Introduction
Chronic pain CP is defined as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”,1 which persists past the normal tissue healing time that is usually considered to be three months, in the absence of other factors. 2-3 It affects roughly 20% of adults worldwide and approximately 36.7% of Portuguese adults, being a major public health problem and an economic burden. 4-5 CP has direct and indirect costs such as the ones related to health expenses and work absenteeism, respectively. 6 Since CP affects both the physical and psychological condition of patients, 4,7 it can negatively impact virtually every aspect of everyday life, preventing patients from fulfilling their family and work responsibilities and hindering their social life. 4 Given the multiplicity of domains that can be affected by CP, treatment strategies should consider the social, biological, and psychological context of the patients besides the physical factors Figure 1. 2 Indeed, the treatment and management of CP generally include strategies to improve social and physical factors, minimizing disability and social isolation, besides providing pain relief. 8 In Portugal, a questionnaire directed to last year’s medical students and first-year residents, conducted by Cristóvão and Reis-Pina, showed that 82.1% of the interviewees did not assess pain as a routine in clinical practice because the patient did not always manifest pain. 9 Moreover, 81.7% were unaware of the existence of clinical guidelines and national legislation about CP. 9 Regarding pain assessment tools, whereas 82.9% knew that self-assessment scales existed, particularly the 0-10 numerical scale 35% and the visual analogue scale 21.9%, 70.9% were not aware of the existence of pain hetero-assessment scales. 9 This reinforces the need for dissemination of information on multidimensional pain assessment methodologies. Accordingly, 98.4% of the interviewees felt it would be important to have more education on the pathophysiology and management of CP, 9 a thought echoed by other physicians. 10-11 In this study, the best-known assessment tools were the ones that evaluate pain intensity using a numeric scale. However, it has been shown that CP patients have difficulty rating pain by a single score. 12-13 Additionally, one number cannot capture the complexity of pain, can be influenced by the perception of what the patient thinks would be beneficial, and may not reflect the functional status of the patient. 12-13
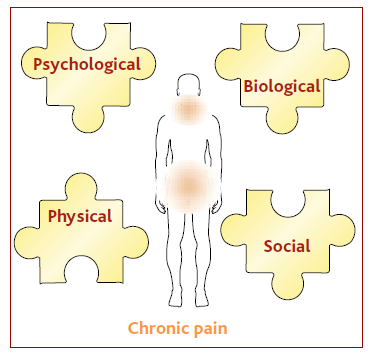
Figure 1 Factors that influence pain. Psychological, biological, social and physical factors influence how individuals perceive and report pain. 2 The most common sites of chronic pain are the neck/shoulder and lower back areas. 68
A recent study found that CP affects one-third of patients in Portuguese primary care units. 14 Consequently, a significant number of CP patients are followed by their family medicine doctor. The lack of knowledge about choric pain assessment is a barrier to effective treatment and management. Therefore, increasing the knowledge of pain assessment tools, which evaluate multiple domains of pain, will contribute to a better assessment and management of CP. Here, we describe five different pain assessment tools, considered particularly relevant by a group of Portuguese experts, including family medicine specialists. These tools assess the nature of pain and how this pain influences the functionality of CP patients. The successful implementation of such tools in clinical practice, particularly in primary care units, is expected to have a major impact on the management of CP patients.
Methods
This study involved four focus groups using a semi-structured approach. This is a qualitative method that allows to explore the perception and experience of different specialists, promoting the change of ideas and expertise about specific topics. 15 The expert panel that participated in the focus groups included 29 Portuguese physicians specialized in family medicine 26 specialists and orthopaedics three specialists from different regions of Portugal. The panel was divided into four working groups, according to the geographical area, and reflects the diversity of physicians within the different Portugal regions, including mainland Portugal and the autonomous region of Madeira. The panel included orthopaedic specialists with experience in managing CP patients and family medicine experts since most CP patients are followed by these medical specialities in primary care units. 14
The working groups met between September 2020 and March 2021 to discuss the main difficulties in assessing the different domains of CP. Particularly, tools to assess the functionality of patients and to understand how CP impacts their quality of life were debated. The debate was conducted by a moderator and assisted by two observers. The moderated conducted the meetings using a semi-structured guide and ensured the equal participation of all intervenient. The meetings were conducted in Portuguese. Given the lack of dissemination and awareness of the use of multidimensional pain assessment tools, the experts decided to perform a narrative review of the available tools that were deemed more useful and relevant in the clinical practice. The final text was agreed upon in June 2021.
Results
Qualitative Pain Assessment Tools
ACT-UP
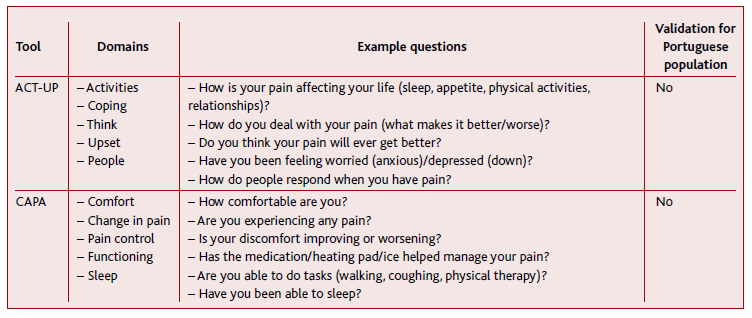
ACT-UP is an acronym for Activity, Coping, Think, Upset and People’s responses, developed by Turk et al, to guide healthcare workers in a brief screening interview of CP patients. 22-23 In this interview, the healthcare provider can observe the patient’s behaviour and identify behaviours that may influence pain self-report or areas that may require a more comprehensive evaluation. 22 The objectives are to assess 1 how pain is affecting everyday activities such as sleep, appetite and physical status Activity; 2 how the patient copes with pain, specifically what ameliorates or worsens pain Coping; 3 if the patient thinks the pain will get better Think; 4 if the patient has been feeling anxious and/or depressed Upset; and 5 how other people respond to the patient’s pain Table 1. 22-23 Although negative emotions caused by pain are normal and can even have a protective function, their persistence might be indicative of depression and other mood disorders. 24 Identification of these mood disorders and/or signs of symptom amplification related to psychological and/or social reasons will lead to a more adequate pain assessment and, consequently, increase the probability of good treatment adherence by the patient. 22,24 While no direct translation to Portuguese is possible, this acronym might function as a reminder to evaluate the behaviour of patients during the medical appointment.
Clinically Aligned Pain Assessment CAPA Tool
The Clinically Aligned Pain Assessment CAPA tool was created to replace the numeric rating scale, the default tool for pain assessment in a hospital setting. 12,25 The motivation came from the low satisfaction scores concerning pain management obtained by the University of Utah health hospitals and clinics. 12-13 The CAPA tool promotes a casual conversation between the patient and the healthcare professional to evaluate multifaced domains of pain. 13,25 The patient does not rate a scale nor chooses a previously defined alternative. 13 The tool provides healthcare professionals with the framework to conduct an interview which focuses on the 5 domains under evaluation and encoded wording to help with the documentation of the results. 12-13 The five domains include questions regarding comfort, change in pain, pain control, functioning, and sleep Table 1. 12 There is no script and the healthcare professional does not supply any pre-defined answers or ask the patient to rank or choose. 12-13
The CAPA tool recognizes that the experience of pain is more than just a number, and supports the engagement of patients and clinicians in a brief conversation about pain that leads to a coded evaluation. 12 Cultural relevant interpretations of pain are also better captured by CAPA since patients can discuss their pain freely. Another important feature is that CAPA can be applied to adult and paediatric patients who are participate in a basic conversation. 13 Therefore, CAPA offers a solution to one-dimensional pain intensity ratings and has proven reliable, responsive, and consistently improved patient and staff satisfaction. 26 However, as the CAPA tool does not have defined scoring rules, its reliability and validity have not been tested, and a better understanding of its quality in different populations is needed. 26 Although there is no official translation of this tool to Portuguese, healthcare professionals may adapt it as a template for discussing treatment progression with CP patients.
Quantitative Pain Assessment Tools
Barthel Index
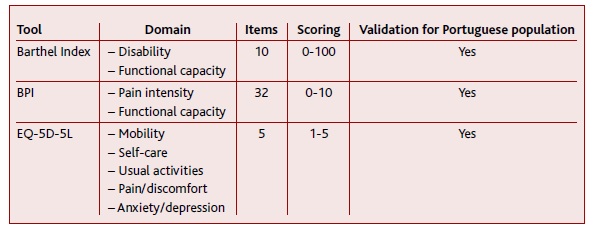
The Barthel index was initially developed to follow the improvement in mobility and self-care abilities during inpatient rehabilitation. 27-28 Nowadays, it is a well-known tool to assess functional capacity, i.e., the ability to perform everyday activities in an independent and autonomous manner. 29-30 Several adaptations of the Barthel index have been created. 28,31-32 The original index is one of the most used versions and comprises 10 items to evaluate if patients can perform activities such as going up and down stairs, feeding, and grooming in an independent manner. 27 Index scores range from 0 completely dependent to 100 completely independent and can be calculated from medical record information, by direct observation, or by interview of the patient or of the patient-caregiver Table 2. 27,33 Additionally, it can be self-administered. 34 The Barthel index has been validated for the Portuguese geriatric population and is available in the information system of the Portuguese National Health Service. 35 It is commonly used to assess the progress of rehabilitation of neurological disorders and the functional status of older adults and of stroke patients. 36-38 Although it is not specific for CP, its simplicity and easy access make it a valuable tool for a fast assessment of how pain interferes with the daily activities of patients.
Brief Pain Inventory BPI
The brief pain inventory BPI was initially developed to rate cancer-related pain. 39 However, since then, studies have confirmed the validity of using this questionnaire to assess pain from other aetiologies, 40-43 including non-malignant CP. 44 This questionnaire has been translated and validated in different languages including Portuguese, 45 and was recommended by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials IMMPACT as an outcome measurement of functional impairment in all CP clinical trials. 46 BPI is a self-reported measurement that evaluates both pain severity and its interference with normal life. 47 Two versions of BPI were developed: the long form and the short version. The first was found to be too extensive for repeated use in clinical monitoring and for research purposes. 47 The shorter version, besides the difference in extension, considers 24 hours of recall period, instead of the one week considered in the long form, 47 and is the one recommended for standard use in clinical and research contexts. 47-48 It includes a question that enquires if the patient had unusual pain, front, and back body diagrams to indicate pain location, four pain severity items that evaluate pain intensity at its ‘worst’, ‘least’, ‘average’ and ‘now’, and seven items to evaluate pain interference with ‘general activity’, ‘mood’, ‘walking ability’, ‘normal work’ including housework, ‘relations with other people’, ‘sleep’ and ‘enjoyment of life’. 47-49 Additionally, it has two questions to describe the pain treatment received and to assess the relief provided by that treatment. 47 Pain intensity, interference, and relief are rated using 0-10 scales Table 2. 49 From this questionnaire two scores can be obtained: one for pain intensity and the other for pain interference. 47,49 All intensity and interference items have the same weight in the final score and, therefore, the scores can reach a maximum of 40 or 70, respectively. 49 The other components of the questionnaire provide useful information for the physicians but are not taken into account for the calculation of the scores. 47,49
EuroQol 5 Dimensions EQ-5D
The EuroQol 5 Dimensions EQ-5D was developed with the aim of having a “standardized non-disease-specific instrument for describing and valuing health-related quality of life”, so that studies pertaining to different countries could be compared. 50 It was intended as a measurement tool that would complement the existent assessment questionnaires while still allowing cross-national comparison of reference data. 51 The EQ-5D has been applied to various illnesses and treatments, 52-54 and was suggested as one of the most appropriate tools for assessing patient functionality in CP. 55 This tool was translated to Portuguese in 1997 at the Centro de Estudos e Investigação em Saúde from Coimbra University and was afterwards validated for the Portuguese population. 51 Moreover, specific scoring functions for the Portuguese reality were defined. 56-57 The EQ-5D is a self-report questionnaire that assesses five domains of health: ‘mobility’, ‘self-care’, ‘usual activities’, ‘pain/discomfort’ and ‘anxiety/depression’ Table 2. 50,58 These five domains comprise three levels of impairment severity, in which level 1 corresponds to «no problems», level 2 to «some» problems and level 3 to «extreme» problems. 50,58 The health status of patients is given by the levels on each of the five domains. 51 The different combinations can originate 243 health states, to which ‘dead’ and ‘unconscious’ were also added totalling 245 health states. 58 Additionally, there is the possibility of having a score that reflects specific settings by employing country-specific scoring functions. 51,55 EQ-5D also includes a visual analogue scale where 0 corresponds to the ‘worst imaginable health state’ and 100 to the ‘best imaginable health state’, and the patient is asked to localize their health state in this scale. 58 Both the quantitative and the descriptive aspects of the questionnaire are used by healthcare providers to assess the impact of CP in the health status of patients. 51 In 2009, the EuroQol group developed a new version of this questionnaire to improve sensitivity and to decrease ceiling effects. 59 To achieve this goal, two more levels of impairment severity were added to each of the five domains of health being assessed: in addition to «no problems», «some» and «extreme», «slight» and «severe problems» were also included Table 2. 59 To distinguish between the two versions, the newly developed questionnaire was named EQ-5D-5L due to the five levels of response and the original tool was renamed EQ-5D-3L. 59 EQ-5D-5L has also been validated for the Portuguese population and country-specific norms were calculated. 60-61
Discussion
The effective management of CP patients can only be achieved after assessment of pain aetiology, patients’ specific phycological and behavioural presentation, and symptoms interpretation. 22 To achieve that, a multimodal comprehensive approach that combines information regarding patient history, physical examination, clinical interview, and standardized assessment tools should be integrated. 62 Different individuals will have distinct interests and priorities that will dictate which of the areas affected by CP will cause more inconvenience. Additionally, CP patients’ recognition that factors such as mood, fatigue, and potential judgment from healthcare providers influence pain assessment, reiterate the need for pain assessment that goes beyond a simple number. 63 Unidimensional self-reported tools provide a single, general rating that does not consider the different individual characteristics, nor contextual detail of pain, such as the localization, circumstances, characteristics, and the time and frame of pain to be assessed. In addition, the impact of CP on patients’ physical capabilities and quality of life are important features to be addressed. 22 Therefore, multidimensional pain assessment tools, that evaluate the impact of CP in different aspects of patients’ lives, such as those described in this work, are important instruments in the clinical practice that impact patient management Figure 2.
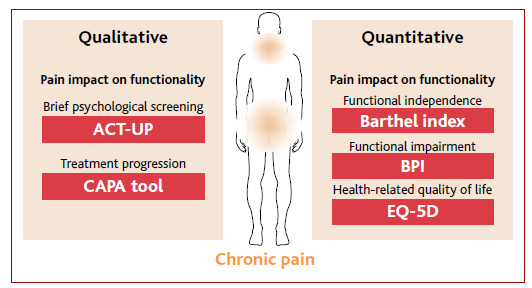
Figure 2 Factors that influence pain. Psychological, biological, social and physical factors influence how individuals perceive and report pain. 2 The most common sites of chronic pain are the neck/shoulder and lower back areas. 68
The qualitative nature of the ACT-UP and CAPA might render the comparison of pain characteristics more challenging. Still, they are valuable tools to guide physicians through interviews and to perform qualitative assessments. Some healthcare providers have reported some difficulties in understanding how to use CAPA: some were inclined to read the potential encoded evaluations to the patient and others stated that they did not feel skilled enough to have conversations about pain with patients. 12 Thus, specific training, which includes role modelling and examples, might be beneficial for the application of CAPA. 12
The Barthel index is a useful tool to measure how CP impacts the functional independence of patients. By being available in the information system of the Portuguese National Health Service it is a very accessible tool and has been considered simple and easy to use. 64 When it is self-administered, it will have the self-report bias common to most of the discussed tools. When it is administered by a healthcare provider, it is assumed that the disabled patient is performing at their usual level of functioning and that the healthcare provider is trained in using the scale and has access to the scoring guidelines. 64 Thus, deviations to these conditions might influence the score. 64
BPI provides a complete assessment: of pain localization, intensity, and relief, together with the evaluation of how this pain affects everyday life and the relation-ships of patients. It is easy to score, has good clinometric properties, and can be administered verbally to patients with reading and/or writing difficulties. 47,49 Nevertheless, it is more extensive than other tools and its use can be time-consuming during a consultation. One way to circumvent this disadvantage could be to ask patients to fill out this questionnaire before the consultation, either on their own or with the help of a healthcare provider.
The EQ-5D is simple and quick to fill and specific population weights can be used. 55 However, given it is a generic tool for health status assessment, the questions might not be as specific for CP as in other questionnaires and thus, it can be less sensitive and have a lower discriminatory ability. 65 Additionally, the visual analogue scale might be interpreted differently by distinct patients as some patients find the concept too abstract/hard to comprehend. 66 Nevertheless, the EQ-5D has shown good construct validity and responsiveness for the evaluation of CP patients, being a valuable tool to assess the impact of CP on the overall quality of life of patients. 55
Primary care providers are frequently the first health professionals that identify and manage CP patients. However, CP is challenging and can be time-consuming, and many primary care clinicians have difficulties with CP management to regular appointments due to, for example, a lack of guidelines. 67 Additionally, factors such as time constraints of medical appointments, the population’s level of literacy, and lack of familiarity with functional assessment tools, might hinder CP assessment. Asking for help from other healthcare professionals, to assist patients fill the questionnaires before the medical consultations, could prevent consultations’ overextension. Additionally, strategies for information dissemination, such as this publication, can help to increase awareness of the functionality assessment of CP patients. Of all the tools discussed and presented in this work, EQ-5D appears to be the most advantageous. Although is not a specific pain questionnaire, it allows the assessment of multiple quality-of-life variables, including pain assessment. Filling is easy and fast, it has clear scoring rules, and environment-specific scoring functions can be applied. 55-57 Moreover, it has been previously used with good results to assess the quality of life of CP patients, has been validated for the Portuguese population and specific norms for Portugal have been calculated. 55,60-61
Nevertheless, if employing one of these pain assessment scales is not possible, at a minimum, an open conversation with the patient and/or caregivers must occur. This conversation will allow the assessment of the impact of CP in the patients’ lives, namely in the quality of sleep, mental health, everyday activities, and overall functional independence. Moreover, this conversation can help adjust the patients’ expectations and consequently, increase their treatment compliance.
Conclusions
The various pain assessment tools described in this work consider the multidimensional nature of pain, albeit with different specific foci. By highlighting these tools, we hope to increase the knowledge and awareness regarding CP assessment, a complex process due to its inherent subjectivity and the multitude of factors that influence pain. Specifically, we wanted to increase the visibility of tools that measure the functionality of patients and promote a more open conversation between physician and patient, allowing for a tailored treatment strategy. Ultimately, the use of tools that measure more than one domain of pain or the combination of multiple tools, can lead to the improvement of CP management and the decrease of the emotional and economic burden associated with CP.