Background
Persons suffering from chronic heart failure (P-CHF) experience a multiplicity of symptoms and signs with a significant impact on quality of life.1-3
This clinical syndrome is a public health problem affecting 37.7 million individuals worldwide with a 50%, five-year mortality rate and responsible for over one-third of all deaths from cardiovascular causes. 2-3
The Portuguese EPICA study revealed, a prevalence of 4.4% amongst adults older than 25 years, and 78% have at least two hospital admissions per year, leading to an annual cost of 2.6% of the total public health expenditure, its prevalence is expected to increase in the future. 4-5
CHF has been divided into three distinct phenotypes according to the measured left ventricular ejection fraction (LVEF), the one with reduced ejection fraction (P-CHFrEF) being more problematic. 6
Cardiac remodeling attenuation has been the treatment objective and a standard of care in CHF. 6-8 During the past 20 years, the benefits of angiotensin-converting enzyme inhibitors (ACEI), Antagonists of the angiotensin 2 type one receptors (ARB), together with the Renin-Angiotensin-Aldosterone System-acting drugs (RAAS-I) and beta-blockers (BB) on mortality, morbidity and hospitalization have been shown. 4 For the treatment of P-CHFrEF a set of four prognostic modifying medicines is recommended, a fifth one being necessary for symptom relief. 6
Novel medicine therapies targeting different pathways in the pathophysiology of CHFrEF, namely angiotensin receptor-neprilysin inhibitors (ARNI) and sodium-glucose cotransporter-2 inhibitors (SGLT2i), were introduced in the P-CHFrEF management. 6,9
The European Society of Cardiology (ESC), issued therapeutic recommendations in August 2021 whose use must be studied for the primary health care (PHC) setting. 6
The ESC Guidelines acknowledge four groups of prognostic modifying drugs, the RAAS along with ARNI, BB, mineralocorticoid antagonists (MRAs), and SGLT2i. 1,6
Under-treatment, clinical inertia, low adherence to guidelines by PHC physicians, and low drug compliance by patients are frequently associated with poor PCHF management outcomes. 10
More than half of PCHF are diagnosed in PHC centers and almost a third are treated exclusively by family doctors (FD). 8 Despite numerous reports on CHF in hospital settings, studies are scarce on how patients in PHC are being managed and treated. 11
Within the Portuguese National Health Service (NHS), PHC units can be named UCSP or USF according to structural and organizational setting. It is relevant to assess the accordance of current medicines therapy in P-CHFrEF with ESC’s most recent guidelines. 1
PCHF and P-CHFrEF can suffer from multimorbidity, hence patients giving it relative importance, compared to other simultaneous diseases, the same occurring with CHFrEF treatment in the resulting polypharmacy context. 12-13
This study aimed to evaluate the accordance between the 2021 August guidelines issued by the ESC for the treatment of P-CHFrEF, and the ongoing medicines prescription in PHC, in the central region of Portugal in December 2021. 6 And, also to know about mean age, median time since the diagnosis and last echocardiogram performance.
Methods
An observational cross-sectional randomized study in a population of 2,381 patients diagnosed with CHF (K77, ICPC-2), on the 31st December 2021, from eleven PHC units, according to the informatics office of the Portuguese NHS Central of Portugal Authority, was performed.
These eleven disseminated PHC units from the central region of Portugal NHS were the ones purposively invited in, after an Ethics Committee approval: UCSP Cantanhede, USF Mondego, UCSP Soure, USF Fernando Namora, USF Anadia, UCSP Campos do Liz, USF Rainha Santa Isabel, USF Figueiró dos Vinhos, USF Pombal, USF Esgueira and USF Grão Vasco, and accepted to participate.
Initial data from the PCHF units were obtained from the informatics office of the Portuguese NHS Central of Portugal Authority, issuing a list by the NHS number. This list was later transformed, in each PHC unit, into an inverted alphabetical order. PHC units assigned family medicine internees and specialists, to collect echocardiogram reports as well as the input date and date of the ICPC2 K77 registration input. The reports were studied in consensus by two of the research team members, according to the oldest registered systolic ejection fraction. A population of n=453 P-CHFrEF was retrieved, from which a size representative sample, 95% confidence interval, and 8% margin error, was calculated as n=133, which was proportionally distributed by each PHC Unit. Each health unit then used its file to gather its case information according to the number needed to study, dividing the number of P-CHFrEF to be studied per the number of P-CHFrEF on their inverted alphabetically ordered list.
In case of the non-existence of the above-detailed information, the next P-CHFrEF in the list was studied and if this one did not have the necessary data either, the one before would be searched. If neither of them was eligible, the next random one would be studied.
Per protocol, the sample size was calculated with [https://pt.surveymonkey.com/mp/sample-size-calculator/] for a confidence interval of 95% and an 8% margin of error.
PHC data were anonymously transmitted to the investigators. As inclusion criteria, P-CHFrEF should be followed up in family medicine appointments, documented from SClínico (Portuguese NHS official electronic registrations program), with a clinical appointment in the last semester. Medicines treatment was retrieved from the PEM® software (Portuguese electronic medicines prescription registry).
For each P-CHFrEF the following variables were recorded:
Age and gender.
Year of registration of the ICPC-2 K77 problem.
Years since the last echocardiogram.
Ongoing prognostic modifying therapy of CHFrEF: ACEI, ARB, ARNI, BB, MRA, SGLT2i. As in Portugal neprilysin antagonist, sacubitril is only prescribable in association with the ARB valsartan, for this study, those prescribed with ARNI were also considered as ARB prescribed.
Other drugs for CHF treatment: loop diuretic, digitalis, calcium channel blockers (CCBs).
Other prescribed medicines: non-steroidal anti-inflammatory drugs (NSAIDs), oral chronic cortico-therapy, thiazide diuretic and tricyclic antidepressants.
Data were studied using the Statistical Package for the Social Sciences (SPSS®), v. 24 for Windows®. Descriptive statistical methods were used with measures of central tendency for continuous variables.
Using the Kolmogorov-Smirnov test, the distribution of the numeric variables age, years with the diagnosis, and years since the last echocardiogram were tested. For nominal, ordinal, and numeric non-normal variables, non-parametric tests were used, p-value <0.05 being considered for significance. For normal distribution numerical variables, parametric tests were performed.
Results
From these 11 PHC Units, a universe of n=2381 PCHF and a population of n=453 P-CHFrEF was found. A size representative sample of P-CHFrEF, n=133 (5.6%), n=95 males (71.4%) was studied.
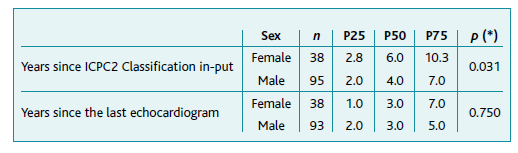
Mean age was of 74.3±11.6 years, males 73.4±11.0 and females 76.6±12.9, p=0.088. The median time since the diagnosis was 6.0 for males and 4.0 for females, p=0.031. Between genders years since ICPC2 Classification in-put were significantly different but years since the last echocardiogram were not, according to Table 1. For the n=87 P-CHFrEF aged ≤80 years, the median time since the last echocardiogram was 3.0 years, and for the n=46 older than 81 years it was 4.0 years (p=0.045).
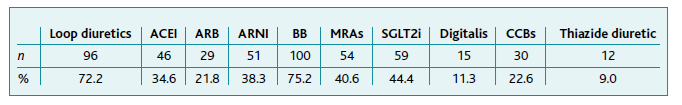
Table 2 presents the prescription rates of the different classes of drugs, the most frequent ones being BB (75.2%) and loop diuretics (72.2%). The third and fourth most prescribed classes were SGLT2i and MRAs, in 44.4% and 40.6%. The ARNI was prescribed in 38.3%. The ACEI and ARB isolated were prescribed in 34.6% and 21.8% respectively. For 94.7% there was a prescription of a RAAS-I (ACEI plus, ARB, plus ARB+ARNI). In four persons, a prescription of ACEI and ARB was found and in one case there was a prescription of ACEI and ARB/ARNI.
Table 3 presents the number of P-CHFrEF on a combination of three or more prognostic modifying medicines and less than three prognostic modifying therapies.
Table 3 Number of patients managed with three or more/less than three prognostic modifying medicines, by sex
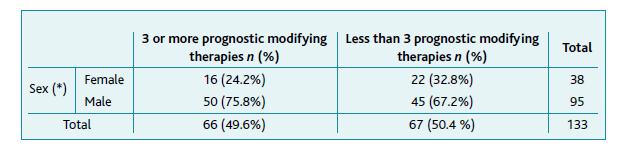
Note: (*) p=0.183, χ2
For n=66 (49.6%) three or more prognostic modifying drugs were prescribed. Although the ARNI incorporates an ARB (valsartan, in Portugal) in its pill presentation, in this study, we considered its use independent of the use of an ARB isolated, for statistical purposes.
For women, n=16 (42.8%) were treated with three or more classes of prognostic modifying drugs, and for men, n=50 (52.6%) were too, with p=0.183 between genders.
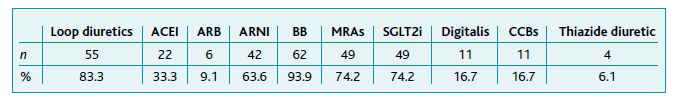
Table 4 presents the prescription rates for the different classes of drugs, in the subgroup treated with three or more prognostic modifying drugs. The most prescribed classes were the BB (93.9%), followed by the MRAs and the SGLT2i (both 74.2%). ARNI was prescribed in 63.6%. The second most prescribed class was loop diuretics (83.3%), which are prescribed for symptomatic treatment.
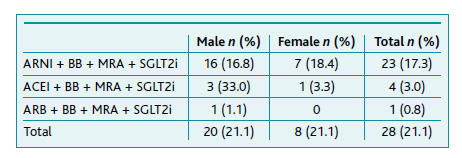
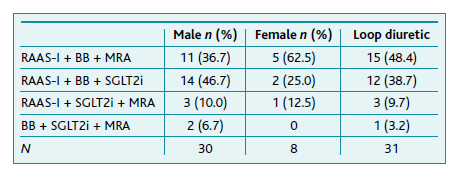
According to Table 5, n=28 patients (21.1%), 20 men and eight women, were on a quadruple combination regime. The most frequent quadruple modifying prognosis association was ARNI + BB + MRA + SGLT2i, in 23 patients (17.3%), n=19 (82.6%) of them simultaneously medicated with a loop diuretic.
Table 6 presents the results for triple combination regimes. For n=38 patients (28.6%), 30 men and eight women, a prognostic-modifying triple therapy regime was prescribed. Association of RAAS-I + BB + MRA was present in n=16 (42.1%), with the prescribed RAAS-I being an ARNI for n=9 (56.3%) and an ACEI for n=7 persons. For other n=16 (42.1%) patients the association of RAAS-I + BB + SGLT2i was present, again with n=9 (56.3%) being prescribed an ARNI. In this group, n=12 (75.0%) were also on a loop diuretic treatment. The triple cornerstone therapy (RAAS-I + BB + MRA), was prescribed for 44 patients (33.1%).
Double prognostic-modifying therapy was verified in n=47 (35.3%) P-CHFrEF, 34 men and 13 women. Out of these, n=33 (71.7%) were on a RAAS-I + BB. The second most frequent association was a RAAS-I + SGLT2i in n=9 (19.1%) patients (eight men and one woman). The combinations RAAS-I + MRA and BB + MRA were found in n=3 (6.4%) and n=2 (4.3%) patients, respectively. Also, out of these 47 patients, n=32 (68.1%) were simultaneously medicated with a loop diuretic.
For n=17 (12.7%) P-CHFrEF, 10 men and seven women, only one prognostic modifying medicine was prescribed. From these, n=12 (70.6%) were prescribed with a RAAS-I: n=5 with an ACEI, n=4 with ARNI, and n=3 with ARB. BB was the second most frequent class prescribed in monotherapy, with n=4 (23.5%) persons. Finally, n=1 (5.9%) P-CHFrEF was medicated with SGLT2i in monotherapy. From this group of P-CHFrEF under one prognostic modifying medicine, n=8 (47.1%) were simultaneously medicated with a loop diuretic.
For n=3 (2.2%) P-CHFrEF, no treatment with prognostic modifying drugs was found.
Digitalis was prescribed in n=15 (11.3%) P-CHFrEF, out of which n=11 (73.3%) were simultaneously medicated with the optimized P-CHFrEF therapy. The use of CCB was present in n=30 (22.6%) P-CHFrEF, with n=19 (63.3%) prescribed suboptimal P-CHFrEF therapy. In n=18 (13.5%) P-CHFrEF, an NSAID medicine was prescribed, n=9 (50.0%) simultaneously on three or more prognostic modifying drugs. In n=3 (2.3%) P-CHFrEF, corticosteroid therapy was prescribed, n=2 (66.7%) of them under suboptimal P-CHFrEF therapy.
Discussion
The main objective of this study was to analyze the management of the P-CHFrEF according to the ESC guidelines in PHC in a representative random study of patients from 11 invited PHC units in central Portugal.1
All P-CHFrEF should start medical therapy with the combination of all four groups of prognostic modifying medicines. 14-15 In a n=133 randomized, size representative sample, n=66 (49.6%) were being treated with three or more classes of prognostic modifying medicines, n=28 (21.1%) of them with the optimized medical quadruple therapy.
The ARB + BB combination, whether alone or associated with other therapies, was present in 93 patients (69.9%). This result is superior to other studies. 3-4,7-8,10 The individual prescription rates for these two classes stood out, as 91.0% were prescribed with an ARB and 75.2% with BB, contrasting with previous studies where lower prescription rates of ARB and BB were reported. 3-4,8,10 A possible explanation for the high use of ARB, as well as BB, might be that these classes were present in earlier recommendations for the treatment of CHF.
The triad of RAAS-I + BB + MRA is recommended as a cornerstone therapy for these patients and was prescribed for n=44 (33.1%) persons, from which n=28 (63.6%) were also treated with SGLT2i. 6
According to the ESC guidelines, the DAPA-HF study in 2019 and EMPEROR-reduced study in 2020, all patients undergoing this triple therapy, regardless of whether they are diabetic or not, should be considered for treatment with SGLT2i. 6,14,17
Despite the prescription rates of three or more prognostic modifying medicines classes in this study being 49.6%, thus higher than other previous studies, such findings indicate non-complete accordance with the current ESC guidelines. 3-4,7,10,13,18
Why P-CHFrEF is still under-treated, or on less adequate combinations, is a matter for future studies. An explanation might be that FD are ever more managing frail, multimorbid, polymedicated old patients. 12-13,15
Multimorbidity has been shown to have a significant impact on how recommended pharmacological therapies are prescribed by FD, as drug interactions and competing therapeutic requirements must be considered. 12-13,19
Many FDs can also be reluctant about starting new recommended medicines in the elderly for fear of intolerance, adverse drug reactions, or because of price concerns. 20-22 Clinical therapeutic inertia is a problem to be dealt with in P-CHFrEF. 1,12-13,15,17,22
Loop diuretics are symptomatic control medicines in P-CHFrEF. Therefore, less symptomatic patients could lead to clinical inertia regarding prognostic medicines, given the high prevalence of loop diuretics prescription. This was not verified in the present study, with 83.3% of the patients on three or more prognostic modifying medicines being simultaneously medicated with a loop diuretic, against 61.2% on less than three prognostic modifying medicines. 6
Results show an apparent non-inertia, as the prescription rates of SGLT2i (44.4%) and ARNI (38.3%) are higher than some previously ESC guidelines recommended medicines, namely drugs affecting the RAAS (55.1%) and MRAs (40.6%).1,12-13,15,17,22 Reasons for this are to be discovered, but these results favor a good continuous medical education and a well-designed medicine prescription in December 2021, with the 2021 ESC guidelines being released on August the 21st 2021. The reason for this prevalence level of SGLT2i prescription was not studied, but it may be due to associated diabetes or to heart failure specific indications. ARNI and SGLT2i were the latest additions to the CHFrEF prognostic modifying treatment regimen. SGLT2i prescription is higher than the prescription of ARNI, even though the SGLT2i approval is more recent. The proportion of prescription rates between the three different medicines in the RAAS-I group shows that ARNI, despite being the most recent addition and always in association with valsartan, is already more prescribed than ACEI and ARB isolated, in P-CHFrEF. This result is in line with other studies showing a rapid increase in ARNI utilization in real-world clinical data. 3,23
A significant limitation to the widespread adoption of the recommended therapeutic strategy can be the lack of any existing framework allowing PHC physicians to perceive the adequacy of the implemented treatment. 18 Currently, there is no implemented framework to describe the degree a patient’s medical regimen deviates from (or adheres to) the recommendations presented by the ESC guidelines or others.
To address these liabilities a simple informatics approach to PHC physicians could be a pop-up asking about whether:
PCHF was receiving each of the recommended prognostic modifying medicines;
PCHF was on target doses for each of these medicines;
PHCF had been tried on the medicines/optimal doses and these could not be tolerated, despite efforts at rechallenge or adjustment of other medications;
PCHF had been checked for literacy about CHF, medicine adherence, and pharmacokinetic or pharmacodynamics interactions. 24-25
This paper did not study if elderly or multimorbid or polymedicated P-CHFrEF were on lower rates of prognostic modifying medicines.
The presence of NSAIDs prescription in n=18 (13.5%) P-CHFrEF is somehow worrisome, representing sub-optimization of CHF therapy, revealing pain as a problem for P-CHRrEF.
Monitoring of P-CHFrEF should imply an annual echocardiogram for follow-up. There can be, however, a fraction of patients who clinically no longer benefit from carrying out this yearly surveillance. Time since the last echocardiogram was significantly different, older than 80 years P-CHFrEF within a longer mean time than younger ones. For this sample, the mean time is strikingly longer than recommended. 26-27
For PCHF, particularly P-CHFrEF, knowledge is crucial for adequate pharmacologic and non-pharmacologic treatment. So, consultation time and Person-Centered Medicine is an important issue to be considered and put into practice. 28-29
As strengths, this study, the first to our knowledge to acknowledge this matter in Portugal, perceived the rate of adequate prescription for P-CHFrEF and the high prescription rates of loop diuretics. The knowledge of P-CHFrEF prescribed with NSAIDs and the quality of medical e.registrations, with deficient exams patient’s follow-up, namely the echocardiogram. And also revealed, for the elapsed time since the release of the August 2021 CHF ESC Guidelines, the pattern accordant pharmacologic prescription. As weakness the type and amount of pathologies patients had diagnosed, nor its treatments, were studied. Also, the fact that it was made in purposive PHC units, although in a random sample in these 11 PHC Units. Another weakness was the lack of a quality of life (QoL) study, which was also not performed. Quality of life in P-CHFrEF should be studied so that their management can be up-graded. 30
Conclusion
Underutilization of the most recent evidenced-based medicine treatments to reduce morbidity and mortality in P-CHFrEF, particularly in the PHC setting, regarding the prescription of combination regimes according to recommended ESC guidelines was found for 49.6%, 17.3% being on a quadruple combination and 23.3% on a triple one. Longer than recommended intervals for echocardiogram monitoring were also found.
Authors contribution
Conceptualization, JV, LMS, and RG; methodology, JV, LMS, and RG; software, JV, LMS, and RG; validation, JV, LMS, and RG; formal analysis, JV, LMS, and RG; investigation, JV, LMS, BL, MF, LC, VF, SR, JFN, LF, LA, HB, JRM, and RG; resources, LMS, BL, MF, LC, VF, SR, JFN, LF, LA, HB, JRM, and RG; data curation, JV, LMS, and RG; writing - original draft preparation, JV, LMS, and RG; writing - review and editing, JV, LMS, BL, MF, LC, VF, SR, JFN, LF, LA, HB, JRM, and RG; visualization, JV, LMS, BL, MF, LC, VF, SR, JFN, LF, LA, HB, JRM, and RG; supervision, LMS, and RG; project administration, LMS, and RG.