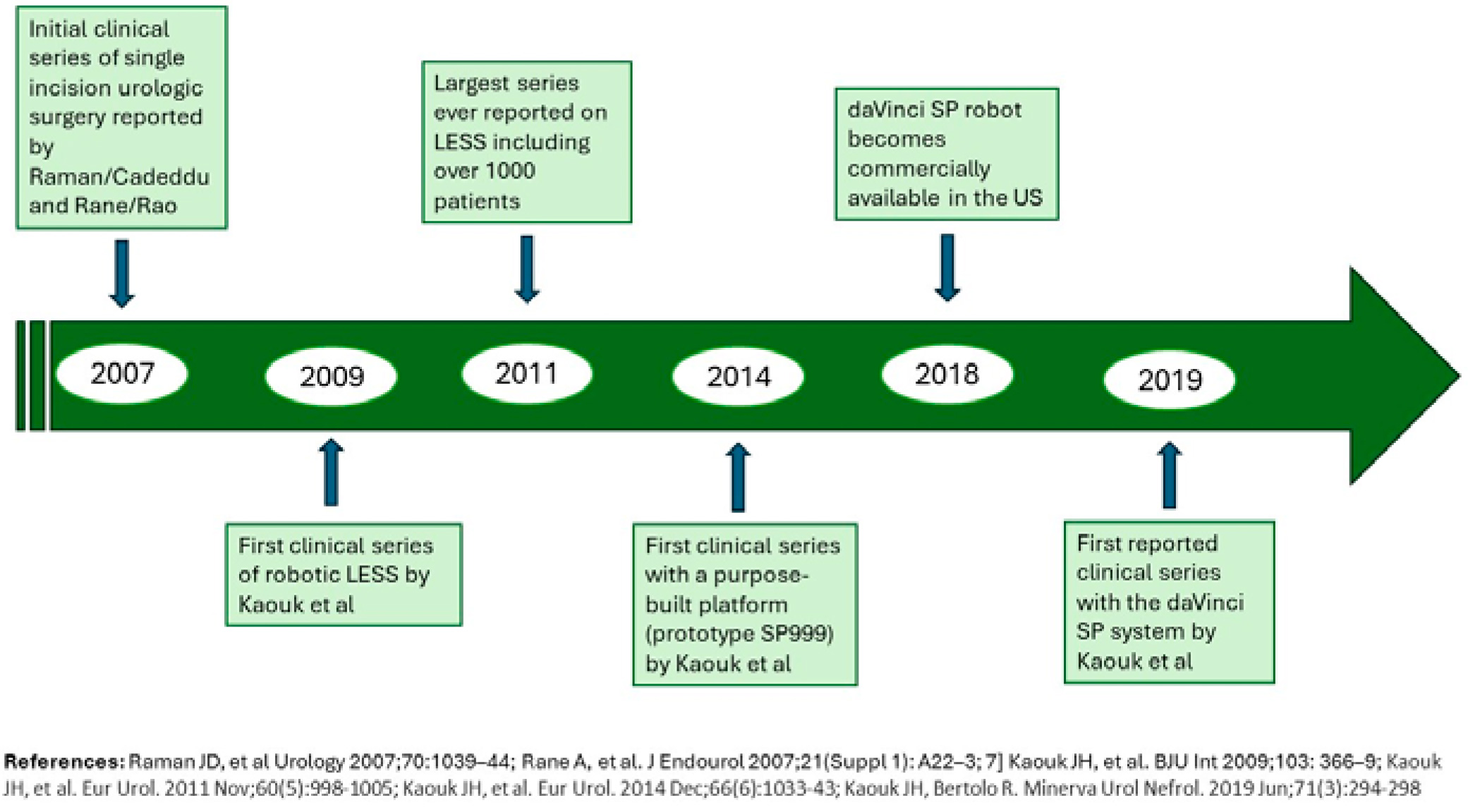
A historical perspective
The idea of performing a surgical procedure through a single abdominal incision date back to approximately 20 years ago1 (Fig. 1). The rationale behind it was that minimization of skin may benefit patients in terms of port-related complications, recovery time, pain, and cosmesis. Thus, there was a lot of enthusiasm around the concept of “laparoendoscopic single site surgery” (LESS), and many surgeons around the world rode a wave of clinical investigations aiming at exploring the potential application of this novel surgical concept for a large variety of urologic indications.2 Those pioneers soon realized that LESS was plagued by significant technical challenges which would hinder its wide implementation.
Therefore, the use of the commercially available multiport robotic platforms was explored to overcome these challenges.3 Ultimately, the need for a purpose-built robotic system was deemed crucial for the renaissance of single-incision/single-port surgery.4
In 2014, Kaouk et al reported the first clinical investigation on the use of a novel robotic platform specifically designed for single-port urologic surgery (da Vinci prototype SP9999).5 A total of 19 procedures were successfully performed including radical prostatectomy, radical, simple and partial nephrectomy. This feasibility and safety study paved the way for the FDA clearance of the daVinci SP robotic system. However, the system became commercially available in the US a few years later, in 2018, but only for Urology and Transoral surgery.
Kaouk et al reported the first clinical series using the new platform.6
In 2022, the system was cleared for use in Japan. As of December of 2023, 177 SP systems have been installed in the US.7 In January 2024, the SP system received CE clearance and it is now available also in Europe.
Overview of the sp system and accessories
A familiarity with the SP robotic system and its main features, as well as accessories that are used with it, is essential to understand its functionality and potential.8
The da Vinci SP (Intuitive Surgical, Sunnyvale, CA, USA) integrates upgraded software, which improves its overall functionality, offering features that optimize surgical procedures and ensure seamless integration with the platform and instruments.
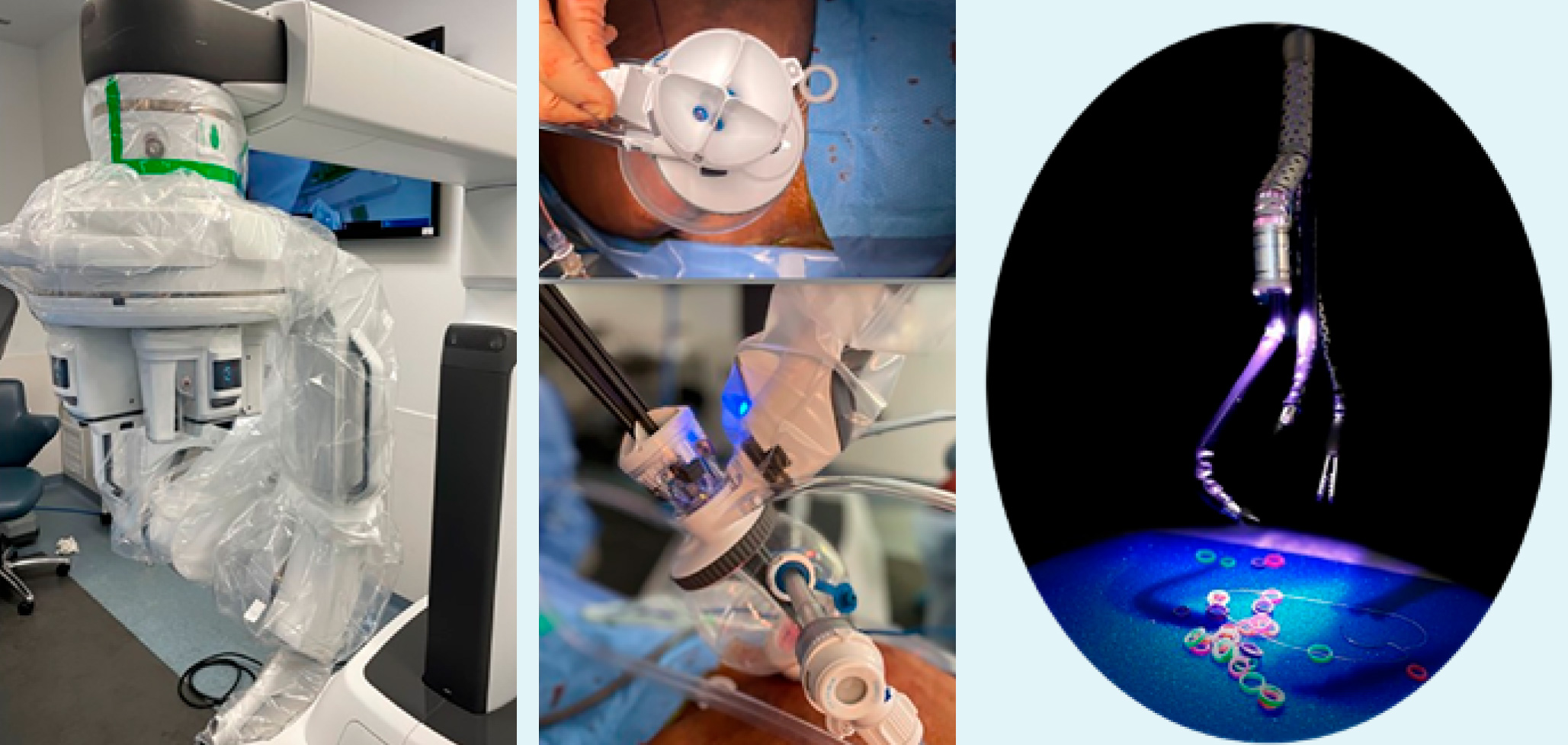
Figure 2: (a) daVinci SP single arm boom; (b) Access port with Airseal; (c) Camera and instruments deployed during a dry lab
A visual icon, called the “Navigator”, has been introduced on the screen to improve the coordination between instruments and the camera, enabling the surgeon to have a global visualization of all the instruments within the surgical space. The surgeon console mirrors the Xi console in both hand controls and foot pedals. The patient cart is the operative part of the robotic platform and encloses a single-arm boom and a patient arm (Fig. 2). The patient arm features four instrument drives in which instruments and scope are inserted, and a cannula arm that holds the port through which instruments are deployed. The SP flexible camera can rotate in all directions and therefore different perspective angles can be achieved while the instruments maintain a fixed position. Furthermore, a specific feature of the SP called “re-location” allows the entire platform to be moved in any direction around its fulcrum.
The camera and each instrument are positioned in the 12, 3, 6, and 9 o’clock positions within the trocar.
Port placement is flexible and allows for 360° of robotic docking.
A purpose-built “Access port” (Intuitive Surgical) allows for “floating docking”. This port exists in two sizes (small 2.4-5 cm; large 2.4-7 cm) and it includes the globe, an Alexis wound retractor, an “entry guide” (a 25-mm multichannel trocar that houses one entry channel for an 8 mm flexible 0° endoscope, and three other entry channels for the 6 mm robotic instruments), and an inflatable plastic globe which ensures adequate distance of the instruments from the surgical field. Through the Access port, there is also a 12 mm entry that can be used by the bedside assistant, and a lateral 8 mm entry which is usually used to insert a 5-8 mm Airseal® trocar (Conmed) (Fig. 2). Suction can be performed either an adapted 16-18Fr Nelaton tube or with a commercially available Remotely Operated Suction Irrigation (ROSI) system 112 (VTI, Nashua, NH USA), a flexible tube with a short rigid tip that the surgeon can handle throughout the surgical field. During partial nephrectomy procedures, a low-profile drop-in US probe is advisable, such as the L43K Robotic Transducer (Hitachi Aloka), can is preferred to facilitate handling. Moreover, the low-pressure SCANLAN® Reliance Bulldog LP Clamp can be used as it allows robotically controlled application (rather than done by the bedside assistant).
What procedures can be Done with the sp system?
The entire spectrum of urologic procedures can be done with the SP robotic system,9 with some specific ones that are more suitable for a system that is designed to work in narrow surgical fields (Table 1; Fig. 3).
Table 1: Most appealing SP robotic urologic procedures
| Procedure | Approach |
|---|---|
| Radical Prostatectomy | Extraperitoneal |
| Transvesical | |
| Simple Prostatectomy (Prostate enucleation) | Transvesical |
| Partial Nephrectomy | Retroperitoneal via lower anterior approach |
| Retroperitoneal via flank approach | |
| Nephro-Ureterectomy | Retroperitoneal via lower anterior approach |
| Pyeloplasty | Retroperitoneal via lower anterior approach |
| Transperitoneal (periumbilical) |
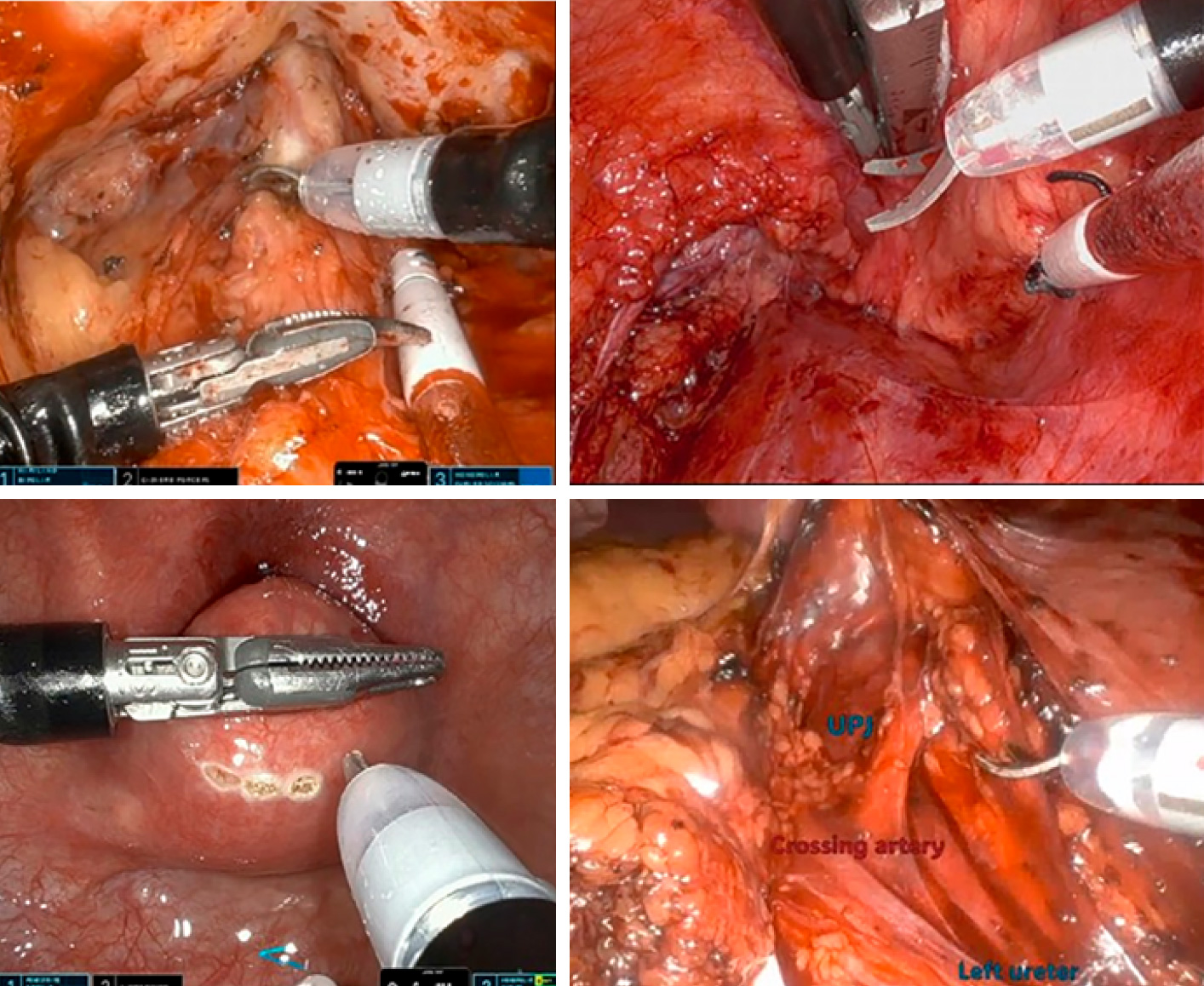
Figure 3: Examples of SP robotic procedures: (a) extraperitoneal radical prostatectomy, (b) intraoperative US during retroperitoneal partial nephrectomy via lower anterior access, (c) incision of the posterior plane during transvesical simple prostatectomy, (d) identification of crossing vessel during left transperitoneal pyeloplasty
While early SP series on radical prostatectomy (RALP) described a transperitoneal approach (and the use of a “plus one” trocar),10,11 over more recent years there has been a transition to alternative approaches.12 The extraperitoneal and transvesical SP-RALP appear to be the two most promising appealing ones, as they offer decreased invasiveness, potentially shorter length of stay, and better pain control.13,14 Despite being novel, SP-RALP was shown to be safe during the early phase of its clinical implementation. In a report by the SPARC collaborative group, of 1103 cases, intraoperative complications were noted in five patients (0.4%), all of which occurred during the transperitoneal approach.
Postoperative complications were noted in 143 patients (13%), with major ones being only 3.7%.15
SP robotic simple prostatectomy is being mostly performed via transvesical approach. The largest report to date by the SPARC group on 91 patients (mean prostate volume 156 mL) showed this could be a safe, pain-free, outpatient procedure.16 This has been renamed Robot-assisted SP transvesical enucleation of the prostate,17 as it can become competitive with more established enucleation techniques.
Surgical treatment of renal masses is another key application of SP robotic surgery. Partial nephrectomy (PN) was initially explored via transperitoneal approach.18 In a single-center comparative study, 30 SP cases were matched 1:1 to 30 multiport cases and there were no significant differences in operative time, estimated blood loss, ischemia time, transfusions rate, intraoperative complications, postoperative complications, and positive surgical margin rates. Patients undergoing SP-RAPN had a 30% reduction in median length of stay (median 25 vs 34 hours, p<0.003).19 Similar to the RALP experience, it was soon realized that the value of the SP lies in its use for retroperitoneal surgery. Pellegrino et al described a lower anterior retroperitoneal approach, with patient in supine position, that can be used for a variety of upper tract procedures.20 Several series with this approach for SP robotic PN were reported with very promising outcomes.21 In a recent report by the SPARC group, the “traditional” lateral flank approach and the new low anterior access were compared for SP retroperitoneal robotic PN.22 Both approaches were acceptable with comparable perioperative outcomes, but the lower anterior approach seems to be more versatile for varying tumor locations. In addition to PN, other kidney surgeries can be performed, including radical nephrectomy and radical nephroureterectomy. In this latter case, the SP platform allows to perform this multi-quadrant procedure via the lower anterior retroperitoneal approach.
Another procedure that seems to be a perfect fit for SP robotic surgery is pyeloplasty (as well as any other purely reconstructive ureteral surgery procedures). This is especially true when considering that the patient population in this case is young and therefore more interested in a good cosmetic outcome. The procedure can be safely and effectively performed with a 3-4 cm single incision via a trans-umbilical (transperitoneal) approach23 or a lower anterior approach.24
Advantages & challenges of sp robotic surgery
Implementing SP robotic surgery in a Center with an established multiport robotic program is at the same time a challenge but also a unique opportunity for growth and improvement.25 This requires a commitment by the entire surgical team to exit the comfort zone. A step-by-step approach can be used where indications can be limited to low-complexity cases and the approach can be initially a standard transperitoneal approach while one gets comfortable with the platform. However, a transition to the retro and extra peritoneal spaces is advisable after just a few cases. Similarly, the use of an additional (“plus one”) trocar can be an initial strategy, but this is not needed for most cases, except for selected PN and simple prostatectomy cases. Introducing SP robotics in an academic Center where there are residents and fellows to train might pose some challenges. On the other hand, it could be argued that younger (less structured surgeons) are more open-minded about acquiring a new technique. Therefore, it is key to gauge interest and motivate, to put in place educational hands-on opportunities. At the same time, a multiport robotic volume should also be maintained, also because the SP and the multiport robot have complementary (rather than alternative) roles.
While virtually anything can be done with the SP system, multiport robotic surgery is still a better option for “non narrow space” procedures (ie large tumor nephrectomies, radical cystectomies). Another consideration is that acquiring an SP system (which is now mostly reserved to Urology and transoral procedures) can translate into larger overall access to robotic surgery for the other service lines within the hospital.26
The main value of SP robotic surgery versus multiport surgery certainly lies in the opportunity for expanding the use of outpatient and same day surgery, and this can potentially become a cost-effective option.27
Conclusion
SP robotic surgery is one of the latest and most interesting innovations in the urology field. It has the potential to further minimize minimally invasive surgery by minimizing skin incision and surgical trauma, by facilitating the use of extra and retroperitoneal spaces, and therefore by expedite postoperative recovery, paving the way for outpatient robotic surgery.
Transitioning from MP to SP requires a shift in mindset and it involves a learning curve, but SP can be implemented safely, and it should not be considered as “against” multiport robotic surgery, but rather as an additional tool in the surgical armamentarium at the disposal of modern urologists. While cost can be regarded as an issue, it can be counterbalanced by potential savings in terms of hospital beds/days.
Last, but not least, as this is the first commercially available SP platform, it is foreseeable that its features will be further optimized.