Introduction
Vertigo and dizziness affect around 20-40% of the general population and are among the most common medical complaints in emergency rooms.1 Benign paroxysmal positional vertigo (BPPV) is the most common type of vertigo. (2 The reported incidence of BPPV is 0.6% per year and the lifetime prevalence is 2.4% of the population. (3 In BPPV, detached otoconial debris from the utricular macula moves around in the semicircular canal or attaches to the ampullary cupula, which causes recurrent vertigo induced by positional changes of the head. (3 Those symptoms are associated with a considerable personal and health care burden, as they generally require medical consultations and lead to disruption of daily activities and absenteeism. (4) Although most commonly BPPV is idiopathic, it maybe also be secondary to head trauma, Ménière’s disease, or Vestibular Neuritis. (5) Age and gender has been reported as risk factors for BPPV. BPPV is more common in individuals in their 50s and 60s, and the rate of occurrence is 2:1 to 3:1 in women and men. (3,6
Seasonal variation in BPPV has been evaluated in several studies with diverging results. While some studies found indications of seasonal variation7, other studies did not confirm these findings. (8 In a tropical region study, vertigo was more frequent in late winter-spring, negatively correlating to humidity and rainfall. (9 According to an earlier study, the incidence of BPPV was associated with monthly changes in air temperature and pressure. (10 In a large study of the German population, no seasonal variation was demonstrated for any vestibular disorder. (8) Considering the scarce and conflicting reports on the subject, this study aimed at analyze the existence of a seasonal distribution of BPPV, and the correlations of these findings with climatic factors.
Material and Methods
Data collection
Patients who visited the emergency room of Centro Hospitalar Universitário Lisboa Central (latitude: 38.7177640, 38°43’04.0”N; longitude: -9.1374533, 9°08'14.8"W) with vestibular symptoms from January 1 to December 31, 2021, were enrolled in the study. The diagnosis of BPPV was confirmed by symptoms consistent with BPPV as well as typical nystagmus during diagnosis maneuvers. Proper canalith-repositioning maneuvers were performed according to the affected canal. Secondary BPPV patients who have specific causes for BPPV such as head trauma were excluded from the study. The number of patients diagnosed with idiopathic BPPV was calculated weekly.
A total of 5339 patients were seen by Otorhinolaryngology in the emergency room during this period. Of these, 494 had vestibular symptoms and 178 were diagnosed with idiopathic BPPV.
Age, sex, lesion side and the involved semicircular canal were analyzed. Differences among the week and seasons of BPPV diagnosis were evaluated. Spring started from 21st of March to 20th of June; summer from 21st of June to 20th of September; autumn from 21st of September to 20th of December; and winter from 21st of December to 20th of March.
Climate factors were collected daily from the Humberto Delgado Airport Meteorological Station, including daily average atmospheric temperature (°C), atmospheric pressure (hPa), humidity (%), cloud amount (cloud covered area, expressed as 10 fractions of the whole sky), daylight time (h/day) and solar radiation (Kwh) in Lisbon Metropolitan area. The weekly mean value of each factors represented an arithmetic average of the daily values.
Data analysis
Simple correlation analysis was performed to evaluate the association between the number of BPPV patients diagnosed per week and the weekly mean value of climate factors. Statistical analysis was performed using IBM SPSS Statistics version 19 (IBM Corp., Armonk, NY). Statistical significancy was set at p values less than 0.05.
Results
Sample characteristics
The age of the 178 patients diagnosed with idiopathic BPPV ranged from 24 to 91 years, and their mean age was 54.9 (±14.8) years. There were 62 male (34.8%) and 116 female (65.2%). The number of females was 1.87 times higher than that of male. The clinical charts revealed that the posterior semicircular canal was the most frequently involved, 101 patients (56.7%). The right side was affected in 99 patients (55.6%) and the left side in 79 (44.4%).
Seasonality of BPPV
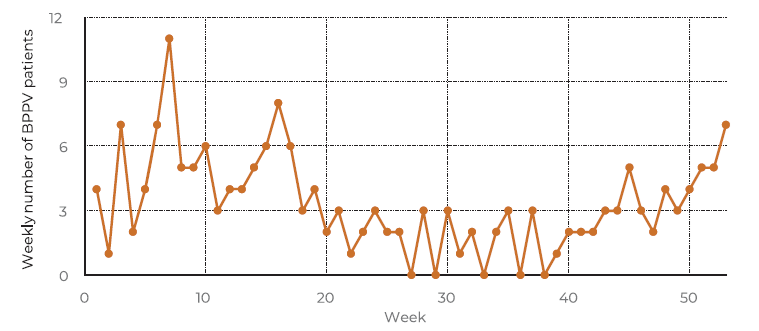
The weekly number of patients diagnosed with BPPV is presented in Figure 1. The average number of BPPV patients per week was 3.42. A seasonality variation was found in the incidence of BPPV, with a lower number of patients diagnosed with BPPV in the summer months (p = 0.0002), despite an increase in the total number of patients in the Otorhinolaryngology emergency room (p = 0.0008) in this period. The winter months correspond to the period the most cases of BPPV.
Association to climatic factors
Weekly distribution of climate factors can be seen in Figure 2. The average temperature was the lowest in January (8.25 °C) and the highest in August (23.50 °C) (Figure 2a). The month with the lowest atmospheric pressure was February (1013.75 hPa) and the highest month was December (1024.80 hPa) (Figure 2b). The month with the highest average humidity was February (86%) and the month with lowest humidity was July (55.6%) (Figure 3c). Total cloud amount was the lowest in July (10.4%), and the highest in December (48.6%) (Figure 2d). The lowest month for daylight time hours was December (9.52 h) and the highest month was June (14.88 h) (Figure 2e). The month with the lowest value of sunshine amount was December (1.40 KWh) and the month with the highest amount was July (8.02 KWh) (Figure 2f).
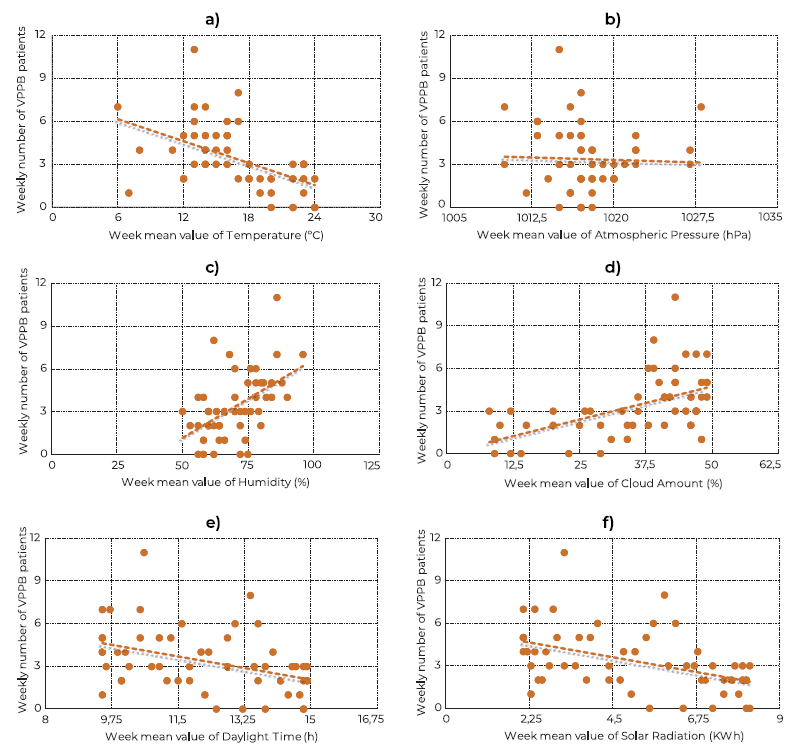
The association between the weekly number of BPPV patients and the weekly mean value of climate factors are presented in Figure 3. Simple correlation analysis revealed a significant negative association between atmospheric temperature (r = -0.5215, p = 0.000063), daylight time (r = -0.4024, p = 0. 002847) and solar radiation (r = -0.4463, p = 0.000817) with the number of BPPV patients diagnosed per week. A positive and significant association was found between cloud amount and the incidence of BPPV (r = 0.537, p = 0.000034). No statistically significant association was found between atmospheric pressure (r = -0.0366, p = 0.798015) or humidity (r = 0.2525, p = 0.068707) with the incidence of BPPV.
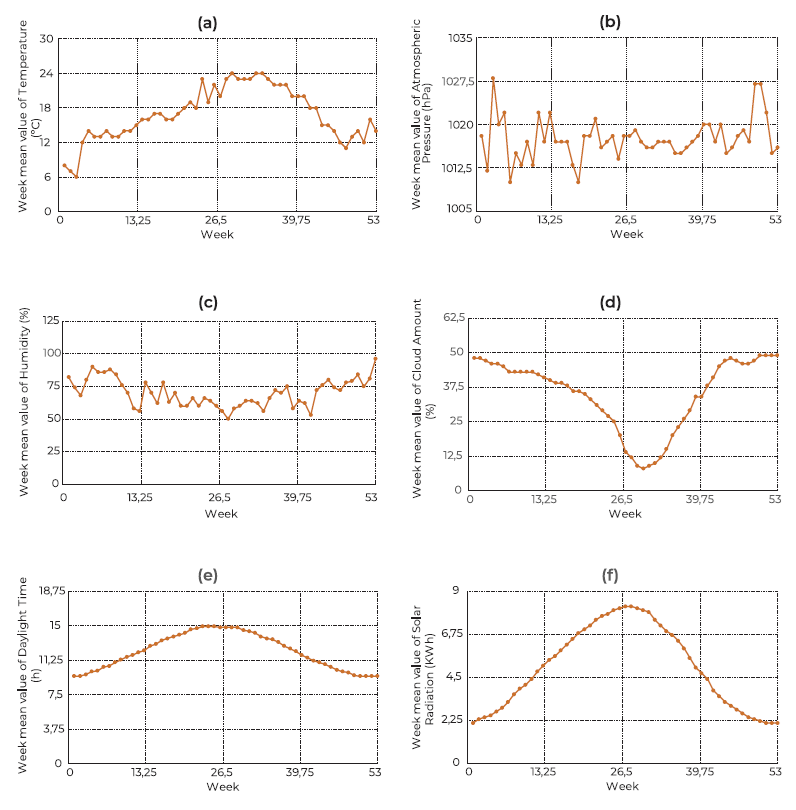
Figure 2 Weekly distribution of climate factors:(a) atmospheric temperature, (b) atmospheric pressure, (c) humidity, (d) cloud amount, (e) daylight time and (f) solar radiation.
Discussion
BPPV is the most common vestibular disorder across the lifespan and frequently presents with a limited period with clusters of episodes, followed by an interval of no attacks before recurring again. (10 The BPPV 5-year recurrence rate was reportedly around 50%.11 The results of this study are in agreement with those reported in the literature regarding the age, gender, semicircular canal and affected sides. (12
In order to minimize BPPV incidence and recurrence, it is necessary to understand the pathophysiology of BPPV and to investigate the factors associated with it. Several studies have reported seasonal variation in BPPV. Whitman et al. analyzed 956 visits for BPPV over 5 years in Boston (United States of America), and reported that the incidence of BPPV was significantly higher during the early spring months (March to May). (13 Zuma e Maia et al. evaluated 214 patients with BPPV , over 6 years, in Porto Alegre (Brazil) and reported an association between the incidence of BPPV and solar radiation, with more patients with BPPV during the autumn and winter, when there was low solar radiation. (12 Shu et al. evaluated 1269 patients with BPPV in Shanghai (China), over 6 years and reported an increase in BPPV incidence in winter months and also a moderate negative correlation with patients serum 25-hydroxyvitamin D levels. (14 On the contrary, Seidel et al. examined 11153 patients with BPPV using a large German nationwide database and reported no seasonal variation. (9) In our population, we found that the incidence of BPPV decreases in the summer months and that has its peak in winter period.
The effects of climate factors are related to the amount of time spent indoors and outdoors, which differs between weekdays and the weekends. (7 We calculated BPPV incidence and climate factors weekly to reduce this effect. Saeed et al. demonstrated a correlation between temperature and the incidence of BPPV. It has also been reported that an increased incidence of BPPV is associated with a seasonal decrease in serum vitamin D levels. (15 Calcium is the main component of otoconia in the utricular macula, and the metabolism of calcium is affected by vitamin D. (2) The synthesis of vitamin D is influenced by skin exposure to ultraviolet B radiation, season, time of day, cloud amount, latitude, altitude, air pollution, clothing, and sunscreen use. (12,15) Consequently, the increase in cloud amount may decrease serum vitamin D levels, which may result in increased BPPV occurrence. (16 As there is a great interconnection between climatic factors, our study analyzed six of them. As result, we demonstrated a significant negative and statistically significant association between atmospheric temperature, daylight time and solar radiation with the number of BPPV patients diagnosed per week; and a positive and significant association between cloud amount and the incidence of BPPV.
There are several limitations to this study. First, our study is retrospective in design and only included data from a single Lisbon tertiary institution. Second, this study included patients with BPPV who had visited our Otorhinolaryngology emergency room and did not include patients with BPPV who had visited other departments, such as the Neurology Department. However, at our institution, the great majority of patients who visited other departments were referred to the Otorhinolaryngology emergency room when BPPV was suspected. Despite these limitations, we were able to include a large number of patients with BPPV and showed climate factors that could explain the seasonal variation in BPPV incidence. Additional studies based on prospective multi-center data are required.
Conclusions
In our population, the incidence of BPPV decreases in the summer months, when atmospheric temperature, solar radiation and daylight time are higher and cloud amount is lower. No association was found between atmospheric pressure or humidity with the incidence of BPPV.
Conflicts of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Data Confidentiality
The authors declare having followed the protocols in use at their working center regarding patients’ data publication.