Introduction
Desmoid-type fibromatosis (DTF), also known as desmoid tumor or aggressive fibromatosis, is a rare monoclonal fibroblastic proliferation that arises from a variety of connective tissues, including muscle, fascia and aponeurosis. Despite its benign nature, these tumors can cause significant local morbidity from infiltration of the surrounding structures. These lesions are predominantly located in the extremities and abdominal wall1), (2), (3), (4.
DTF has an incidence of 2.4 to 4.3 per million per year and a 2- to 3.5-fold increased incidence in women, with a peak age of 30 to 40 years old. Pregnancy-associated DTF is even rarer and available research is limited1), (2), (4), (5), (6.
The etiology is multifactorial since genetic, endocrine, and physical factors seem to play an important role. The majority of DTF occur sporadically, while 5-15% are associated with familial adenomatous polyposis (FAP). Association with elevated estrogen states was hypothesized, but since estrogen receptors are not universally found in DTF, this relation is still controversial. The reported inhibitory effect of antiestrogenic agents, such as tamoxifen, also supports the role of hormonal factors in tumor development1), (3), (4), (5), (7.
Although the molecular events surrounding tumor formation are not completely understood, dysregulation of the Wnt signaling pathway, leading to accumulation of beta-catenin and fibroblast proliferation, appears to play a role in the development of both sporadic and FAP-associated aggressive fibromatosis. Approximately 90% of sporadic DTF are associated with somatic mutations in the Catenin Beta 1 gene (CTNNB1). CTNNB1 and APC gene mutations are mutually exclusive in DTF1), (2), (4.
Macroscopically, these tumors are found to be firm and, on cross section, they reveal a white, coarsely trabeculated surface that resembles scar tissue. Therefore, surgeons may have difficulty distinguishing recurrent fibromatosis from scar tissue related to prior excision. Histologically DTF is characterized by proliferating slender spindle-shaped cells separated by abundant collagenous stroma, with variable staining for smooth muscle actin, muscle-specific actin and B-catenin1), (3), (4.
Optimal management of this disorder has yet to be defined. Different modalities, including expectant management, surgery, radiation therapy, hormone therapy, targeted therapy and cytotoxic therapy have been used. The optimum treatment depends on tumor and patient-related factors, including tumor size, tumor location, and patient comorbidities. In the past, surgical resection was considered the mainstay of treatment. However the latest consensus guidelines from the National Comprehensive Cancer Network (NCCN) recommend expectant management as a primary treatment option for surgically unresectable tumors or resectable tumors that are not symptomatic, life threatening, or causing significant impairment. Nonetheless, surgical resection should be attempted in symptomatic patients or in patients with tumors that pose imminent risk to surrounding structures1), (4), (7.
The most important prognostic factor is tumor location and recurrences are seen in 20-68% of patients, typically within the first 5 years after treatment1.
We present the case of an intra-abdominal DTF arising from the retroperitoneum that was diagnosed and resected during pregnancy.
Case report
A 23-year-old female patient arrived at our emergency department with mild abdominal pain. She was 15 weeks pregnant and a bulky intra-abdominal mass was found during physical examination. The patient had no relevant antecedents besides obesity (BMI 35.5) and laparoscopic appendectomy.
An abdominal ultrasound was performed and revealed a solid mass, measuring 18.1 x 18.0 x 10.0 cm, with sparse vascularization and myometrium-like echogenicity. To better characterize the lesion, magnetic resonance imaging (MRI) of the abdomen and pelvis was requested and showed a 18.5 x 17.8 x 10.9 cm mass, attached to the uterus, with an isointense to the myometrium lesion in T1 weighted images and a heterogenous lesion in T2 (Figure 1). Administration of intravenous gadobutrol contrast suggested a cystic component. The upper limit of the mass was located at D12-L1 level and compressed the inferior right renal pole, not causing hydronephrosis nor anatomical distortions.
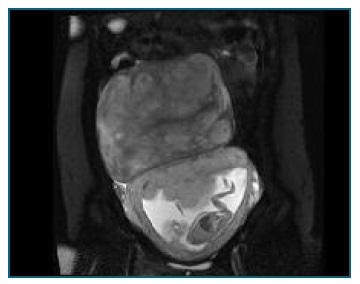
Figure 1 Magnetic resonance image: T2-weighted image showing a heterogeneous lesion measuring 18,5 cm in diameter, occupying the upper abdomen of a 16 weeks pregnant woman.
Given the imagiological findings, the first diagnostic presumption was an exophytic uterine fibroid with cystic degeneration.
The case was discussed within a multidisciplinary team. Considering the dimension and the location of the mass (which posed a space conflict with the growing fetus) and the risk of progression and complications during pregnancy (such as degeneration or torsion) it was decided to perform surgical excision at 17+4 weeks. Surgery was performed under epidural anesthesia.
During surgery, a 25 cm long mass was found in the upper abdomen and arising from the retroperitoneum, with no relation to the uterus. The procedure was complicated by an accidental section of the right ureter that was immediately repaired with an ureteral stent placement and end-to-end anastomosis. Fetal well-being was confirmed after surgery using ultrasound.
The patient had a favorable evolution during the postoperative, with urinary catheter removal in day 5 and hospital discharge in day 6.
Gross examination of the specimen showed a 20 x 17 x 12 cm mass with 2085 g. Macroscopically, the tumor was firm and the cut surface was white and trabeculated, resembling scar tissue (Figure 2). Proliferating slender spindle-shaped cells separated by abundant collagenous stroma (Figure 3) were found in histology. Polymerase Chain Reaction analysis was positive for CTNNB1 gene mutation, favoring the diagnosis of a desmoid-type fibromatosis.

Figure 2 Lesion macroscopy: A firm and well circumscribed tumor with a white and trabeculated cut surface.
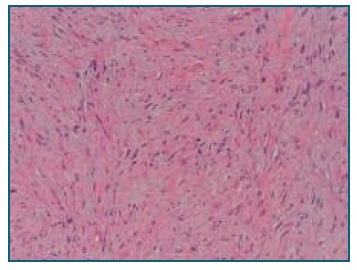
Figure 3 Lesion microscopy - Low magnification hematoxylin and eosin stain: spindled - stellate tumor cells with ill-defined borders, fibrillary eosinophilic cytoplasm, and bland nuclei.
The postoperative (8th day) got complicated by pyelonephritis, which was resolved with antibiotic therapy. Antimicrobial prophylaxis was performed throughout pregnancy. Ureteral stent was removed four weeks after surgery.
The patient suffered from iron deficiency and reactive thrombocytosis which were treated with iron supplementation. No other maternal or fetal complications were detected.
The patient had a spontaneous vaginal delivery of a healthy 3820 grams baby girl at 40+2 weeks.
There is no evidence of local recurrence after 9 months of follow-up.
Surgery and pregnancy follow-up were performed in a tertiary care hospital.
Discussion
DTF is a rare neoplastic tumor of fibroblastic proliferation that poses several diagnostic and management challenges for gynecologists. Due to the low incidence and variable presentations, they are not usually considered during the differential diagnosis of an abdominal mass. Its occurrence during pregnancy rises even greater challenges regarding diagnostic tools and treatment options.
Ultrasonography is the most frequently used imaging modality for the initial evaluation of an intra-abdominal mass but MRI is the modality of choice to characterize DTF, since it provides information on tumor invasion, depth, and neurovascular encasement, which is necessary to determine mass resectability1. In the case presented, MRI failed to detect its retroperitoneal origin, which made impossible previous ureter catheterization to prevent ureter injury.
Since the diagnostic presumption was a large exophytic uterine fibroid with cystic degeneration, possible complications such as torsion or degeneration that would demand emergency intervention further along were anticipated. The fact that the mass occupied a significant intra-abdominal volume also posed a space conflict with the growing fetus, increasing the risk of preterm birth. After multidisciplinary discussion, surgical resection was decided. Even though the diagnosis of DTF was made afterwards, surgical resection would probably still be the management of choice considering NCCN consensus guidelines, since the woman was symptomatic and the mass increased the risk for the ongoing pregnancy.
Histological and immunohistochemistry examination allowed the diagnosis of DTF to be made. In our case, a mutation was detected in the CTNNB1 gene, supporting the diagnosis and excluding a syndromic condition (Gardner Syndrome) and the necessity for further condition related exams.
Surgery was performed early in the second trimester since it is considered the optimal time for elective surgery during pregnancy, avoiding the increased risk of spontaneous miscarriage of the first trimester and of preterm birth of the late-second and third trimesters8.
This case illustrates a very unusual location of a desmoid-type fibromatosis associated with pregnancy, itself a rare condition among soft tissue tumors and, the diagnostic and treatment challenges inherent to this condition.
Previous reports have documented the diagnosis and successful surgical management of DTFs during pregnancy, but to the best of the author’s knowledge, there are no reports of a tumor arising from the retroperitoneum managed antenatally.
Patient’s informed consent
The patient has given informed consent for the material to appear in a publication of the acta obstétrica e ginecológica portuguesa.
Author’s contribution
Marta Xavier has contributed substantially to the collection and analysis of data, writing of the manuscript and final approval of the version to be published.
Carla Ferreira, Antónia Furtado and Graça Ramalho have contributed substantially to the collection of data, critical review of the manuscript and final approval of the version to be published.














