathic pain: duloxetine and pregabalin. Pregabalin, which has an analgesic effect, improves symptoms significantly in 1 week and remains effective during the treatment.35,36 Its oral bioavailability is approximately 90%, with peak plasma levels occurring after approximately 1 hour.
Pregabalin is not protein-dependent, with a plasma half-life of 6 hours that is not dose-dependent. It has fewer drug interactions and little effect on hepatic enzymes.37 While renal excretion accounts for 95% of the oral dose, hepatic metabolism is insignificant. Pregabalin administration is an effective and well-tolerated treatment for neuropathic pain.38 In the presente case, pregabalin treatment was initiated based on existing documented evidence, considering the nerve damage that causes neuropathic pain after calcium hydroxide extrusion to the mandibular canal.
The present 4-year follow-up case report revealed the complete resolution of paresthesia and the disappearance of ICM extrusion with the non-surgical approach. The combination of steroids and pregabalin may be considered a viable option for complete resolution of paresthesia.
In conclusion, ICMs are prone to induce neurotoxic effects following extrusion into the inferior alveolar canal. The clinician should be cautious while preparing the root canal system space to avoid apical violation or overfilling with the ICM or obturating materials. The non-surgical treatment should be considered a viable initial approach over surgical management.





















