Introduction
Recent literature reveals important relationships between cognitive function, depressive symptoms, and physical activity in older adults, both with and without Alzheimer’s disease. Manso and colleagues (2021) identified a significant link between high levels of perceived stress and depressive symptoms in physically active older adults. Their results suggest that practicing physical activity may alleviate these symptoms. The study by Mendes et al. (2021) showed that older women have a higher prevalence of depressive symptoms and functional dependence compared to men. This study highlights the importance of considering gender differences in the mental health of older adults. Glisoi et al. (2021) reported that cognition and functionality are interconnected, with older adults with Alzheimer’s presenting a higher risk of falls and worse cognitive performance. Finally, Bezerra et al. (2023) emphasized that regular physical activity can protect against neuroinflammation and improve cognitive functions, benefiting both healthy older adults and those with Alzheimer’s. These studies underscore the importance of physical activity in the mental and cognitive health of older adults.
Regular physical activity seems to benefit the preservation of several cognitive functions, which can reduce the risk of neurodegenerative diseases, namely Alzheimer’s disease, and thus promote healthy aging (Hernandez et al., 2010). It may delay the process of cognitive decline in an older person diagnosed patients with Alzheimer’s disease (Hernandez, et al., 2010). The effect of physical activity on Alzheimer’s disease is explained by its influence on metabolic and neuropathological changes linked to the neurodegenerative process, stimulating the growth of neurotransmitters responsible for cognitive functioning. Similarly, physical activity increases the production of endorphins, which decreases typical depressive symptoms in Alzheimer’s disease.
Similarly, the literature indicates the existence of an inverse and statistically significant association between physical activity and the presence of depressive symptoms since the physically active older person presents a lower incidence of depression compared to the sedentary older person.
There seems to be a consensus in the literature that physical activity may represent a protective factor and an essential non-pharmacological contribution to the reduction of depressive symptoms and maintenance of cognitive functioning in healthy and older adults with Alzheimer’s disease (Hernandez et al., 2010; Santana & Maia, 2009; Vital et al., 2012).
Therefore, the present research aims to compare older adults with Alzheimer’s disease and healthy older persons (control group) in a permanent system of institutionalization in terms of cognitive functioning and the presence of depressive symptomatology. More specifically, the research aims to:
To compare between the sexes, within the group of older people with Alzheimer’s disease and the control group, the presence of depressive symptoms and cognitive functioning.
To compare by the level of schooling, the group of older adults with Alzheimer’s disease and the control group, the presence of depressive symptoms and cognitive functioning.
To analyze the effect of family visits on the level of symptoms of depression and cognitive functioning in the older person with Alzheimer’s and the control group.
To compare, within the Alzheimer group and the control group, the physically active older person and the sedentary older person in terms of depressive symptoms and cognitive functioning.
Methods
Sample
The sample was collected at a host institution in the interior of Portugal. The stratified sampling technique was used to select and collect the sample. The sample consisted of thirty older adults divided into two groups: the Alzheimer’s disease group, which contains 15 older adults formally diagnosed with the disease, and the control group, comprising 15 older adults without neurodegenerative diseases. Participants were between 68 and 102 years old, with a mean of 84.10 ± 7.91 years old. The Alzheimer’s group consisted of ten males and five females, and the control group had five males and ten females. As for educational levels, 20% of the participants are illiterate, 73.3% completed the first basic education cycle, and only 6.7% completed the second (9th year).
Regarding the length of stay in the institution, 20% of the older persons live in the household between 1 and 3 years, 30% between 4 and 6 years, 16.6% between 7 and 9 years, and 23.4% of the participants are institutionalized ten or more years. Of the total sample, 23.3% reported never receiving a family visit, 40% received a family visit only during festive seasons, and 36.7% received a family visit one or more times a month.
Instruments
The same questionnaire was applied to both groups. The first part of the questionnaire contains questions aimed at collecting the sociodemographic data of the sample, namely age, sex, educational level, length of stay in the institution (in years), the frequency with which the family visits the older person, the level of physical activity and, if the older person practices physical activity, how many times a week. The second part of the questionnaire contains the Geriatric Depression Scale of Sheikh and Yesavage (1986), translated, calibrated, and adapted for the Portuguese population by Veríssimo (1988) to verify the existence of depressive symptomatology in older persons. The scale consists of 30 closed-response items (“yes” and “no”), and each item that translates to the presence of a characteristic symptom of depression is 1 point. The cutoff point that indicates the possibility of occurrence of depression in the older person is eleven or more points.
The third part of the questionnaire, the Mini-Mental State Examination (MEEM) by Folstein, et al. (1975), was adapted for the Portuguese population by Guerreiro et al. (1994). This questionnaire aims to evaluate aspects related to cognitive functioning, such as spatiotemporal orientation, reasoning ability, attention, calculating ability, memory recall, and language. The MMSE score can range from 0 to a maximum score of 30 points. Cutoff points to indicate the presence of cognitive decline depend on the level of schooling of the examinee: 22 points for illiterate elders or up to two years of schooling, 24 points for older persons with 3 to 6 years of schooling, and 27 points for the older person with seven or more years of schooling.
Procedure
After obtaining the authorization, the older persons were selected to participate in the study with the help of health professionals, according to established inclusion criteria: age 65 or older, being diagnosed, formally or clinically, with Alzheimer’s disease in their onset (initial stage), to belong to the Alzheimer group and accept to be submitted to the application of the questionnaires. Older people with communication and interpretation difficulties, hearing impaired, older persons with unspecified dementia, and older persons with Alzheimer’s disease in the advanced stages were excluded from the sample.
Two nursing professionals oversaw the administration of the questionnaire in the nursing department, safeguarding the anonymity of all participants and the institution’s identity.
Statistical analysis
Data analysis was performed using Statistical Package for Social Sciences (SPSS) version 20.0. Cronbach’s α assessed instrument reliability. Internal consistency was calculated, considering MANOVA conditions. Due to the small sample size, Box’s M test was used to verify multivariate normality (Dancey & Reidy, 2006). The effects of independent variables on dependent variables were examined using multivariate analysis of variance (MANOVA) and univariate analysis. Pearson’s correlation coefficient measured the relationship between the two dependent variables.
Independent variables included Alzheimer’s disease status, gender, education level, frequency of family visits, and physical activity. Dependent variables were depressive symptoms (measured by the Geriatric Depression Scale) and cognitive functioning (assessed via the Mini-Mental State Examination).
As no participants engaged in physical activity, its effect on depressive symptoms and cognitive functioning was analyzed by comparing sample means with those from similar studies involving physically active older adults. A one-sample t-test evaluated the effect of physical activity status (active vs. sedentary) on dependent variables, assuming normal data distribution (Dancey & Reidy, 2006).
A significance level of 5% (p < .05) was applied throughout the analysis.
Results
Internal consistency analysis using Cronbach’s α revealed high reliability for both instruments: the Geriatric Depression Scale (α = .88) and the Mini-Mental State Exam (α = .94). The Box’s M test for variance-covariance homogeneity yielded p = .772, indicating that the homogeneity assumption of variance-covariance matrices was not violated. This result supports the use of parametric tests.
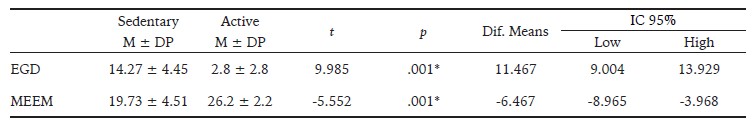
Table 1 presents the descriptive data on depressive symptoms and cognitive functioning of the study population. The mean score obtained in the Geriatric Depression Scale (EGD) is 19.53 ± 6.43, which indicates the presence of depressive symptomatology. In the Mini-Mental State Examination, the mean of the results was 13.56 ± 7.57.
Table 1: Descriptive Analysis of Dependent Variables in the Sample: Depressive Symptoms and Cognitive Functioning.
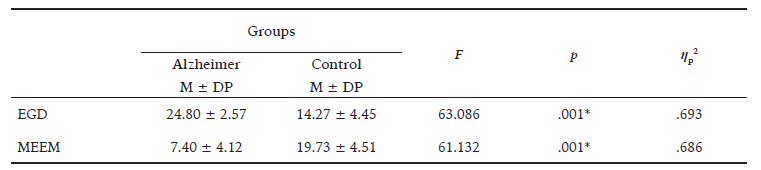
In order to compare the Alzheimer group with the control group in the presence of depressive symptoms and cognitive functioning, constituting the general objective of the investigation, it is verified that the values of the multivariate analysis show statistically significant differences between the two groups concerning the dependent variables, where a statistical effect and a high observed power are emphasized [Wilks’s λ = .204, F(2, 27) = 52.618, p = .001, η p 2 = .796, OP = 1]. To verify the influence of Alzheimer’s disease on the dependent variables separately, we used the univariate analysis. There are significant differences between the groups in the results of the Mini-Mental State Examination [F (1, 28) = 61.132, p = .001, η p 2 = .686] and the Geriatric Depression Scale [F (1, 28) = 63.086, p = .001, η p 2 = .693]. A strong observed power was obtained, suggesting that 100% of the variation of the results obtained in the Mini-Mental State Examination are in the 95% confidence interval of the marginal means (11.95 - 15.18). Likewise, there is a strong power of 100% in the variation of the results of the Geriatric Depression Scale within the confidence interval of 18.17 - 20.89.
As can be seen in Table 2, the older adult in the Alzheimer group presents higher scores on the Geriatric Depression Scale and lower scores on the Mental State Mini Exam compared to the older person in the control group, who, although presenting values indicative of depressive symptomatology and cognitive decline, are significantly lower than those in the Alzheimer group.
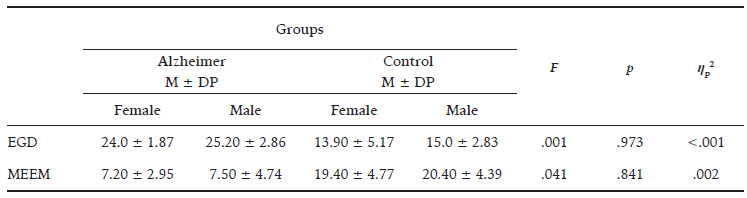
Regarding the specific objectives, there are differences between the sexes within the Alzheimer group and the control group in terms of depressive symptoms and cognitive functioning. As shown in Table 3, in the Alzheimer group, the older men obtained a higher score on the Geriatric Depression Scale (25.20 ± 2.86) and the Mental State Mini Exam (7.50 ± 4.74), compared to the female sex. The same phenomenon is observed in the control group, in which the older men present higher values than the female sex in the presence of depressive symptoms (15 ± 2.83) and in the level of cognitive functioning (20.40 ± 4.39).
The differences between the sexes at the level of the dependent variables in the two groups are not statistically significant [Wilks’s λ = .998, F(2, 25) = .020, p = .981, ηp2 = .002], showing weak power which suggests that 5.4% of the variations in the results of the Mini-Mental State Examination and 5% in the results of the Geriatric Depression Scale can be attributed to gender, given the confidence interval of 11.85 - 15.40 (MMSE) and 18.04 - 21.01 (EGD).
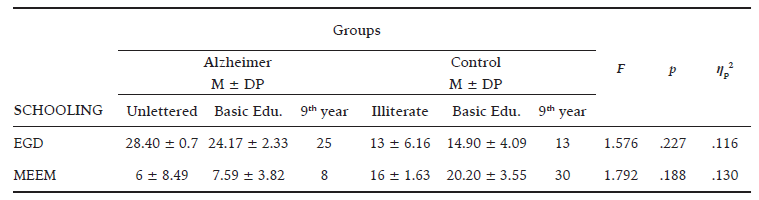
Regarding the variable educational level (Table 4), the results of EGD and the MMSE seem to have no influence. Despite an increase in MMSE performance due to a higher educational level, these differences are not statistically significant, either in the older person group with Alzheimer’s disease or in the control group. However, there is a moderate statistical effect [Wilks’s λ = .758, F(4, 46) = 1.709, p = .164, ηp2 = .129]. The observed power indicates that 30.1% (EGD) and 33.7% (MMSE) of the variability of results are attributed to schooling. The 95% confidence interval of the marginal means ranges between 17.59 - 21.93 in the EGD and 12.37 - 16.90 in the MEEM.
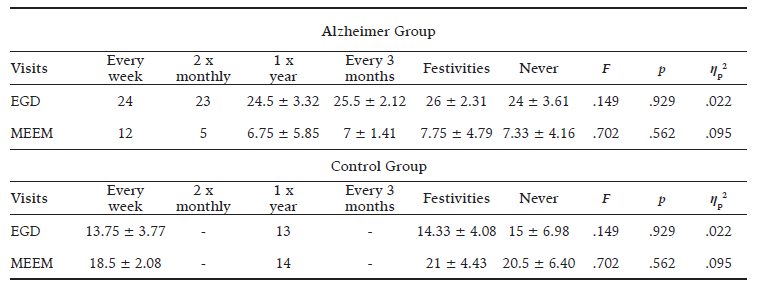
As can be seen in Table 5, when we verified the effect of family visits on the incidence of depressive symptoms and cognitive functioning, we did not observe statistically significant values in the results of dependent variables in Alzheimer’s and control groups [Wilks’s λ = .880, F(6, 38) = .419, p = .862, ηp2 = .062]. However, although they were not significant values, mean effects were obtained, indicating that 7.3% (EGD) and 17.2% (MMSE) of the variations are due to the frequency with which the older person receives visits. The confidence interval of marginal means at 95% significance is between 9.79 and 14.18 in the MEEM and 18.35 and 22.64 in the EGD.
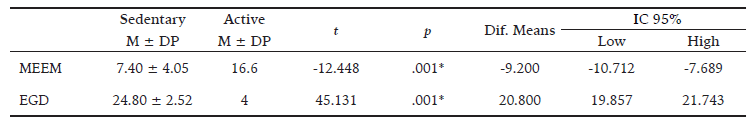
In order to compare the physically active older person with the sedentary older person in the incidence of depressive symptoms and cognitive functioning and because the sample was sedentary, the results of the dependent variables were compared with the results of a study by Silva and Santos (2009), who uses the same instruments and methodological procedures as the present investigation to measure the presence of depressive symptomatology and cognitive functions (Table 6).
When comparing the sedentary older person of the control group with the active older person concerning the presence of depressive symptoms, measured through the Geriatric Depression Scale, the mean value obtained in the EGD of the sedentary individual was 14.27 ± 4.45, the presence of depression. In contrast, the active elder had a value of 2.8 ± 2.8, indicative of the absence of depression. Using the one-sample t-test, we verify the statistically significant differences between active and sedentary older adults regarding the incidence of depressive symptoms (t = 9.985, p <.001).
Regarding the effect of physical activity on the cognitive functioning of the older person, it is possible to observe that the active older adult obtained significantly higher values in the Mini-Mental State Examination than the sedentary older person (t = -5.552, p = .001).
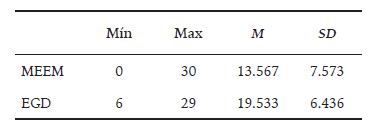
In the Alzheimer group, a study by Groppo et al. (2012) was used to compare older and older people with active depressive symptoms and cognitive functioning. Six older person women with Alzheimer’s disease underwent a six-month physical activity program (Table 7), whose methodological procedures were identical to the present study’s.
Thus, there are significant differences between the two groups in terms of cognitive functioning (t = -12.448, p ≤ .001), and the older person with Alzheimer’s disease who practice physical activity show more remarkable preservation of cognitive abilities and a lower incidence of depressive symptoms, compared to the sedentary person.
Discussion
This study aimed to compare healthy and institutionalized older persons with Alzheimer’s disease concerning depressive symptoms and cognitive functioning, considering the influence of variables such as sex, level of schooling, frequency of visits, and practice of physical activity. In the present investigation, it is verified that older adults with Alzheimer’s disease and inactive older persons present lower preservation of cognitive functions and a greater prevalence of depressive symptoms compared to older persons without dementia and those who practice physical activity.
The results showed that the older person with Alzheimer’s disease presents a more significant impairment of cognitive functions and a greater incidence of depressive symptoms compared to the older person without neurodegenerative diseases that were part of the control group, corroborating the hypotheses of investigation and against the results found in the literature (Groppo et al., 2012). This phenomenon occurs due to the progressive deterioration of brain areas characteristic of Alzheimer’s disease, leading to a decline in cognitive ability and an increase in apathy in the older person. However, the mean results obtained in the Geriatric Depression Scale are predictors of the presence of depressive symptomatology in the entire sample, which can be explained by the fact that they are institutionalized, which in itself constitutes a risk factor (Alencar et al., 2011).In comparing the sexes in the older person group with Alzheimer’s disease and the control group, no differences were recorded in the data obtained through the Geriatric Depression Scale and Mini-Mental State Examination. However, studies show that the mean of depression is in older women institutionalized without neurodegenerative diseases (Bandeira, 2012).
Regarding the influence of the educational level on the incidence of depressive symptoms and the cognitive functioning of the older person, this association is not significant despite a better performance in the Mini-Mental State Examination in older persons with higher educational levels. A low level of schooling (less than four years) is one of the factors described in the literature as being consistently associated with a worse performance in the MMSE (Bandeira, 2012; Espino et al., 2001; Valle et al., 2009).
In the association between symptoms of depression, cognitive functioning, and family visits, although it is not significant, it is essential to note that there is a higher incidence of depressive symptoms in older persons receiving less frequent family visits. The loss of family ties may be a risk factor and an intensifier of depression, and the institutionalized older person needs to strengthen social and family relationships to reduce feelings of sadness, loneliness, and hopelessness linked to their institutionalization (Bandeira, 2012).
Comparing active and sedentary older adults, both with and without Alzheimer’s disease, reveals that those who engage in physical activity exhibit fewer depressive symptoms and better-preserved cognitive functions. The results of previous studies have shown a significant association between a moderate to high level of physical activity and a lower risk of cognitive impairment, thus reducing the risk of neurodegenerative diseases (Etgen et al., 2010; Gobbi & Stella, 2010; Hernandez et al., 2010; Silva & Santos, 2009). Likewise, there is evidence that older people who practice physical activity regularly since adolescence and/or adulthood present more remarkable preservation of cognitive abilities, namely in speed of information processing and memory, than inactive older people. In older persons with Alzheimer’s disease, investigations in this area demonstrate that regular and systematized physical activity contributes to preserving and improving several cognitive functions (Coelho et al., 2009).
The effect of physical activity on cognitive functions is explained by its influence on the brain level. The brain, characteristic of its plasticity, tends to lose volume with advancing age, affecting various cognitive functions. However, the practice of physical activity preserves the volume of the areas responsible for cognitive abilities, namely the frontal, parietal, and temporal cortex, including the hippocampus, by reducing gray matter loss (Erickson et al., 2012).
Concerning the decrease in depressive symptoms, physical activity is a non-pharmacological alternative to treatment since studies conducted with older person people show that the practice of physical exercise for three days per week has a significant effect on the reduction of symptoms of depression. Due to their action on the release of endorphins in the body responsible for increasing the sense of well-being, the practice of physical activity may constitute a factor of protection of mental health (Groppo et al., 2012; Pérez & Carral, 2008).
Finally, this study aims to increase the scientific community’s knowledge of the benefits of physical activity in older person, considering the importance of regular practice in preserving cognitive functions and maintaining their mental health.