Introduction
The successful outcome of endodontic treatment relies on na interplay of numerous factors encompassing biological, technical, and patient-related variables.1 Among these factors, a profound understanding of the tooth’s intricate anatomical characteristics and root canal system, the identification of anatomical variations, and the location of all canals are imperative for anticipating potential errors, which is crucial for achieving a favorable prognosis in preserving both the functionality and longevity of the tooth.2,3
Studies on multi-rooted teeth have consistently unveiled anatomical variations that deviate from the typical morphological and canal configuration expected for each tooth.4-7While most mandibular molars typically exhibit two roots-one mesial and one distal, the existence of a third root renders these teeth prime candidates for unexpected anatomical complexity.3,8 These additional root structures are commonly located in distolingual or mesiolingual positions, denoted as radix entomolaris (RE) and radix paramolaris (RP) correspondingly, and possess distinctive canals.9,10 Among these variations, RE is the most prevalent and may manifest as a distinct, separate root or a partial fusion with the main roots. RE may occur in any mandibular molars but has been least documented in second molars.9 Its prevalence has been reported to vary among populations, with about 4% in Caucasians and over 30% in Mongolian populations.3,8-10
Detecting these anatomical root variations poses a significant challenge due to their location within the same bucolingual plane as the distal root.9 This spatial proximity can lead to superimposition on orthogonal periapical radiographs, making this anatomical variation easy to overlook. Failing to identify and treat an additional root canal during the root canal treatment has been associated with a high probability of post-treatment apical periodontitis.11
Given the clinical implications of missing these anatomical variations, it is important for clinicians to remain observant and informed about the potential presence of additional roots in mandibular molars when performing root canal treatments. In this context, this study presents three cases of RE and RP, offering additional awareness and insights into their clinical management to ultimately enhance the success rates of root canal treatments in mandibular molars.
Case reports
General clinical procedures
Three patients, each reporting pain in a mandibular molar, were referred for an endodontic evaluation by colleagues within a multidisciplinary private practice following their initial dental assessments. Their medical history was reviewed and considered non-contributory in all cases. The intra-oral inspection revealed large crown fillings not associated with visible caries lesions and the absence of periodontal probing or bleeding. Teeth mobility was within the physiological limits.
Radiographic examination and ice sensitivity tests were also conducted to collect complementary data for the diagnosis.
The three cases were classified as highly difficult, according to the American Association of Endodontists’ endodontic case difficulty assessment form, due to their anatomical variations and complexities.12 Proper pulpal and apical diagnoses were established, and root canal treatment was recommended. The patients accepted the proposed treatment and signed its informed consent form.
After proper mandibular nerve block infiltration (1.8 mL of 4% articaine with 1:200,000 epinephrine; Artinibsa, Inibsa, Spain), an adequate rubber dam isolation was achieved. The access cavity was prepared using round and endo-z endodonrev tic burs, and the pulp floor morphology was inspected under an 8.5x magnification with a dental microscope (Opmi Pico, Carl Zeiss Surgical, Germany). All teeth’ chamber floors presented dark embryological lines that indicated the location of the multiple root canal orifices. After refining the canals’ entrances with ultrasonic tips (Start X, Dentsply Maillefer,
Switzerland), the root canals were negotiated, and patency was achieved with stainless-steel ISO size-10 K hand files (Dentsply Sirona, Switzerland). The working length was double- checked with periapical radiographs and an electronic apex locator (Root ZX, Morita, Japan). The mechanical instrumentation of all canals used the ProTaper Next (Dentsply Sirona, Switzerland) rotary system, according to the manufacturer’s recommendations. Finishing was completed using X2 instruments in the mesial canals and X3 files in the distal.
The mechanical debridement was complemented with a copious syringe irrigation with a minimum of 36 mL of 5.25% sodium hypochlorite per tooth using a side-vented 27 G needle (Monojet, Covidien, Mansfield, USA). The teeth were closed using a provisional filling (Cavit W, 3M ESPE, Germany).
A second appointment was scheduled to follow up properly on the initial symptoms. No intracanal dressing was used between visits.
At the second appointment, the patients were already asymptomatic and comfortable. After the anesthesia, rubber dam isolation, and regaining endodontic access, a final irrigation protocol was completed with 1 mL of 17% EDTA for 30 seconds and 3 mL of 5.25% sodium hypochlorite rinses per canal.
The canals were dried with paper points, and X2 and X3 gutta- percha master cones (ProTaper Next Conform Fit Gutta-Percha, Dentsply Sirona, Switzerland) were fit at the working length. The root canal obturation used a resin-based sealer (AH Plus, Dentsply Sirona, Switzerland) and was accomplished by the continuous wave of condensation technique using the System B unit (Sybron Endo, USA) for down packing, selecting the appropriate plugger size that binds at 4-5 mm from the apical limit of each canal and Obtura II (Obtura Spartan, USA) for backfilling. Finally, the pulp chamber was cleaned with alcohol, the canal orifices were sealed with a flowable resin (Supraflow, R&S, France), and the endodontic access was again restored with a provisional filling (Cavit W, 3M ESPE, Germany).
The cases were referred to oral rehabilitation, and follow-up visits were scheduled.
Case #1
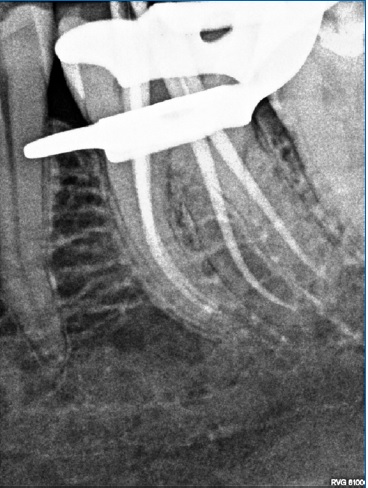
A 46-year-old Caucasian female came to the endodontic appointment complaining of permanent pain on the left mandibular first molar (tooth 36). Oral inspection revealed a buccal fistula and symptoms on percussion. The tooth did not respond to the ice sensitivity test, and the radiographic examination showed a large deep filling on the crown’s distal aspect and an extra distal root (Figure 1). A diagnosis of pulp necrosis with chronic apical abscess was made, and root canal treatment was recommended. After proper endodontic access was achieved, the dark lines of the pulp chamber floor revealed two root canal orifices in its mesial and distal portions. Distolingual canal negotiation made evident a more pronounced angulation on the canal entrance, suggesting this root as the additional one and making it possible to catalog it as an RE. After gaining the canal patency, the angulation was smoothly rectified using an SX file (ProTaper Gold, Dentsply Sirona, Switzerland), and all canals were shaped and disinfected. Two weeks after the initial appointment, the canals were obturated according to the description above (Figures 2, 3, 4, and 5). At a 27-month follow-up, the patient was asymptomatic, her fistula had completely healed, and the periapical tissues appeared normal on radiographs. (Figure 6).

Figure 2 Pulp chamber floor with dark embryological lines after root canal shaping, showing four root canal entrances.
Case #2
A 35-year-old Caucasian female attended an endodontic appointment, reporting intense pain, mostly associated with cold drinks, on tooth 36. Oral and radiographic examination showed a deep amalgam filling and a third root between the usual mesial and distal roots (Figure 7). The ice sensitivity test confirmed prolonged pain lasting for over 30 seconds. A diagnosis of symptomatic irreversible pulpitis with normal apical tissues was made. Root canal treatment was suggested and accepted by the patient.

Figure 7 Initial radiographic condition showing a third root between the usual mesial and distal ones.
Following anesthesia, rubber dam isolation, and cavity access, the endings of the dark embryological lines in the pulp chamber floor were scouted using a DG16 endodontic explorer, revealing four root canal entrances (mesiobuccal, mesiolingual, distobuccal, and distolingual). The canal entrances were rectified using ultrasonic tips. The negotiation of the distolingual root canal and canal entrance was particularly challenging, and this additional root was defined as an RE. The root canals were then chemo-mechanically prepared and obturated, as previously described (Figures 8, 9, 10, and 11). At the 8-month follow-up, the tooth was asymptomatic, and its radiographic examination showed normal periapical tissues (Figure 12).
Case #3
A 51-year-old Caucasian female came to an endodontic consultation reporting intense pain that tended to increase with cold on the right mandibular second molar (tooth 47). The patient’s examination showed that the tooth was symptomatic on percussion and had a large, deep resin filling (Figure 13).
The ice sensitivity test recorded an intense and prolonged response. The patient was diagnosed with symptomatic irreversible pulpitis with symptomatic apical periodontitis and agreed to the root canal treatment suggested.
Prior to the treatment, the clinician examined a previously performed cone-beam computed tomographic volume and confirmed a three-rooted configuration. The disposition of the three roots enabled classifying the mesiobuccal root as an RP as it was off-centered, while the other two roots (mesial and distal) were very close and aligned mesiodistally (Figure 14). Following anesthesia, isolation, and endodontic access opening, an inspection of the chamber floor and its dark embryological lines revealed two root canal entrances in the mesial and distal parts of the chamber and a third entrance positioned off-centered toward the mesiobuccal direction. The root canal treatment followed the steps previously described (Figures 15, 16, 17 and 18). At the 6-month follow-up, the tooth, which was not definitively restored yet, was asymptomatic, and there was no radiographic evidence of apical pathology (Figure 19).
The patient was strongly advised to have an urgent appointment for the restoration.
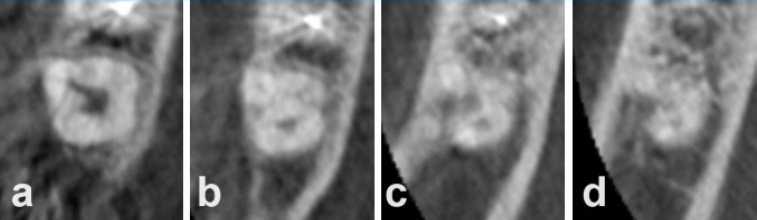
Figure 14 Cone-beam computed tomography axial slices of tooth 47: (a) pulp chamber with an off-center mesiobuccal deviation, (b) coronal portion, (c) middle portion showing an off-centered mesiobuccal root, (d) apical portion of the roots
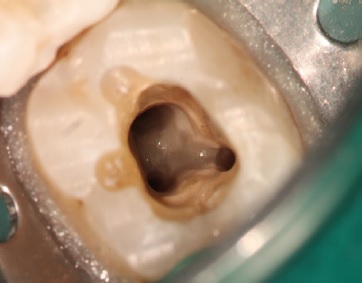
Figure 15 Pulp chamber view revealing an off-centered root canal entrance toward a mesiobuccal direction.
Discussion and conclusions
These case reports emphasize the significance of comprehensive clinical and radiographic examinations and a thorough understanding of dental anatomy when diagnosing and treating teeth with RE or RP. These anatomical variations involve extra roots in mandibular molars, which, although uncommon, Figure 15. Pulp chamber view revealing an off-centered root canal entrance toward a mesiobuccal direction. Figure 17. Pulp chamber view after root canal filling. Figure 16. Master cone radiograph Figure 18. Post-endodontic treatment radiograph. can significantly influence the prognosis of endodontic treatment if the extra root canal is missed or if the canals are not adequately debrided.1,3,13 The successful treatment outcomes in all three cases relied on crucial factors, including precise identification of the extra root, accurate diagnosis, and effective management of these anatomical variations.
Detecting these additional roots before initiating treatment is essential to ensure accurate diagnosis and formulate appropriate treatment plans. However, it requires a meticulous examination of various crown features that may serve as indicators.
One such key feature is the presence of an extra cusp, often accompanied by a distinct distolingual lobe and cervical convexity, which should immediately raise suspicions of na additional root.9,14 Furthermore, a comprehensive review of periapical radiographs, taken at various angulations, may reveal subtle yet crucial details indicating these additional roots.15 While it is feasible to identify an additional root using two-dimensional radiographs, previous studies have shown that cone-beam computed tomography (CBCT) is a superior method for assessing dental structures.16,17 CBCT not only excels at confirming the existence of anatomical variations such as additional root and missed canals, but it is also invaluable for precisely pinpointing their location and orientation.2,18 This capability proves especially vital in distinguishing RE from RP.
Case #3 serves as a prime example of CBCT’s significance in making a definitive diagnosis that categorizes the additional root in the buccal plane as an RP, a task that might be considerably more challenging with only conventional periapical radiographs.
While recognizing the additional root’s presence is indeed pivotal, the subsequent location and effective cleaning of its canal can be a formidable challenge. Hence, the design of na appropriate access cavity holds paramount importance, as it not only guarantees superior visualization of the entire pulp chamber floor but also establishes a direct, unobstructed pathway to the canal orifices.9,19 The orifices of the additional root canals have been described as typically located in the lingual position, either mesially or distally from the distal root canal.20This distinct positioning implies that the conventional access cavity preparation may not adequately expose these orifices, often requiring a larger access cavity.9,10
When locating the canal’s orifice becomes challenging, a meticulous examination of the pulp chamber floor and walls, particularly in the distolingual region, becomes imperative.2
In the presented cases, careful evaluation of the pulpal floor by tracing the dark embryologic line with an endodontic explorer (DG16) was crucial for locating the canal. This approach helped unveil the overlaying remnants of the pulp roof that obscured the entrance to the root canal. The incorporation of a dental microscope proved to be immensely advantageous in locating the canals more precisely. These optical tools significantly enhance the accuracy of the examination, facilitating a more thorough and effective exploration of the intricate dental anatomy.21
Additionally, the canals within this extra root have been described as having smaller diameters and may exhibit curvatures in various portions, including the coronal, middle, or apical thirds, which increases the risk of encountering shaping errors during the endodontic procedure. These errors could manifest as root canal straightening, ledge creation, root canal transportation, or even inadvertent separation of endodontic files.9,10Given these challenges, a cautious approach when preparing the canal is recommended by ensuring a smooth glide path with a small K file up to size 15 before using rotary files, as this initial preparation serves to reduce the torsional stress placed on the rotary files and helps ensure a more controlled and safe procedure.2,9,22 Also, when shaping the canals, a conservative approach using files with less taper can help mitigate the risk of over-preparation and potential errors.6 By minimizing the extent of canal enlargement, clinicians can maintain the natural anatomy of the tooth and reduce the likelihood of complications associated with excessive dentin removal. In essence, these precautions and strategies are essential to navigate the complexities associated with the extra root, ensuring a safer and predictable result.
These cases highlight the importance of understanding the varying anatomical characteristics of mandibular molars and how careful identification of additional roots, coupled with advanced diagnostic tools and techniques, can lead to successful treatment outcomes.