Introduction
The oral cavity favors bacterial community development, providing a suitable environment for organized and complex species of several degrees of virulence to grow due to its humidity and temperature,1,2among other factors. The oral microbiota of a healthy person is usually balanced, with the predominance of Gram-positive streptococci. Biofilm development, however, favors association with Gram-negative anaerobic bacteria and fungi. An increase in biofilm pathogenicity occurs in the first 48 to 72 hours of intensive care unit (ICU) hospitalization, leading to a higher systemic complication risk.3-5
Hospital ICUs are responsible for the treatment of critical patients, mostly affected by acute diseases or chronic disease complications,6,7 and generally at imminent risk of death. In general, ICU patients present lip resection and salivary flow alterations.8 Decreased salivary flow consequent to medication administered favors the growth of oral pathogenic microorganisms, impacting oral health.1,8
The dentist’s assistance during hospitalization is importante for oral health promotion. During this period, patients may present oral alterations locally originated by traumas, infections, and neoplasms or systemically originated by medications, basic diseases, and the patient’s immunosuppression state, which may, in turn, influence the evolution of the patient’s general health.9 Chemical stomatitis, or chemical damage to the mucosa, is a type of traumatic injury caused by the contact of oral tissues with chemicals and drugs improperly administered.10
Some patients, especially children or those undergoing psychiatric treatment, may keep the drugs in their mouths instead of swallowing them, causing clinically significant damage.10
Clinically, chemical stomatitis appears as a whitish, pleated plaque, which may detach from the underlying tissue and show a red, hemorrhagic conjoined tissue associated with painful symptoms.11 Oral care and oral lesions monitoring during ICU hospitalization aims to control the development and maturation of a more pathogenic biofilm in various oral cavity sites, as biofilm volumes increase rapidly and intensely in patients during hospitalization due to their critical health status and hygiene dependence.8 Moreover, oral care is often neglected or performed inappropriately when not part of a pre-established care routine.8 In this context, the present study aims to report the clinical case of an adolescent patient with chronic renal disease who, during an ICU hospitalization, suffered significant oral alterations.
Case Report
A 14-year-old male patient with chronic renal disease and participant in the Replacement Renal Therapy - Peritoneal Dialysis program, due to treatment-related complications, evolved to bacterial peritonitis. This situation required dialysis treatment mode alterations, so the patient initiated hemodialysis and was admitted to a pediatric ICU.
The patient’s medical history indicated many types of medication, including calcium carbonate 500 mg capsules.
The person in charge reported that the patient exhibited difficulty in swallowing the calcium carbonate capsules, so he would open them and release their content directly into the oral cavity. However, according to the medical team’s recommendations, this medication should only be ingested in capsule form. After recurrent administrations in the oral cavity, the patient developed extensive oral lesions associated with chemical burns and several bleeding points with highly painful symptoms. This condition prevented him from eating, requiring a nasogastric tube-administered diet.
Due to the clinical characteristics of the lesions and because he was a patient with chronic kidney disease, the hypothesis of uremic stomatitis was considered. However, this diagnosis was discarded after observing that the patient had serum urea levels of 74 mg/dL.
The initial clinical examination revealed many crusts associated with poor hygiene. Thus, hygiene was carried out with gauze and 0.12% alcohol-free chlorhexidine, following the established hospital protocol. Subsequently, ulcerated, bleeding lesions were observed on the inner lip, jugal mucous membranes, hard palate, and soft palate (Figure 1).
The diagnostic hypothesis put forth was chemical stomatitis. Lesions were treated with a topical corticosteroid -clobetasol propionate 0.5 mg/g gel- with 6-hour intervals between applications. Concomitantly, low-intensity laser
photobiomodulation was initiated as an adjuvant treatment agent to accelerate the healing process and decrease painful symptoms employing the following protocol: Laser Hand Duo (MM Optics LTDA); continuous operation mode; semiconductor light-laser emitter (GaAIAs and InGaAIP); 100 mW power; 0.03 cm² spot; 660 nm wavelength; 33.3 J/cm² energy density, 10 seconds/point in the lip, tongue, jugal mucosa, hard palate, and soft palate regions, along the entire length of the lesion; 1-cm distance between each point of application. The laser tip was placed perpendicularly and near the tissue, respecting the patient’s possible discomfort when touching the tissue. Each region received ten 1 J/point, 60 J per day/session. In total, 480 J of energy were delivered with a total irradiation time of 4800s. Eight sessions were performed at 24-hour intervals until total lesion regression (Figures 2 and 3).
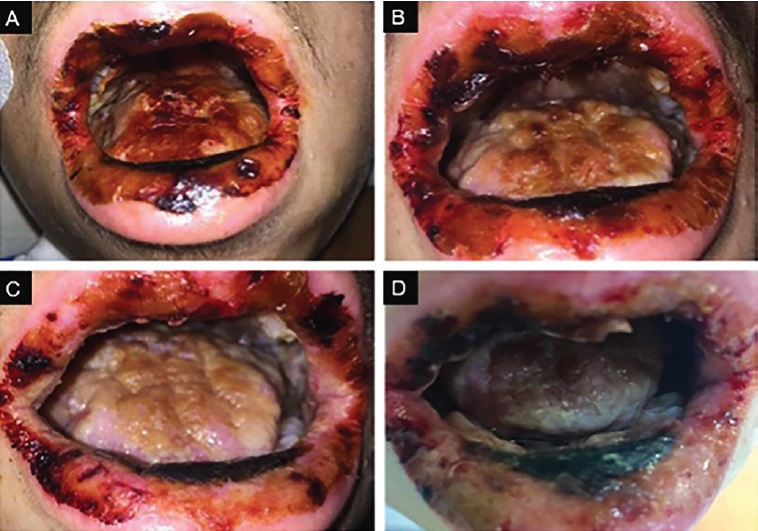
Figure 2 A) Evolution of the lesion after the second laser photobiomodulation session. B) Evolution of the lesion after the fourth laser photobiomodulation session. C) Evolution of the lesion after the sixth laser photobiomodulation session. D) Evolution of the lesion after the eighth laser photobiomodulation session
The initial clinical examination revealed many crusts associated with poor hygiene. Thus, hygiene was carried out with gauze and 0.12% alcohol-free chlorhexidine, following the established hospital protocol. Subsequently, ulcerated, bleeding lesions were observed on the inner lip, jugal mucous membranes, hard palate, and soft palate (Figure 1). The diagnostic hypothesis put forth was chemical stomatitis. Lesions were treated with a topical corticosteroid -clobetasol propionate 0.5 mg/g gel- with 6-hour intervals between applications. Concomitantly, low-intensity laser photobiomodulation was initiated as an adjuvant treatment agent to accelerate the healing process and decrease painful symptoms employing the following protocol: Laser Hand Duo (MM Optics LTDA); continuous operation mode; semiconductor light-laser emitter (GaAIAs and InGaAIP); 100 mW power; 0.03 cm² spot; 660 nm wavelength; 33.3 J/cm² energy density, 10 seconds/point in the lip, tongue, jugal mucosa, hard palate, and soft palate regions, along the entire length of the lesion; 1-cm distance between each point of application. The laser tip was placed perpendicularly and near the tissue, respecting the patient’s possible discomfort when touching the tissue. Each region received ten 1 J/point, 60 J per day/session. In total, 480 J of energy were delivered with a total irradiation time of 4800s. Eight sessions were performed at 24-hour intervals until total lesion regression (Figures 2 and 3).
The patient reported considerable improvement in the painful symptomatology after the first laser photobiomodulation session. The dental team assessed the effectiveness of the photobiomodulation process through clinical examination.
The oral mucosa exhibited the clinical appearance of a healed tissue following treatment.
Discussion and conclusions
The patient reported herein had chronic renal disease and underwent peritoneal dialysis as a replacement renal therapy due to significant renal system involvement. One of the most frequent complications associated with peritoneal dialysis is peritonitis, a condition where inflammation of the membrane covering the abdominal cavity organs and the internal wall of the abdomen occurs because of intense manipulation during dialysis, making it more susceptible to infections, resulting in peritonitis and requiring ICU treatment.12,13
Patients who undergo chronic dialysis require a large drug arsenal, which may include antihypertensives and calcium carbonate supplementation. The latter is required for vitamin D activation and control of the calcium blood level decrease, consequent to the decreased kidney function and aggravated by excess phosphorus in the blood, leading to calcium reabsorption from the bone. Thus, supplementation may be administered to correct this deficiency and avoid hypocalcemia.14,15
The patient evolved to chemical stomatitis due to inadequate calcium carbonate administration. Many drugs cannot be crushed or have their contents extracted from their capsules due to the risk of complications, including therapeutic failure, drug-nutrient interaction, biological risk due to carcinogenic potential, and damage to the gastrointestinal tract, as noted in this case report.16
After a complete evaluation, it was concluded that, although the patient’s lesions appeared because of poor drug administration, they intensified due to poor oral hygiene and, especially, due to a sharp decrease of the salivary flow, common in patients with chronic kidney disease and in individuals admitted to the ICU because of administered medications.17-19
The hypothesis of uremic stomatitis was also considered. It is a condition of the oral mucosa associated with uremia in patients with chronic renal failure with serum levels above 200mg/dL. It presents with various clinical types, with the ulcerative form being the most common.20-24In the present case, the hypothesis was discarded after observing the patient’s 74mg/dL serum levels.
Laser photobiomodulation, formerly known as low-power laser therapy, was used for the treatment. It uses irradiation with wavelengths in the red and infrared ranges and includes various types of radiation, such as electromagnetic, broadband lights, LEDs, and lasers.25,26 It is a non-invasive therapy that, when applied to the mucous membranes, is absorbed by endogenous chromophores such as mitochondria, causing photophysical and photochemical events through biological pathways.27,28Depending on the dose of energy used, it can have anti-inflammatory, analgesic, and healing properties. It has been increasingly used in dentistry as an alternative for treating inflammation and wounds in the oral cavity. Laser photobiomodulation increases the universal energy source -adenosine triphosphate- intracellularly and reduces oxidative stress, which is its accepted primary mechanism of promotion of healing. Moreover, its analgesic activity is probably induced by an inhibitory effect on A and C neuronal pain fibers, with the modulation of neuroperception, slowing of neural conduction velocity, reduction of action potentials amplitude, and suppression of neurogenic inflammation.29,30
Corticosteroids were applied topically to the mucosa for joint treatment with laser photobiomodulation to potentiate the anti-inflammatory effects due to the severity of the presente clinical condition. The literature reports other oral conditions also treated with this association, such as Graft versus Host Disease. In turn, other studies prove the efficacy of laser photobiomodulation as a first-line therapy in the treatment of lesions in the oral cavity.31,32 Besides its easy access, photobio-modulation is also promising due to being a non-pharmacological treatment that can spare patients from adverse effects.
Based on the applied protocol and the patient’s evolution presented in this clinical case, the association of laser photobiomodulation with topical corticosteroids was proven an effective alternative for oral lesion treatment, especially in ICU patients.
This therapy acts by stimulating healing, analgesia, and inflammation modulation effects, contributing to general patient health and reducing hospitalization lengths of critical patients.

















