Introduction
Polyorchidism, also named as supernumerary testicles, is a very rare developmental anomaly, defined by the presence of more than two testicles. Since it was first described by Ahlfeld,1 only about 200 cases have been reported in the literature.2 Due to the rarity of this condition and scarcity of systematic reviews, the management of polyorchidism is still controversial.
We report a case of a 6-year-old patient with polyorchidism that presented as a painless scrotal swelling. Herein we also provide a revision of the literature, particularly the classification system and management approaches.
Case Presentation
A 6-year-old boy, presented with asymptomatic left scrotal swelling. He had a history of right orchidopexy in infancy, due to cryptorchidism, and lacked previous evidence of pathology on the opposite side. Physical examination revealed a left communicant hydrocele.
Scrotal ultrasound (US) was performed and confirmed a mild volume left communicant hydrocele. Moreover, also on the left side, US depicted a superiorly positioned smaller supernumerary testis (volume of 0,16 cc) compared to the inferiorly positioned testis (volume of 0,32 cc) (Fig.1). An apparent communication of the two testes with a common epididymis was suggested. Diffuse bilateral testicular microlithiasis was also found, including the supernumerary one. Besides this, US evaluation of the right scrotum was unremarkable, with a normal sized testis for the age group (volume of 0,52 cc).
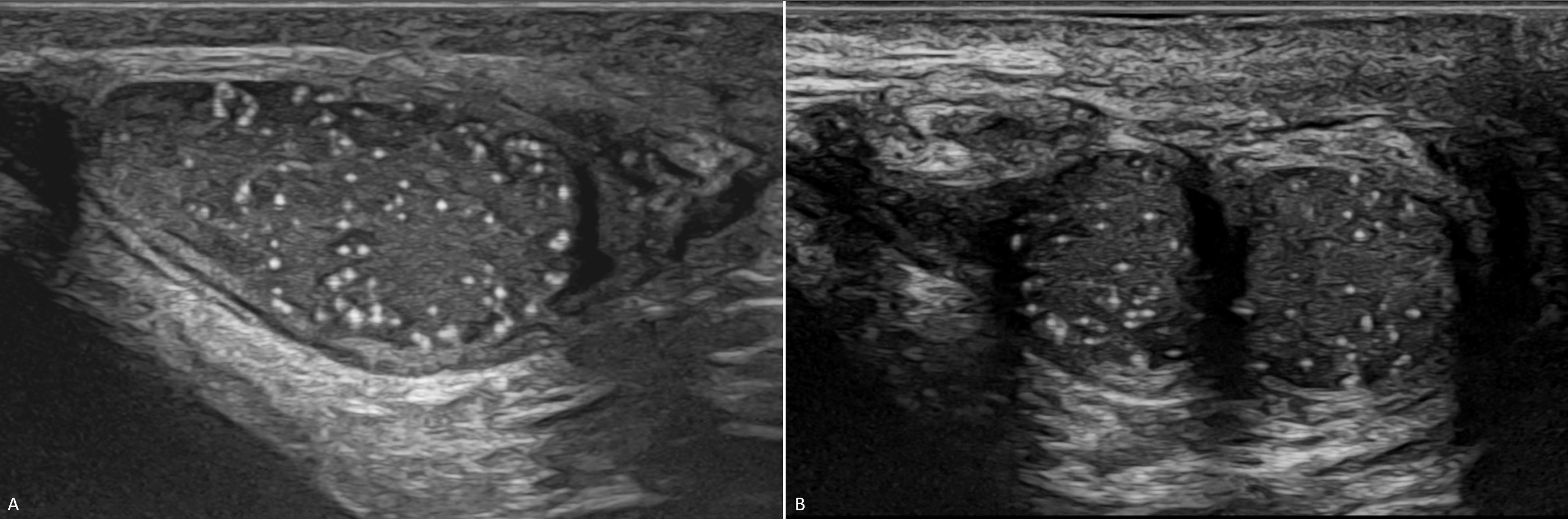
Figure 1: Diffuse bilateral microlithiasis. A- Longitudinal ultrasound image of the right scrotum depicts a normal sized testis for the age group. B- Longitudinal ultrasound image of the left scrotum depicts two testes with smaller volume compared to the contralateral.
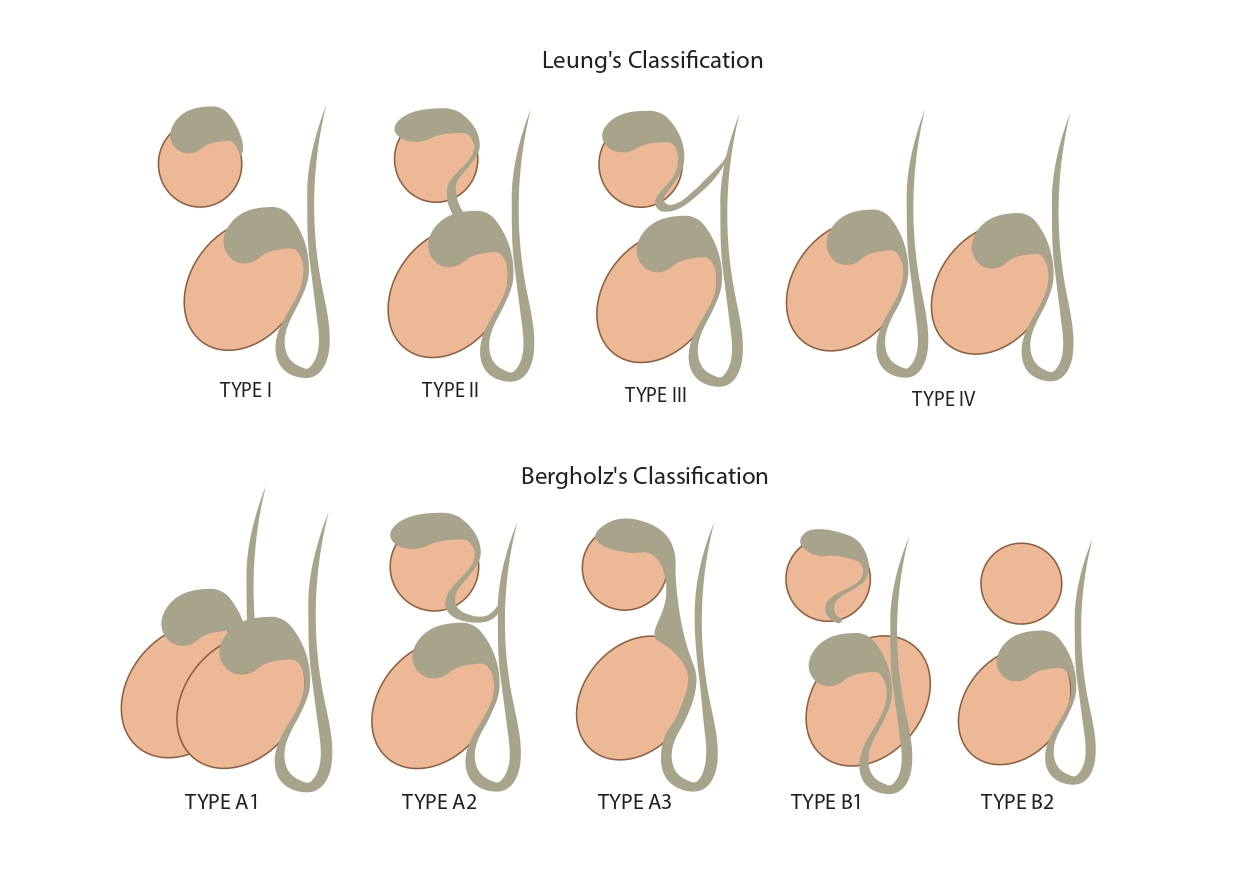
Considering the presence of hydrocele and the need for further diagnostic clarification, surgical exploration was proposed. A left inguinal exploration was accomplished and after ligation of the patent processus vaginalis, the scrotal content was eviscerated through the surgical incision for evaluation. The diagnosis of triorchidism was confirmed: two testicular masses sharing the same epididymis and vas deferens (Fig. 2), consistent with type II of Leung’s classification3 and type A3 of Bergholz’s classification (Fig.3).4

Figure 2: Intraoperative photograph showing scrotal content delivered through the inguinal incision: two testes (asterisks) connected to the same epididymis (arrowhead) and draining into a common vas deferens.
Since these testicular units shared the same drainage into the vas deferens, preservation of both was decided. The testicular units had a wandering relation, meaning that they moved freely along the epididymis axis. With this in mind, and considering the risk of torsion, an absorbable suture was undertaken between them.
The patient was discharged the same day of surgery and postoperative recovery was uneventful. After 12 months of follow-up the patient remained asymptomatic and no other findings on physical examination were noticed.
Discussion
Polyorchidism, defined by the presence of more than two testicles, either intra- or extra-scrotal, is a rare condition with only around 200 cases described in literature.2 Its etiology is associated with an accidental division of the genital ridge,5 and its diagnosis is often incidental. Patients frequently present with complaints not related to this condition itself but elicited by other associated conditions. A meta-analysis from Bergholz et al. showed that only 16% of patients presented with an asymptomatic scrotal mass, with the remaining presenting with other inguino-scrotal associated conditions.4 Several clinical features related to this condition have been previously highlighted, such as left side affectation and scrotal position of the supernumerary testis in most cases.4 Most of these features were present in the case that we reported, with the exception of the age at which most of the patients described in literature were diagnosed, usually older than our case. Mal-descent, inguinal hernia, torsion, hydrocele and malignancy are frequently reported and commonly the source of symptoms.4,6
Polyorchidism’ classification is not consensual in literature. Leung, Singer and Bergholz have presented different types of classification, one more focused on embryological features and others emphasizing anatomical findings and functional potential.3,4,7According to Leung, polyorchidism type II (supernumerary testis draining into epididymis of usual testis, sharing a common vas) is the commonest, and in conjunction with type III (supernumerary testis with its own epididymis draining in a shared vas) account for 90% of cases.3,6 Bergholz has proposed a different classification, with emphasis on the practical and functional aspect of this condition, dividing cases in those with some drainage (type A) and those with none (type B), being therefore non-contributive to reproductive function.4 Our case represents a type II of Leung’s classification and A3 of Bergholz’s classification, the commonest form of this condition.
Physical examination might be helpful in raising suspicion, but the diagnosis should not rely only on it. There are many differential diagnoses of scrotal mass that cannot be accurately excluded with clinical examination alone. Histological analysis was believed to be needed by some authors to confirm diagnosis.3,4 However, recently, ultrasound and magnetic resonance have been used for the diagnosis with high accuracy, and in some cases without further need of surgical exploration or biopsy for confirmation.8,9 With the case presented, we showed that ultrasound can depict findings related to polyorchidism even when there is no clinical suspicion and may go even further, disclosing the type of polyorchidism.
Histological analysis might be helpful in describing spermatogenesis quality and excluding associated malignancy. According to Bergholz et al. near 37% of polyorchidic patients were found to have decreased or absent spermatogenesis and 51% of these supernumerary testes were maldescended.4 The frequency of malignancy in supernumerary testis compiled in this meta-analysis was 6.4% and most cases represented maldescended testis.2 In the case we presented, no histological analysis was undertaken, since preservation of the testicular units was decided, as there was no significant variation between testicular units’ volume. Besides, both testicular units were in scrotal position, which represents a lower risk for spermatogenesis impairment and neoplasm development.
Historically, supernumerary testis resection was common, regardless of the type or location due to torsion and malignancy concerns.4 However, a normal spermatogenesis was described in about 50-63% of the supernumerary testes4,10, as the most common types of polyorchidism are those drained by some structure, either shared or not. Since the absence of contribution of these supernumerary testes to reproductive function cannot be excluded, preservation is recommended in most cases nowadays. Many have proposed a conservative management in cases of scrotal polyorchidism, in the absence of other abnormalities and without suspicion of malignancy, reserving resection for non-drained types (type I of Leung or type B of Bergholz), for maldescended testes, for those associated with other abnormalities, complicated by torsion or with malignant suspicion.4,6,11,12 There are also some reports of supernumerary testes managed conservatively, without surgical exploration, only surveilled by imaging.8,9,10 In our case, surgical exploration was offered according to the associated diagnosis of hydrocele. Since torsion of supernumerary testis is the most common related complication,4 pexy of both testicular units was decided in order to prevent the occurrence of such complication.
According to the associated risk of malignancy in polyorchidism, annual follow-up with ultrasound is recommended by some authors.9 Resection of supernumerary testis should be offered when there are suspected features of malignancy at diagnosis or any change in echogenicity, shape or focal mass appearance on follow-up ultrasound.4,10
Regarding microlithiasis, Yesil et al. recommend annual follow-up US of at-risk patients when risk factors other than microlithiasis are present,2,13 therefore we set our patient for this follow-up strategy for the combination of the two conditions.
Conclusion
Polyorchidism is a rare condition with a non-consensual management. Ultrasound plays an important role in the diagnosis and surveillance of these patients at a higher risk for malignancy and may preclude the need of surgical exploration or even resection, reserving these attitudes for selected cases. As previously proposed by others, for drained types of polyorchidism, without other anatomical abnormalities, in scrotal position and without suspicion of malignancy, we advocate conservative management and US follow-up once a year.