Introduction
Chronic obstructive pulmonary disease (COPD) is a common, multifactorial, progressive disorder that is characterized by airway obstruction and respiratory symptoms such as dyspnea and cough.1 According to the World Health Organization, it is currently the third leading cause of death, accounting for approximately 6% of total deaths worldwide. 2-4 Most cases can be linked to exposure to harmful airborne particles, such as outdoor pollutants or tobacco smoke. 5-6 Being a respiratory disease, COPD nonetheless represents an important risk factor for other chronic conditions. 7 Associated mortality and morbidity pose a significant social and economic burden across all countries, 4,8 with the severity of the disease relating directly to costs. It is estimated that, in 2015, COPD was responsible for 2.6% of global disability-adjusted life years lost. 4,8 In Portugal, around 14% of individuals over 40 years old have a diagnosis of COPD; according to data from the Primary Health Care System, 1.55% of the Portuguese population has this respiratory disease. Additionally, COPD is responsible for 2.5% of deaths in Portugal. 9
Though incurable, COPD is treatable and preventable. 5 According to current evidence, few interventions can positively impact long-term mortality, 10-11 but many more may improve quality of life by reducing symptoms and the frequency of exacerbations. 11-12 Pharmacological treatment can include inhaled drugs or supplemental oxygen. 5,11 Non-pharmacological treatment encompasses a wide variety of interventions, such as smoking cessation, patient education and self-management, psychological support, and pulmonary rehabilitation. 5,11
The importance and benefits of pulmonary rehabilitation in patients with a diagnosis of COPD have been widely documented. Several randomized controlled trials indicate clinically significant improvement in symptom severity, which in turn improves health-related quality of life. 13-15 Considering that personalized training is upheld as the gold standard of pulmonary rehabilitation, 16-17 it is difficult to define optimal treatment duration, location, and intensity. There is evidence of significant improvement in health-related quality of life for training regimens of at least eight weeks, but no clear evidence of optimal duration or frequency. 17-18 Hospital-based and community-based programs have been proven to be equally effective with equivalent training regimens. 19
When a solid network of community-based rehabilitation providers is available, especially where hospital-based programs possess specific and limiting referral criteria, primary healthcare providers may prefer to utilize local resources. Seeing as these tend to be more numerous than hospitals with the capacity for rehabilitation, they may ensure easier access and even treatment adherence.
Excluding a 2016 article with disparate comparators and an ample variety of included interventions, 20 no recent review has sought to assess the effectiveness of solely community-based pulmonary rehabilitation against standard treatment. Thus, this systematic review seeks to examine the best available evidence of the impact of pulmonary rehabilitation on the quality of life of patients with a diagnosis of COPD, specifically in a primary healthcare setting.
Our motivation to make this review lies within the global need to increase the body of scientific evidence that may influence policymakers’ decisions regarding investment in pulmonary rehabilitation. It serves, as well, as a way of stimulating further studies and projects on pulmonary rehabilitation, which constitutes a fundamental step towards our ultimate collective goal: the betterment of the quality of life of those who suffer from COPD.
Methods
The following databases were searched for randomized controlled trials published up to the 30th of September 2021: MEDLINE, CENTRAL, and Embase. We further searched the following grey literature sources: the European Respiratory Society and the American Thoracic Society.
Intervention
We included community-based pulmonary rehabilitation. This includes home-based rehabilitation plans, as well as supervised exercise and other consultations in outpatient units or gyms. We included only exercise programs considered to be aerobically demanding. Programs including strictly exercise were not included.
We excluded interventions in a hospital setting, as well as studies in which the intervention mainly involved educational programs, flyers, or remote (online, telerehabilitation) rehabilitation programs. We further excluded studies using isometric exercise or training programs that are not aerobically demanding, such as respiratory muscle training, simple breathing exercises, yoga, tai chi, or different types of traditional Chinese medicine.
Comparator
Standard care for COPD, excluding any pulmonary rehabilitation. This included pharmacological therapy.
Outcomes
The primary outcome was health-related quality of life (HRQoL) when compared to standard therapy for COPD, evaluated via validated, disease-specific questionnaires such as the Chronic Respiratory Disease Questionnaire (CRQ) or St. George’s Respiratory Questionnaire (SGRQ).
Secondary outcomes included long-term survival (mortality) and functional exercise capacity (FEC), evaluated via specific exercise capacity assessments such as the Six-Minute Walk Distance, the Incremental Shuttle Walk Test, and the Endurance Shuttle Walk Test.
We established that any unanticipated yet relevant outcome or measurement present in most of the selected studies would also be included.
Search strategy and data extraction
An initial limited search of MEDLINE, CENTRAL, and Embase was undertaken, followed by analysis of the text words contained in the title and abstract, and of the keywords and index terms used to describe the article. A definitive search using the aforementioned terms was then undertaken across all included databases. We included articles published up until the 30th of September 2021.
The search strategy consisted of terms about COPD, pulmonary rehabilitation, and primary health care. For MEDLINE and CENTRAL, we used the Medical Subject Headings (MeSH) in combination with other relevant filters. These search terms were adapted according to each database, depending on existing filters or specific nomenclature. The final search strategy can be found in Supplementary Material 1.
We included only randomized controlled trials that seek to validate the benefits of the intervention. The following types of studies were excluded: reviews, theoretical articles, qualitative studies, observational studies, case reports, protocols, and pre-experimental studies. We searched for studies in English, Portuguese, Spanish, and German. Any other language was excluded.
Titles and abstracts were manually retrieved following the results of our search strategy; article assessment and triage, including the detection and removal of duplicates, were conducted via the free Rayyan QCRI software. Those from additional sources were selected independently by two of the authors to identify studies that potentially met our inclusion criteria.
The full text was then analyzed according to our PICO question: for patients with a confirmed diagnosis of COPD (P), how does pulmonary rehabilitation in a community setting (I) compare to standard care (C) affect health-related quality of life, long-term survival and functional exercise capacity (O)?
A spreadsheet software was used to conduct data extraction and to further evaluate evidence quality and risk of bias. Data extraction was conducted independently by three of the authors, thus minimizing discrepancies. A fourth author intervened when the former could not decide on study inclusion. Relevant missing data was set to be requested from study authors, but unnecessary.
Besides high-level publication meta-data extracted data included the following dimensions: population (number of participants), base demographics and population characteristics, study methodology, intervention context (location, intervening parties), intervention methods and details (frequency, type of exercise), intervention duration in weeks, primary outcomes, secondary outcomes, and information for the assessment of risk of bias.
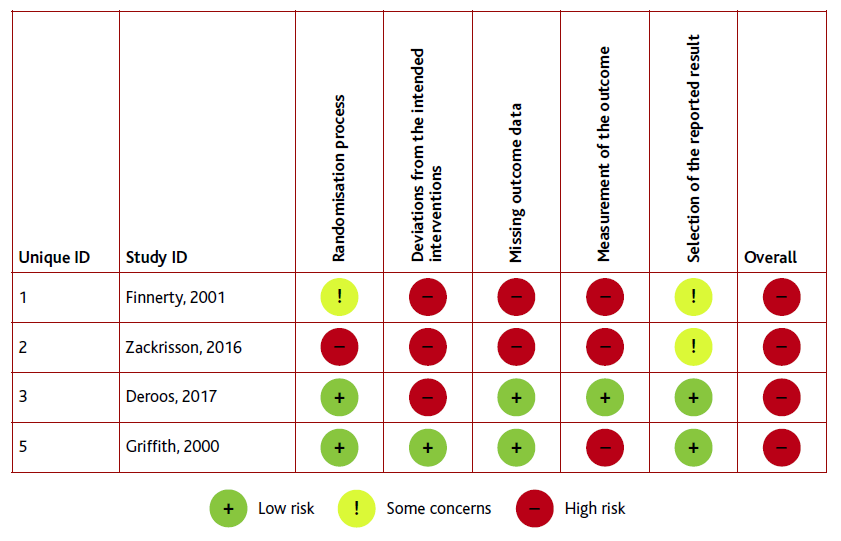
Two of the authors independently assessed the included studies for risk of bias, according to the following characteristics: randomization process; measurement of the outcome; deviations from intended interventions; selection of the reported result; and missing outcome data. Risk of bias was evaluated using the Cochrane Risk of Bias Tool, v. 2.0.
Results
Included studies
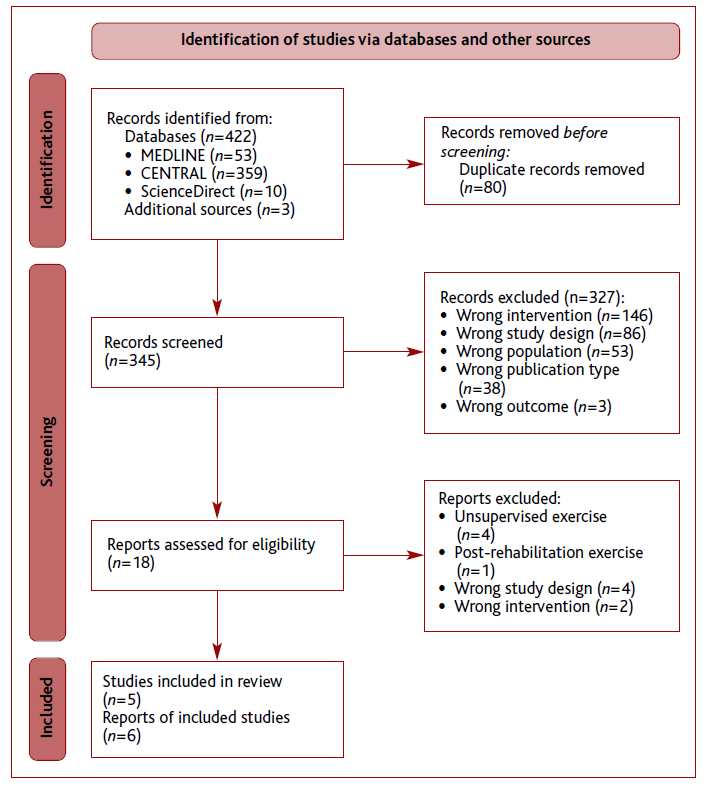
A total of 425 citations were retrieved by our searches. As detailed in Figure 1, 422 of these were obtained from databases. Only three were obtained from a grey literature source, namely the American Thoracic Society (ATS). European Respiratory Society (ERS) publications were dismissed due to search engine limitations, including the inability to export citations and thus systematically assess them. Duplicate removal excluded 80 articles, while title and abstract screening further excluded 327 articles. The reasons for exclusion are specified in Figure 1. The full-text review excluded 13 other articles, mostly due to wrong study design or wrong type of intervention, leaving five articles for analysis.
Two of the included articles referred to the same study (Zakrisson 2011 and 2016). The 2011 article describes the results of a one-year rehabilitation program, whereas the other provides a three-year follow-up. For clarity, these were analyzed together.
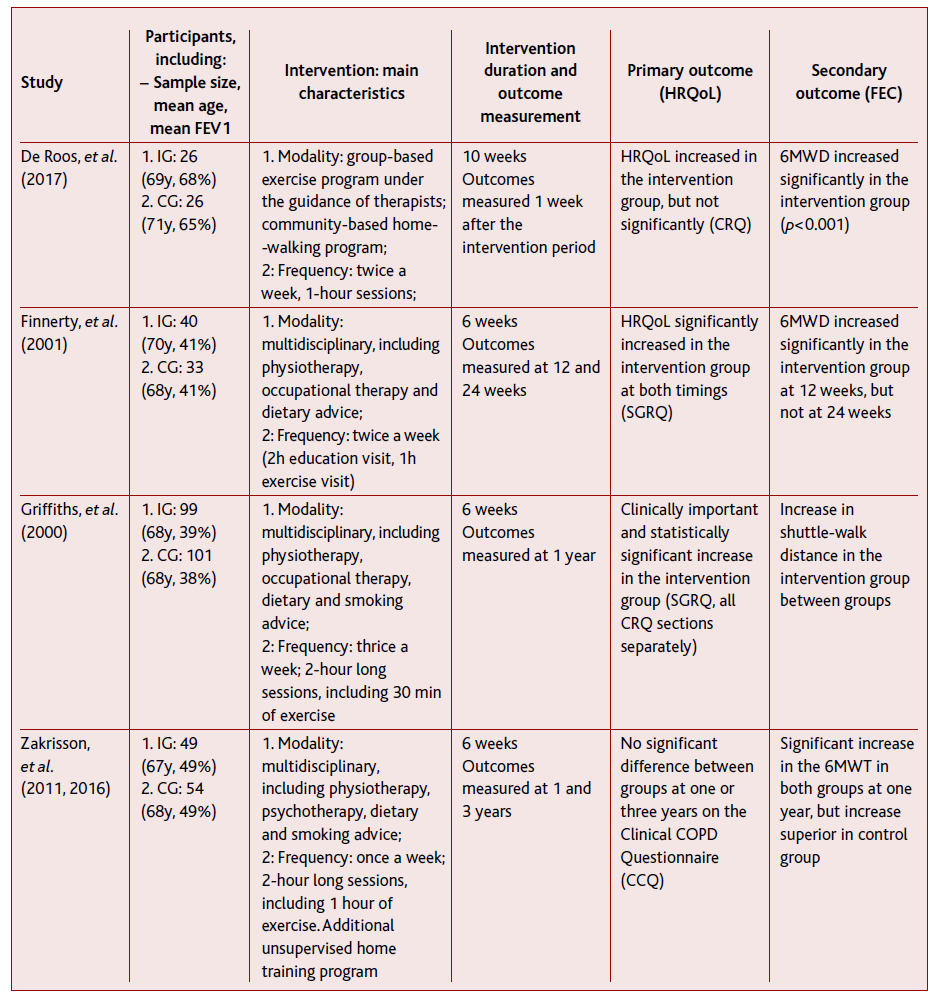
The included studies involved a total of 428 participants. Of these, 214 were allocated to a pulmonary rehabilitation program for a minimum of six weeks. All other participants were allocated to a control group under usual care; one study (Griffiths 2000) offered pulmonary rehabilitation to the control group after one year of follow-up. All studies suitably randomized their participants, save for one (Zakrisson 2011 and 2016), which, although classified as a randomized controlled trial by database search engines, picked intervention (IG) and control groups (CG) from separate pulmonary rehabilitation centers.
All studies’ participants were either previously diagnosed with COPD or diagnosed upon recruitment, with some variation in their baseline characteristics. In three of the studies, the participants’ FEV1 averaged at GOLD 3, while in a fourth (De Roos 2017) it averaged at GOLD 4. There were minimal differences in age and gender distribution between studies.
Study design
As described in Table 1, the study design varied greatly. There were differences in rehabilitation modality, session design, frequency, and duration. For instance, three of the studies used a multidisciplinary approach typical of pulmonary rehabilitation - including physiotherapy, psychotherapy, nutritional advice, and smoking cessation advice -, whereas a fourth (De Roos 2017) involved only physiotherapy sessions and a socially-oriented, unsupervised home training program. Session frequency and duration ranged from a single two-hour session (Zakrisson 2011 and 2016) to three two-hour sessions. Session content varied even between interventions of similar modalities.
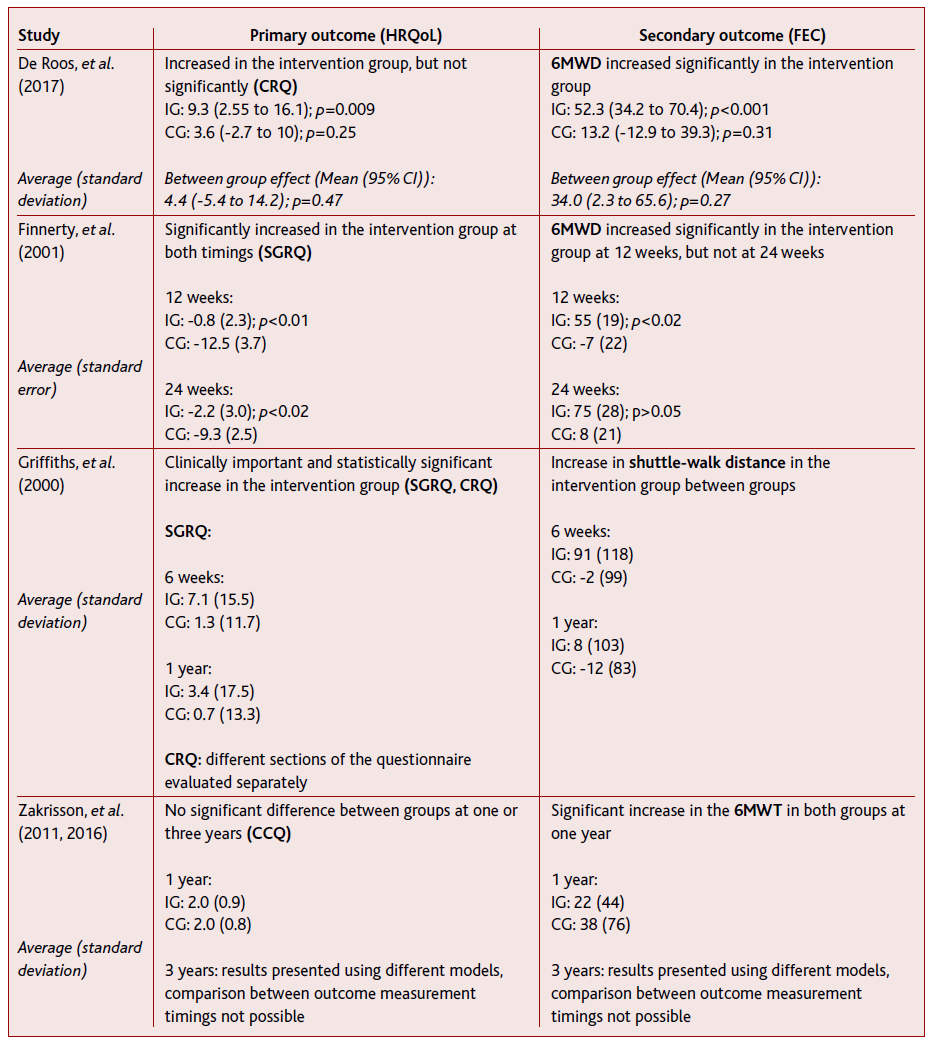
Outcome measurement methods, including scales, also varied between studies. Three different health-related quality-of-life scales were used across the four studies, whereas the preferred measurement of functional exercise capacity was the 6-minute walk distance (6MWD). Outcomes were measured at different timings, ranging from one week to three years after the experimental period. Outcomes are elaborated on Table 2 and further in the discussion.
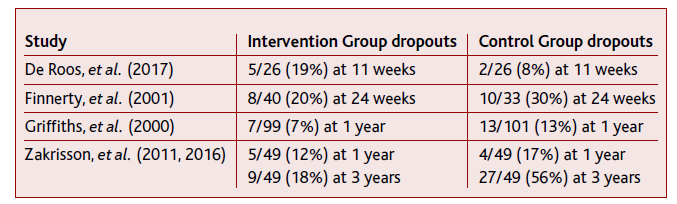
All outcomes were analyzed on an intention-to-treat basis, with dropouts being excluded. There were only slight differences in dropout rates, with intervention groups retaining more participants at follow-up (save for De Roos 2017) - see Table 3.
Risk of bias
As described in Figure 2, the overall risk of bias was high for the outcomes of all included studies, mainly due to limitations in blinding and outcome measurement.
Discussion
Of the four studies included in this review, three reported benefits in either health-related quality of life or functional exercise capacity, with only one (Griffiths 2000) demonstrating a statistically significant benefit in both its outcomes. A fourth study (Zakrisson 2011 and 2016) reported no difference between the two groups in any outcome save for exacerbations, which, although not relevant in the context of this review, was found to have decreased in the intervention group. It should be noted that this study by Zakrisson et al possesses important limitations, as discussed below.
Intervention structure, including session frequency and duration, was shown to have some impact on both outcomes. Griffiths et al report a significant increase in both quality of life and functional capacity at the one-year mark, and the intervention in question boasts both the highest weekly frequency and the highest weekly duration. Two other studies (Finnerty 2001, De Roos 2017) had biweekly sessions, and although their content varied between them; their results were overall favorable towards the intervention group/experimental hypothesis. The last study (Zakrisson 2011 and 2016) reports no differences between groups in quality of life or functional exercise capacity. The absence of benefit cannot, however, be attributed to a single factor. Besides including only, a single weekly session, the study measures its outcomes only at one and three years. This would perhaps suggest that intervention benefits are difficult to maintain over an extended period, although the data reported by Griffiths et al suggests otherwise.
As for the absence of benefit reported by Zakrisson et al, we wonder what the impact of study participation might have been. It’s possible that, in a disorder as complex and impactful as COPD, the act of regularly attending follow-up appointments or merely being reminded of their condition may have a positive effect on patient literacy and adherence; a prospective study published in 2015, for instance, demonstrated that greater continuity of care had a positive association with adherence for statins. 21
Long-term survival was excluded as an outcome due to the incompleteness of data and outcome measurement heterogeneity. In the two studies with complete data on participant mortality, however, the latter was higher in the control groups - four versus one death at the three-year mark (Zakrisson 2011) and twelve versus six deaths at the one-year mark (Griffiths 2000).
No unforeseen secondary outcome was included. Statistical analysis was deemed of limited relevance due to the small sample size, and thus not performed.
The included studies had several important limitations. The main limitation of trials involving complex interventions, such as pulmonary rehabilitation, is the inability to effectively blind them; both participants and caregivers are aware of their role and thus their group. Additionally, all studies evaluated outcomes on an intention-to-treat basis, thus excluding the weight of dropouts in both groups - no studies either suggest or prove that these had no difference in the outcomes.
As a side note, while marked by online databases as a randomized control trial, the study by Zakrisson et al was in reality quasi-experimental, since the participants were never subjected to randomization - instead, the two groups were drawn from separate rehabilitation clinics. We chose to include this study despite the aforementioned wrongful classification both because it did not change the conclusions of our review and because of its relevance in a research setting in which only a reduced number of studies was included.
The review itself was also subject to limitations, starting with study retrieval and selection. Although specific and adapted to our PICO, our search strategy was perhaps too restrictive; the use of the NOT boolean to preemptively exclude a few terms may have severely impacted the amount of included studies. A logical solution would be widening the search strategy’s scope, which would in turn lead to a lengthier triage, but possibly increase the number of included studies. Moreover, some of the review’s aims - secondary outcomes, subgroup analysis, statistical analysis - were designed with a greater number of studies in mind, and thus became difficult or outright impossible to achieve with an output of just five articles.
The exclusion of unsupervised interventions and telerehabilitation programs, although deliberate, was perhaps dismissive of their potential impact as explored by a 2021 Cochrane review. 22 This promising modality of pulmonary rehabilitation requires further investigation.
Differences in search engines further complicated achieving consistent results across all databases: as an example, ScienceDirect allowed only eight boolean connectors per field at the time of writing. Grey literature search engines were especially limited; the European Respiratory Society’s database did not allow for the exporting of citation lists, making article retrieval impractical and, in our time frame, impossible.
Conclusions
This review sought to assess the benefits of pulmonary rehabilitation in both quality of life and functional capacity of individuals with COPD, in the context of primary health care. Our findings are consistent with previous reviews and meta-analyses reporting beneficial effects of pulmonary rehabilitation in individuals with COPD; these had, however, explored the impact of mostly hospital-based interventions.
Although benefits to quality of life and functional capacity can be ascertained in pulmonary rehabilitation, optimal treatment modality, frequency, and duration are yet to be defined. Considering the complex nature of COPD and the myriad factors involved in its etiology, progression, and treatment, this may never be the case; perhaps an important part of pulmonary rehabilitation lies in customizing care to patient attributes, such as age, previous functional capacity, individual support network, among others.
Ultimately, though sound in its design, the present study does not deliver novel conclusions. In the future, we believe that larger-scale, controlled, and more methodologically robust trials may offer more meaningful evidence. This review may, however, help foster interest in pulmonary rehabilitation as a life-changing intervention in individuals with COPD and drive health policies in countries with a greater focus on primary health care.
Authors contribution
Conceptualization, GO; methodology, GO, RF, PR, LM, and CT; formal ana-lysis, GO, RF, and PR; investigation, GO, RF, and PR; resources, GO, and LM; data curation, GO; writing - original draft preparation, GO, RF, PR, and CT; writing - review and editing, GO, RF, PR, LM, and CT; visualization, GO, RF, and PR; supervision, GO.