Introduction
The aging of the population is a worldwide phenomenon. It has become increasingly evident due to the increase in average life expectancy and the decrease in births. Portugal is no exception and has become an aging country; thus, it is necessary to consider appropriate measures to respond to older adults’ needs (Carrilho et al., 2015). The Portuguese National Statistics Institute (INE) published in 2014 reveals that Portugal’s resident population will decrease until 2060, from 10.5 to 8.6 million residents. The aging index will increase from 131 to 307 older adults per 100 young people.
Aging is a natural and dynamic process that is progressive and irreversible, occurring from birth to death, and it characterizes itself as a series of physical, psychological, and social changes (Fechine & Trompieri, 2012). The decline in functional capacity is one of the most notorious aspects of the aging process, affecting neurological and muscular functions such as strength, flexibility, agility, and motor coordination. Another of the most notorious aspects of this process is cognitive decline, which is determined by memory loss, attention deficit, and logical reasoning difficulties. However, it differs in onset and progression. It depends on several factors, such as education, health, personality, and healthy lifestyles (Fechine & Trompieri, 2012). During its process and by how it happens, aging can be seen in two types: “normal and pathological aging.” “Normal aging” refers to organic and functional decline, a process that does not stem from the appearance of illness or any accident but an inevitable event over the years.
On the other hand, pathological aging is associated with stress, trauma, and diseases. These factors also tend to be related to premature aging, the incidence of chronic diseases, cardiovascular, blood pressure, osteoarticular diseases, and others, such as depression or dementia.
Dementia
As a result of an aging society, dementia is one of the serious public health problems of this century because of its dimension and how it harms the sick person and those around him. Dementia is characterized by a cognitive decline compared to a previous individual level, emphasizing memory loss and interferences in social and occupational activities. The onset is insidious, and its evolution is progressive and may occur over several months or even years (Alves, 2015).
Over 25 million people worldwide currently live with dementia, which has various types and causes. Early and accurate diagnosis is crucial, as dementia affects each person uniquely. The disease progresses rapidly for some, within months, while it advances slowly over several years for others. Dementia is typically categorized into early, moderate, and advanced stages. However, not everyone experiences all stages or exhibits characteristic symptoms.
In the early stage, individuals may show decreased interest, difficulties in learning new things and decision-making, irritability, vulnerability, trouble managing money, adapting to changes, and forgetting recent event details. In the moderate stage, problems become more pronounced. Patients often exhibit increased sadness, frustration, confusion, and disorientation in time and space. They may also show declining self-care regarding food and hygiene, inappropriate behaviors, and forgetfulness of recent events. In the advanced stage, the person becomes severely disabled and requires comprehensive assistance. There is a marked increase in confusion and irritability. While agitation and aggression are commonly seen in frontotemporal dementia, they can occur across various types of dementia (Tampi, 2023).
There are several primary types of dementia: progressive, irreversible degenerative dementia, and potentially reversible dementia. Irreversible dementias have been characterized by being more frequent and advanced. Lewy Body dementia, frontotemporal dementia, and Alzheimer’s disease belong to the irreversible dementia group, referred to as primary degenerative. Alzheimer’s disease is the most common type of dementia, affecting 50% to 65% of cases. Reversible dementias appear from vascular accidents, infectious processes, trauma, nutritional deficiencies, and tumors, among other pathologies (Bello & Shultz, 2011).
There is no effective cure for dementia. Most therapeutic programs to relieve cognitive deficits are based on pharmacological and psychotherapy interventions. Some programs combine cognitive rehabilitation programs, physical exercise, and music therapy. These therapeutic interventions efficiently promote behavior changes, autonomy improvements, and higher independence levels. They also improve both patients’ and caretakers’ quality of life.
Cognitive stimulation
Cognitive stimulation in older adults is characterized as an intervention that offers activities that stimulate cognitive functions such as memory, attention, concentration, and reasoning. The programs can be implemented individually or in groups. It is usually carried out during a particular time, fulfilling individual goals. This intervention aims to preserve or improve older adults’ performance or cognitive functions. Cognitive stimulation enhances the autonomy of older adults, decreases the risk of cognitive decline depression, and decreases the risk of dementia. Minor improvements, or even the stabilization of cognitive functions, can be considered significant health accomplishments an intervention with a positive economic impact. Combining the two types of intervention (cognitive stimulation and medication) would be ideal for obtaining positive results in initial and moderate dementia (Apóstolo et al., 2019). According to Giordano et al. (2010), patients with Alzheimer’s disease who received both types of intervention (cognitive stimulation therapy and medication) performed better than those who only received pharmacological treatment. These authors say combining pharmacological and non-pharmacological treatment improved attention, space, and temporal orientation.
According to an investigation by Santos et al. (2012), cognitive stimulation workshops for older adults with a slight cognitive decline, during an intermediary state between healthy cognitive aging and the initial state of dementia, improved cognition, socialization/integration, and meant an improvement in IADL (Instrumental Activities of Daily Life). Other improvements were observed, namely cognitive abilities, such as memory, attention, reasoning, and thinking. After cognitive stimulation, the older adults showed greater ease in remembering and memorizing and greater security in implementing IADL. Social activities helped older adults create new bonds of friendship, feel happier and more motivated, and reduce social isolation expressively. This study reveals that this intervention promotes autonomy and health and improves older adults’ quality of life.
Apóstolo et al. (2011) analyzed cognitive stimulation’s effectiveness in cognition, depressive symptomatology, and IADL in the community context. The study followed a pre and post-test design with a control group. The sample consisted of 23 participants, using their instruments to gather data on the Portuguese versions of the Montreal Cognitive Assessment (MOCA) and the Lawton Brody and Geriatric Depression Scale. The CSP (Cognitive Stimulation Program) was applied in the experimental group, with two weekly sessions for seven weeks. The results showed that older adults submitted to CSP improved their cognitive status. There is no significant evidence on the effect of cognitive stimulation on depressive symptomatology and IADL. However, it should be noted that 42.86% of the older adults in the experimental group, compared to 22.22% in the control group, evolved positively. The authors point out that the CSP contributes to maintaining the older adults’ cognitive health, delaying dementia and, consequently, respondents’ autonomy, independence, and quality of life. Therefore, it is suggested that cognitive stimulation should be included in care programs for older adults.
Quality of life
In the past decade, the concept of quality of life has been primarily utilized by physicians, researchers, economists, administrators, and politicians (Campos & Neto, 2008). Quality of life is closely linked to a healthy lifestyle and is often defined by the absence of diseases and the impact of their treatments. It is a quantitative measure to analyze how diseases and their treatments affect or limit an individual’s daily quality of life.
Numerous instruments have been developed to assess specific aspects of quality of life, tracking changes due to the natural course of a condition or the effects of particular interventions (Campos & Neto, 2008).
Greater longevity of human beings only makes sense if it corresponds to a good quality of life, constituting one of the significant challenges of the current society (Lobo et al., 2014). By adopting healthy lifestyles, active aging leads to a better quality of life in older adults, reducing the risk of diseases and promoting independence and autonomy in everyday activities.
The general purpose of the present study is to evaluate the impact of cognitive stimulation in older adults with dementia through the Portuguese version of the Apóstolo and Cardoso (2012) program of cognitive stimulation, “Making a Difference: An Evidence-based Group to Offer Cognitive Stimulation Therapy (CST) to People with Dementia. The specific goals were to evaluate the cognitive stimulation program’s effectiveness at the cognitive functional level and the quality of life of older adults with dementia.
Methods
The sample of participants in this study included 22 older adults with a clinical diagnosis of dementia. Based on the objectives of the study, the criteria defined for inclusion of the participants were: (a) Age equal or superior to 65 years; (b) Older adults, females or males with a clinical diagnosis of dementia; (c) Older adults in the early or moderate stage of the disease, able to participate in intervention activities.
Two groups of older adults were formed: an experimental group (EG) - undergoing a cognitive stimulation program, with 14 sessions performed once a week, and a control group (CG) - that will not be subject to any cognitive stimulation program.
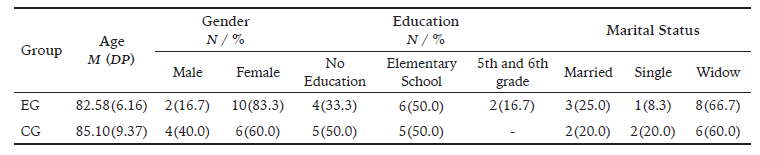
The sample was divided into 12 elements included in the EG and 10 in the CG. Table 1 shows the sociodemographic characterization of the two groups’ participants: age, gender, education, marital status, and employment status.
The experimental group (EG) consisted of 10 (83.3%) females and 2 (16.7%) were male, 6 (50.0%) attended elementary school, 4 (33.3%) had no schooling, and 2 (16.7%) attended the 5th and 6th grade, aged 73-95 years (M = 82.58, SD = 6.16). Regarding marital status, it is verified that the majority of 8 (66.7%) are widowers.
Concerning CG, 6 (60.0%) were female, 4 (40.0%) were male, 5 (50.0%) attended elementary school, and 5 (50.0%) had no education, aged between 67 and 99 years old (M = 85.10, SD = 9.37). Regarding marital status, it is verified that 6 (60.0%) were widowers.
Instruments
Several questionnaires were used in this study. The Mini-Mental State Examination (MMSE) aims to evaluate cognitive decline. The KATZ INDEX proposes to assess the functional independence of the older adults and the EUROHIS-QOL-8, allowing an easy and short, but also valid, instrument to evaluate the quality of life. A sociodemographic questionnaire was also used to obtain more accurate information about older adults (e.g., age, marital status, and education).
Mini-Mental State Examination (MMSE) - (Folstein et al. 1975). This test is easy and quick to apply and seeks to measure cognitive deficits; it was developed for clinical practice, mainly in the geriatric population. This test gathers questions from different cognitive domains, such as orientation, retention, attention, calculation, evocation, language, and constructive ability. Each item is scored on a scale of 0 or 1, depending on its achievement or correction of the answer. The maximum score is 30 points. The questions are answered in the instrument’s order, thus receiving an immediate score for each question. After finishing the test, correctly add the points assigned to each question, thus obtaining the final score. With the translation and adaptation of the MMSE for the Portuguese population, cut-off values are identified to detect a cognitive deficit, namely, less than or equal to 15 points for illiterate individuals, less than or equal to 22 points for intervals of 1 to 11 years of schooling and less than or equal to 27 points for level of instruction over 11 years (Guerreiro et al., 1994). This instrument is used to track cognitive losses and assess cognitive status. It is easy and quick to apply, allowing a brief assessment of the participant’s mental state and not diagnosing dementia. In this study, Cronbach’s Alpha coefficient was .81 and .82 for the pre and post-test, respectively, meaning strong reliability to the instrument.
Basic Daily Life Activities (DLAs) - Katz Index was developed to measure the physical functioning among patients with chronic illness. It measures six basic daily activities: bathing, dressing/undressing, using the bathroom, mobility, sphincter control, and feeding. In the version used for this study, the evaluation form has three categories: 6 points (independent), 4 points (moderate dependence), and ≤ 2 dependent. The higher the score, the better the older adults’ functionality and the higher their independence in the basic activities of daily life. The obtained score is based on the older adults’ current situation and not on the capacity to carry out the activities. In this study, Cronbach’s Alpha coefficient was .72 and .71 for the pre and post-test, respectively, which is a reasonable internal consistency value.
EUROHIS-QOL-8 was developed from the WHOQOL-BREF [EUROHIS Project] to be included in health surveys. Through several statistical procedures, the authors selected the items that obeyed the following criteria: retaining the WHOQOL-BREF domain structure, being Representative of the field in which they are inserted, being significant in most analyses performed, and not presenting problems of frequency or accuracy. Cross-cultural studies have shown that this short version of the instrument shows good internal consistency (Cronbach’s Alphas between .74 and .85) and the ability to discriminate patients from healthy individuals. It also presents good convergent validity with physical and mental health measures and good construct validity, validating the unidimensional structure (Comparative Fit Index [CFI] = .91; Root Mean Square Error of Approximation [RMSEA] ≤ .10). This index showed an instrument with good psychometric characteristics that allows an accessible, brief, and valid assessment of the quality of life assessment, justifying its translation and validation in different countries and languages. In the present study, Cronbach’s Alpha coefficient was .73 and .71 for the pre and post-test, respectively, being a reasonable internal consistency value.
Procedures
Previously, the project for this study was presented and approved by the Ethics Committee of Trás-os-Montes and Alto Douro University. The project was also submitted for approval to the Institution where the participants resided. Next, the respondents were selected. The participation was voluntary and formally authorized by the older adults’ relatives with a clinical diagnosis of dementia. Participants were informed about the nature and purpose of the study. They were assured that the data collected was confidential and would be used solely and exclusively for this study. In this way, the data was collected after clarifying questions related to the procedure and requesting the reading and completion of informed consent.
Data collection was performed at two different moments (pre- and post-test) in the EG and the CG. In order to evaluate the effectiveness of the Cognitive Stimulation Program (CSP) at the cognitive, functional, and quality of life levels of older adults with dementia, a first evaluation was performed using the MMSE, Kats Scale, and EUROHIS-QOL-8.
Then, the CSP was implemented in EG, during 14, 1 hour sessions from 11th January to 11th April, once a week. The main themes of the 14 sessions were: 1st Physical Games; 2nd Sounds, 3rd Childhood; 4th Food; 5th Current Issues; 6th Portraits / Scenarios; 7th Association of Words; 8ª Be Creative; 9th Classification of Objects; 10th Guidance; 11th Usage of money; 12th Games with numbers; 13th Games with words; and 14th Team games (Quiz).
Statistical analysis
The questionnaires were organized in a database using the SPSS Statistical Program, version 26.0. The assumption of the normal distribution of dependent variables in the different groups was verified by skewness and kurtosis.
In evaluating the efficacy of the cognitive stimulation program for older adults with dementia, a t-test for paired samples was performed to compare the cognitive, functional level, and quality of life in the pre and post-test moments. This test was performed (i) after verifying the compliance with the statistical assumptions for the use of this parametric test, (ii) by comparing two variables (scoring in pre and post-test moments) of a scale nature, and (iii) by comparing two dependent observation moments. When interpreting the test (PO), the following criteria scores were respected: >.80 - indicates an adequate test power and <.80 low test power, which may mean the sample size is small.
Results
This section analyzes the results to respond to the general objective and the present study’s goals. The assumption of normal distribution of the dependent variables in the different groups was verified by skewness and kurtosis, ranging from -.004 to -762. Thus, parametric tests were applied.
Table 2 shows that the cognitive stimulation program for older adults with dementia was ineffective in the cognitive, functional, and quality of life of older adults with dementia. No statistically significant differences were found between the EG and control groups. However, a slight decrease in the cognitive deficit (Mdif = .25), a slight increase in functional level (Mdif = -33), and quality of life (Mdif = -.083) was observed. Regarding CG, there was a decline at the level of the different variables measuring the quality of life (p < .05, which decreased in the second moment).
Table 2: Results of the pre and post-test on the functional level, cognitive level and quality of life.
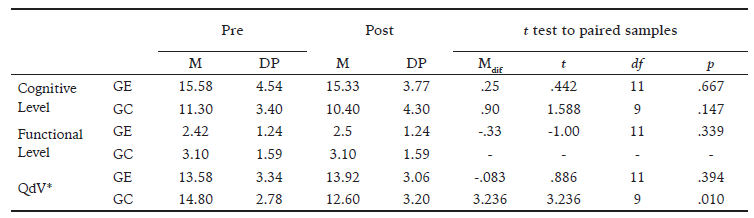
Even though the p values observed do not allow for the determination of statistically significant changes, it is relevant to note that the scores obtained demonstrated differences between the means in the desired direction. Overall, the cognitive stimulation group shows less decline, supporting the idea that cognitive stimulation may mitigate cognitive decline in Alzheimer’s patients. It should be noted that the CG presented a significant decline in quality of life.
Discussion
The results of the present study showed significant clinical outcomes. The scientific evidence on dementia shows that symptoms deteriorate with time. This study’s statistical analysis did not demonstrate statistically significant differences between the two evaluation moments in the cognitive stimulation program of older adults with dementia. However, there were improvements in the EG at several levels: functional (8.3%), cognitive (41.7%), and quality of life (41.6%). The obtained results also demonstrated stabilization of symptoms in several areas, namely at the functional (91.7%), cognitive level (16.7%), and quality of life (25.0%), thus presenting a revealing positive clinical significance.
Several studies have revealed the positive effects of cognitive stimulation programs on cognition, functional level, and quality of life in older adults with dementia. The study by Lira et al. (2011) demonstrated that cognitive stimulation enhanced participants’ performance on assessments measuring semantic memory, language skills, and executive functions. Concerning literacy, low education can interfere with performance in some cognitive activities. Older adults with low education levels presented more difficulties understanding some tasks. The study by Souza et al. (2009), which aimed to analyze cognitive functions in older adults, verified that individuals with more than eight years of education performed better in the proposed tasks. Apóstolo et al. (2019) evaluated the effect of a cognitive stimulation program, where the results pointed to a positive effect on older adults’ cognition. The sessions were performed three to four times a week. They showed small improvements or stabilization in cognitive functions, showing meaningful health achievements.
The Dias and Lima (2012) study on cognitive stimulation showed increased memory function performance. In total, 12 sessions of stimulation exercises were applied three times a week instead of the present investigation. It was applied only once a week. The number of weekly sessions seems relevant when implementing cognitive stimulation programs. To overcome this, researchers must overcome resistance from institutional administrators, caregivers, and healthcare workers. Caregivers and health workers fear such programs might increase their work overload. Administrators perceived it as another potential source of increased expenses.
Lindolfo et al. (2010) used cognitive stimulation activities to verify the autonomy of the IADL (Instrumental Activities of Daily Life) through the Lawton and Kats Scales. The older adults maintained their autonomy levels, thus preserving their independence from daily activities, reflecting the increase in older adults’ quality of life. These results were, to some extent, duplicated in our study.
Costa and Sequeira’s (2013) study evaluated a cognitive stimulation program’s effectiveness in older adults with a slight cognitive deficit. Results showed increased social interaction; the older adults living together became more communicative between themselves. The same was reported in our study by the institutional staff. Increased social interaction may become favorable as it improves or maintains cognitive functions (Costa & Sequeira, 2013).
According to clinicians and caregivers of the group studied, there were improvements in mood during the implementation of the cognitive stimulation program. That is, the older adults felt happier and more motivated. These data align with the results reported by Fonseca et al. (2016). They sought to study the benefits of a cognitive stimulation program in older people, obtaining results that pointed to improved interpersonal relationships and emotional states. The research by Santos et al. (2012) on the impact of a cognitive stimulation program showed improvement in the IADL, mainly manifested in the older adults’ autonomy. As is the case in the present research, older adults feel happier, demonstrating a reduction in social isolation. These aspects are fundamental because they clarify that the program significantly promotes health and improves older adults’ quality of life. In the present study, care providers who work daily with respondents reported behavioral gains among those who integrated the experimental group.
Finally, it is essential to realize that statistical significance is not synonymous with practical or clinical significance. A result can be statistically significant and irrelevant. When analyzing statistical results, one should consider the eventual occurrence of type I or II errors before making any decision. These errors are often overlooked in current research reporting practices in social and human sciences, yet their control is significant. In the clinical context, these statistical procedures may not be relevant. The present study results should be looked at considering the debate about the complementary between clinical validity and clinical utility. The clinical validity is demonstrated as results showed that cognitive stimulation contributes to slowing the progression of dementia. Thus, its integration should regularly be implemented since its positive effects are systematically demonstrated.
Based on the calculated effect sizes using Cohen’s d formula, the intervention had varying effects on the experimental group (GE) and control group (GC) across different domains. For the cognitive level, the effect size was negligible for the GE (d = -.055) and small for the GC (d = -.265), indicating that the intervention had little to no impact on cognitive functioning in either group.
Regarding functional level, the intervention showed no effect on the GC (d = 0) and a negligible effect on the GE (d = .065), suggesting that the intervention did not significantly influence functional abilities in the participants. However, the most striking result was observed in quality of life variable. While the GE experienced a negligible effect (d = .102), the GC showed a large negative effect size (d = -.791), indicating that the control group experienced a substantial decline in their quality of life throughout the study. Considering that the sample consisted of patients diagnosed with dementia, with the experimental group (EG) exposed to a cognitive stimulation program and the control group (CG) not receiving the intervention, the interpretation of the results can be statistically expanded. That is, the negligible effect sizes observed in the cognitive and functional levels for the EG suggest that the cognitive stimulation program may not have been sufficient to lead to significant improvements in these domains for patients with dementia. This could be due to the disease’s progressive nature, which may require more intensive or targeted interventions to yield substantial benefits. However, it is important to note that maintaining cognitive and functional stability in dementia patients is a positive outcome, as the disease typically leads to a gradual decline in these areas.
The large negative effect size in the quality of life domain for the CG highlights the potential impact of not receiving any intervention on the well-being of dementia patients. The decline in quality of life observed in the CG may be attributed to the lack of mental stimulation and engagement, which are crucial factors in maintaining overall well-being in individuals with dementia. This finding emphasizes the importance of providing support and interventions to dementia patients, even if the effects on cognitive and functional levels are not immediately apparent.
The stability in the quality of life for the EG, as indicated by the negligible effect size, suggests that the cognitive stimulation program may have had a protective effect on the participants’ well-being. Engaging in mentally stimulating activities and social interactions, often part of cognitive stimulation programs, can help maintain a sense of purpose, reduce feelings of isolation, and improve overall mood in dementia patients.
We could consider the Theory of Cognitive Reserve and neuroplasticity to explain this phenomenon better. The Theory proposes that engaging in mentally stimulating activities throughout life can build a “reserve” of cognitive resources. In the context of Alzheimer’s disease, patients with higher cognitive reserve may be better able to compensate for brain changes, showing less severe symptoms for a given level of pathology. The cognitive stimulation program may have helped to maintain or even enhance this reserve, allowing patients to better cope with the progression of the disease.
Neuroplasticity refers to the brain’s ability to form new neural connections and reorganize existing ones in response to learning and experience. Even in neurodegenerative conditions like Alzheimer’s, some degree of neuroplasticity remains. The cognitive stimulation exercises may have promoted the formation of new neural pathways or strengthened existing ones, helping to compensate for areas affected by the disease.
Other theories can also be used to explain the results. One of them is Cognitive Scaffolding. This Theory suggests that the brain recruits additional regions to support performance as particular cognitive abilities decline. Cognitive stimulation might enhance this process, allowing patients to utilize alternative neural networks more effectively to maintain cognitive function.
In the eyes of Stress Reduction and Cognitive Function Theory, engaging in cognitive stimulation activities might also reduce the stress and anxiety associated with the diagnosis, which could indirectly benefit cognitive performance. Lower stress levels are associated with better cognitive function in older adults. Another aspect to consider is Social Engagement. If the cognitive stimulation program involved group activities, social interaction could have contributed to maintaining cognitive function, as social engagement is known to protect against cognitive decline.
These theories could explain why the experimental group showed less decline, suggesting that targeted cognitive stimulation can potentially slow the progression of cognitive symptoms in Alzheimer’s disease by leveraging the brain’s remaining plasticity and compensatory mechanisms.
In the present study, the authors opted for a conservative interpretation of the combined results when faced with somewhat discrepant scores between p values, effect sizes, and power observed. Given the discrepancy between the statistical effect obtained and the probability of reproducing the studies, we opted for a more conservative decision criterion, favoring the non-occurrence of statistical effect (Dancey & Reidy, 2006) but claiming evidence of clinical utility of cognitive stimulation programs based on the results obtained.
One of the limitations is the sample size. Another aspect that we recommend is that future studies have a higher frequency of sessions per week. On the other hand, considering the scarcity of research in this area, mainly in Portugal, we emphasize the importance of more research on this topic with larger samples.
Conclusion
The cognitive stimulation program investigated in this study did not yield statistically significant changes in the primary dimensions measured among older adults with dementia. However, the clinical observations and reported improvements in cognition, quality of life, and functional skills suggest potential benefits not captured fully by quantitative data alone. These findings highlight the complexity of dementia and the possible limitations of traditional statistical methods in capturing the subtle but meaningful changes that occur in dementia care.
Despite the absence of statistical significance, the reported improvements by healthcare providers in social interactions, behaviors, and daily institutional engagement indicate that cognitive stimulation may play a crucial role in enhancing the quality of life for individuals with dementia. This underscores the importance of holistic approaches in care regimes considering measurable changes and qualitative benefits.
Further research with larger sample sizes and more refined measurement tools is necessary to explore the full impact of cognitive stimulation programs. This could help understand the specific elements of cognitive stimulation that contribute most effectively to slowing down the degenerative processes associated with dementia, thereby providing a more comprehensive approach to dementia care.
In conclusion, while the study’s quantitative outcomes do not confirm significant improvements, the clinical relevance of the observed changes calls for continued exploration of cognitive stimulation as a valuable component of dementia care strategies. This approach could potentially align more closely with the real-world impacts on patients’ lives, suggesting that cognitive stimulation should be considered a relevant therapeutic tool in a multi-faceted treatment plan for dementia.