Introduction
A mycotic aneurysm is dilation of an arterial wall due to infection. The term "mycotic" was coined by Willaim Osler in his Gulstonian lectures, where he described multiple aortic mycotic aneurysms in a patient with valve vegetations, which resembled the appearance of a fleshy fungus. It does not refer to fungal etiology, as the majority of infected aneurysms are caused by bacterial pathogens. Therefore, it has been suggested that the most appropriate term of these aneurysms is infectious. Infectious aortitis refers to vessel infection without aneurysmal dilation. An infectious aneurysm develops in the setting of an antecedent systemic infections with bacteremia or through the direct local invasion of the vessel wall (e.g., IV drug users) in a pre-existing aneurysm or atheromatous plaques.
The risks are higher in immune-compromised host i.e., HIV, diabetes, high dose glucocorticoids, or malignancy/chemotherapy. Commonly involved vessels include the femoral arteries, followed by the aorta, then the intracranial and visceral (e.g., superior mesenteric, splenic) arteries. Natural history is characterized by expansion, leading to pseudoaneurysm formation (contained rupture), rupture, or sepsis and subsequent multiorgan failure. Mycotic aneurysms are one of the most challenging clinical problems for the vascular surgeon due to the associated peri-operative mortality.1
Case Report
A 69-year-old male patient, with medical background of diabetes, hypertension and bladder carcinoma (ressected 5 years ago, complicated at the time with an E. coli septicaemia), presented at the ER with generalised malaise, asthenia, anorexia, abdominal pain, diarrhea and fever, with 1 week of evolution.
At clinical examination on admission, the patient presented with poor general condition, fever (T 39ºC), normotensive, and the abdominal examination showed no abnormalities.
Laboratory results showed an stable haemoglobin (Hb) of 13 g/dL, leukocytosis (19850/UI) and neutrophilia (90%), PCR 350mg/dL.
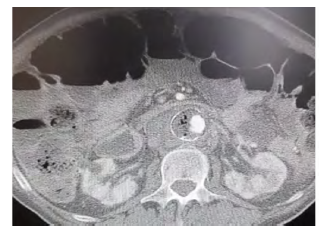
A Computed Tomography-Angiography (CTA) showed an 3,5 cm juxtarenal AAA, saccular, with peri and intra-aortic gas, strongly suggestive of a mycotic aneurysm (Figure 1).
Hospitalization was indicated and a septic and immunologic screening was perfomed. The patient was started on broad-spectrum antibiotic with meropenem and vancomycin. Clinical, hemodynamic and laboratory surveillance were iniciated.
Blood and urine cultures revealed E. Coli infection, and directed antibiotics were started.
After 10 days os hospitalization, the patient remained haemodinamic stable, and presented no fever or abdominal pain. However, inflammatory parameters remained elevated, so a second CTA was performed, revealing a daunting increase of 4 cm of the AAA (7,5 cm) with signs of contained ruture. (Figure 2)

Figure 2 Computed tomography angiography after 10 days of hospitalization, revealing growth and instability of the mycotic aneurysm
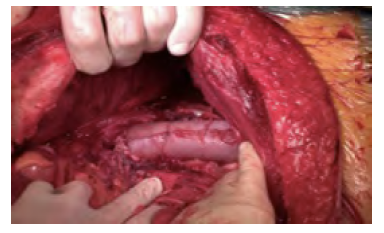
After discussion with the patient, an urgent intervention was decided and the team underwent a retroperitoneal aorto-aortic interposition requiring thoracophrenolaparotomy (Figure 3).
The aorta was reconstructed with a home-made tube using bovine pericardium (Figure 4). Operative cultures were obtained and were negative. After 24h of surgery, the patient unfortunately died of septic shock.
Discussion
The therapeutic management of mycotic aortic aneurysm is challenging.
The prognosis is generally poor, as the rapidly growing aneurysm has a high risk of rupture, and affected patients are often elderly with cardiovascular comorbities and concomitant infections or sepsis.2
Early diagnosis, immediate administration of systemic antibiotics, and timely surgical treatment is crucial to improve early outcomes. Despite lack of evidence, OSR is regarded as the gold standard for definitive treatment of MAA. OSR includes resection of the aneurysm, extensive local debridement, and revascularisation by extra-anatomical bypass or in situ reconstruction. Options for in situ conduits include autologous vein (either femoral or great saphenous vein, reconstructed to a neo-aorto-iliac system), cryopreserved arteries, bovine pericardium, or if unavailable prosthetic grafts (PTFE, Dacron or antibiotic soaked Dacron grafts) based on surgeon’s preference. Autologous or home-made grafts made of bovine pericardium are the most common choices. Operative cultures should be obtained.3
Recent studies with long-term follow up suggest that EVAR may have a short-term benefit over OR in selected cases, with no major late disadvantages. However, because of the rarity of mycotic aneurysms strong evidence on management is lacking, which makes firm recommendations difficult.3
In the present case, we opted for patient optimization before surgical correction of the AAA, which could be argued. Since the patient was frail and septic at admission, and no signs of rupture were present, initial antibiotic medical optimization was preferred. Despite this, and due to the excessive aneurysm growth with signs of contained rupture within a short period of time, repair with in-situ reconstruction was decided. The pre-existing septic condition of the patient is thought to be behind the fulminating multi-organ failure that occurred immediately after the operation, leading to refractary shock.
In conclusion, the authors present a case of mycotic aneurysm, initially managed conservatively and subsequently undergoing surgical repair due to excessive growth. The dismal outcome of this case exemplifies the complex nature of this pathology and the resulting difficutly in decision-making.
Acknowledgments: None
Conflicts of interest: None
Funding None