1.Introduction
In 2017, the Universal Health Coverage Forum proposed the people-centered health services approach. This suggested a change in the way of understanding health, in which the social and cultural dimensions of health acquired significant relevance (WHO, 2017). Studying the cultural influence on the effectiveness of health interventions is relevant because interventions that lack meaning from the perspective of the target population's cosmovision or are not practical in their context, may be less effective (Bautista-Gomez et al., 2022).
Due to this, cultural adaptation arises as a necessity since it alters an intervention or program to better respond to the needs and cultural characteristics of the population and the implementation context (Card et al., 2011; Pasick et al., 1996). Requiring careful planning and execution, and involving the participation of users for whom the adaptation is being designed, as it aims to improve the cultural appropriateness, acceptance, and feasibility, without compromising the expected results of the intervention (Card et al., 2011).
Cultural adaptation takes relevance in the case of economically vulnerable ethnic populations who face great challenges to accessing the health care system, and present poor health conditions. Evidence suggests that culturally tailored interventions are a promising way to improve healthcare equity and quality for minority populations (Fisher et al., 2007; Torres-Ruiz et al., 2018) improve healthcare outcomes (Joo & Liu, 2020), knowledge of self-care and accessibility of health care systems (Fisher et al., 2007), among others.
However, cultural adaptation continues to be an under-explored field of research, particularly in contexts of vulnerability. The systematic reviews and meta-analyses conducted to establish the effectiveness and efficacy of culturally tailored interventions with ethnic minorities have been executed for developed or upper-middle-income countries (Liu et al., 2012; Vincze et al., 2021; Hosseini et al., 2024) but few systematic reviews put the lens on low-middle-income countries (LMIC) (Tawankanjanachot et al., 2023; Li et al., 2023). Considering the differences in socioeconomic structural factors between these groups of countries, the findings for the former group cannot be extrapolated for the latter. Further research is needed to comprehend what factors, under which circumstances, can contribute to improving the health outcomes of culturally adapted interventions with vulnerable populations in low-middle-income countries (LMIC)
Therefore, a qualitative evidence synthesis (Grant & Booth, 2009) was conducted to explore studies reporting cultural adapted health interventions with ethnic groups in vulnerable settings. The aim was to understand how cultural adaptations have been designed and implemented, and how they have contributed to improving health outcomes in low and middle-income countries.
2.Methods
This qualitative evidence synthesis was carried out using a PICo question, as recommended by the Cochrane handbook for qualitative systematic review (Noyes &Harden, 2023), which was: how culturally adapted health interventions are designed and implemented, and which outcomes do they get when they are held with ethnic groups in low- and middle-income countries?
2.1Selection criteria
The eligibility criteria (Supplementary material 1. Eligibility criteria filter) followed was: (a) methodology must be qualitative or at least mixed methods; (b) it must report the design, implementation or assessment of a culturally adapted health intervention; (c) the interventions must be aimed for indigenous, afro-descendant or other ethnic populations, (d) they must be located in LMIC countries; (e) articles must be written in English, Portuguese, or Spanish; (f) be an article published in a scientific journal, (g) be published after 2012, and (h) contains the descriptors (cultural tailoring, health interventions, and ethnic groups) in its title or abstract. For this synthesis, studies were not grouped in a particular way.
2.2Search Strategy
A search strategy was undertaken. Keywords and combinations used included terms related to cultural tailoring, health interventions, and ethnic groups (See Supplementary material 2. Search strategy)). Translation of these terms to Spanish and Portuguese was included, and the full list of LMIC (Low- or Middle-Income Country (LMIC), n.d.). The search was done in PubMed, Web of Science, and SCOPUS in December of 2022.
2.3Data Extraction and Analysis
An analytical matrix was created (Supplementary material 3. Selected papers analytical matrix) with the overview of studies selected, related to objective, methods, target population, health issue addressed, and typology of cultural adaptation. Two reviewers worked independently in this process (LSZ, MFMT) and doubts were solved with a third reviewer (MMBG). For the synthesis process, a narrative synthesis of the main stages of the health interventions (design, implementation, and evaluation) was carried out.
Then a thematic analysis was developed, using analytical categories according with existing literatureabout cultural adaptations.
Based on Healey et al. (2017) framework, the categories assessed in the design stage were: community participation (incidence of the population in different stages of the intervention), service delivery (changes to better respond to the population’s needs), and content (changes that actively respond to the characteristics of the population). In the implementation stage, barriers and facilitators were analyzed; related to cultural, contextual and structural issues that impacted the development of the intervention.
Finally, 4 outcomes were inferred from the Card et al. (2011) guidelines for suitable effective program: effectiveness (the intervention’s goal was accomplished), acceptability (the population and/or community is satisfied), disease knowledge (better understanding of the health issue by the population), and feasibility (capacity to reach its goals with available materials).
3.Results
Search Results
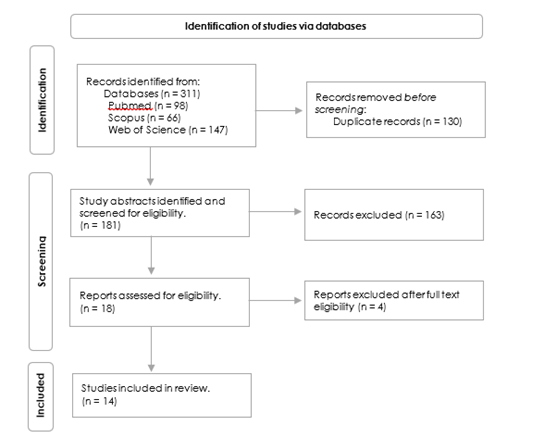
The initial results produced 311 papers; after removing duplicates, 181 remained. These were organized in a first stage standardized data tool (Supplementary material 1. Eligibility criteria filter) and reviewers (LSZ, MFMT) manually assessed abstracts to determine inclusion independently, disagreement were resolved by a third author (MMBG); 163 papers were excluded. Study quality was also assessed in this stage, based on the clarity of the study's objective, the cohesion and coherence between methodology, results and discussion, and the contribution of the research. Four articles were excluded during the full reading stage because of their methodology (Hendriks et al., 2020; Kaspar et al., 2021; Mtuy et al., 2022). The PRISMA flowchart (Figure 1) summarizes the process.
Cultural Adaptation Overview
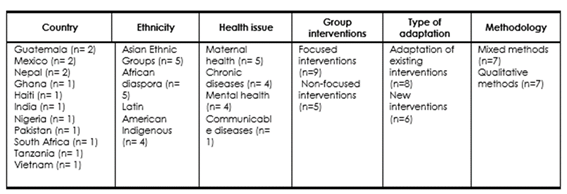
14 articles selected (See Table 1). All of them were in English and the interventions were held in Asia (36%), the Americas (36%), and Africa (28%); they were aimed for Asian Ethnic Groups, African Diaspora communities (n= 5 each), and Latin American Indigenous groups (n= 4).
The reviewed studies allowed the identification of two types of cultural adaptation of health interventions. Eight studies presented an adaptation of pre-existing evidence-based interventions: five programs, one detection tool, one interview model, and one therapy manual were adapted. Six studies presented new interventions co-created with the participants adapted to the cultural context.
All interventions, except one, had a focused approach: three interventions focused on disease; two focused on adolescents; four focused on traditional health workers; and four focused on women. The health issues addressed by these cultural adaptations were Maternal health (36%), chronic diseases (29%), mental health (29%), and communicable diseases (7%).
The results suggest that cultural adaptations have two main functions: nine interventions about behavioral changes to improve health outcomes and three interventions about health education were found. In addition, three studies with other functions were found, one study aimed to provide access to a specific health service, and one study aimed to improve the detection of a health problem. While there were interventions entirely aimed at health education, all the interventions had this component to some degree, involving either the local providers, or the program’s recipients.
In terms of methodology, seven studies used mixed methods, including pragmatic cluster randomized controlled trials and community-led randomized trials, which measured effectiveness by comparing the clinical outcomes with and without interventions. Seven studies used qualitative methodology, four were based on conducting focus groups and interviews and, usually, their goal was to assess the knowledge, beliefs, and practices of participants, and three were done through participatory research which implied a deeper involvement of the participants.
The information reported on the adaptations varied, five studies only proposed a design for an adaptation; four studies included the design and implementation; three studies presented the whole process including design, implementation, and evaluation; and two studies presented the results of the evaluation.
Design of Cultural Adaptation
The cultural adaptation design had three key components. First is participation, all 14 studies have a participatory component, although, they have different levels of community participation involving a diverse range of stakeholders. Eight studies showed a medium level of community participation (Fisher, et al. 2014; Mohsin, et al., 2021; Lamptey, et al., 2022; Loganathan & Varghese, 2019; Maar, et al., 2016; Rose-Clarke, et al, 2020; Sarmieto, et al, 2022; Zubieta, et al, 2020) which means that community was actively involved in at least one stage of the intervention: five of them report complex co-design processes, mainly with participation in content adaptation, and three reported community participation only in the need identification stage, the implementation stage, or evaluation stage respectively. A high level of community participation was reported in five interventions (Catley, et al., 2019; Chomat, et al., 2019; Cockcroft, et al., 2022; Orrego Dunleavy, 2020; Sarmiento, et al., 2020), which means that community involvement was present in all the stages of the intervention: needs identification, design, implementation, and evaluation. In all cases, participation is a key component of cultural adaptation to achieve the study objectives, but it also had an impact that went beyond health matters, it contributed to community agency. Only a study had a low level of community participation (Rimal, et al., 2021), which means there was limited involvement in one stage, but most of the study was created and implemented by the research team.
The second factor is the adaptation of content, reported in 12 of the reviewed studies. The remaining two articles, which correspond to only one study, do not report on content adaptation, but they are likely to have included it in the early stages of implementation. The adaptations of content were classified in surface-structure and deep-structure adaptations (Resnicow et al., 1999). All of the 12 studies reported surface-structure adaptations (Catley, et al., 2019; Chomat, et al., 2019; Cockcroft, et al., 2022 ; Fisher, et al. 2014; Lamptey, et al., 2022; Loganathan & Varghese, 2019; Mohsin, et al., 2021; Maar, et al., 2016; Orrego Dunleavy, 2020; Rimal, et al., 2021; Rose-Clarke, et al, 2020; Zubieta, et al, 2020), which matched materials or messages to observable superficial characteristics of the target population related to (i) the translation to the native language and the inclusion of bilingual delivery agents; (ii) the use of art-based methods (audiovisual content, local soap operas, street play), easily recognizable images (illustration, draws, communication material), cognitive exercise (games, maps, comparison, discussion) and communication elements (colloquialisms, idioms, metaphors, analogies); and (iii) the incorporation of local, frequently consumed foods and typical dishes into the programs. Eight of the 12 studies also reported deep-structure adaptations (Catley,et al., 2019; Chomat, et al., 2019; Fisher, et al. 2014; Lamptey, et al., 2022; Maar, et al., 2016; Mohsin, et al., 2021; Rose-Clarke, et al, 2020; Zubieta, et al, 2020), which addressed cultural, ethnic, historical, social or environmental factors that may influence health behaviors through person centered interventions which take into account economic characteristics, literacy and numeracy levels, traditional gender roles and the family and community influence; some of them took into account socio-cultural factors for the design, such as customs, traditions and belief of the population, and others focused in modification of cultural practices and behaviors of population that impact the health.
The third factor is changes in service delivery, which was present in 11 studies, and it was always joined with adaptations to the content and the community participation (Catley, et al., 2019; Fisher, et al. 2014; Lamptey, et al., 2022; Loganathan & Varghese, 2019; Maar, et al., 2016; Orrego Dunleavy, 2020; Rimal, et al., 2021; Rose-Clarke, et al, 2020; Sarmiento, et al., 2020; Sarmieto, et al, 2022; Zubieta, et al, 2020. The proposed changes were related to (i)adaptations to the methodology of services delivery, such as change in place and time where the services were offered; (ii) changes in service provider, such as shifting to include midwives ; (iii) changes in the mechanism of service delivery, which meant the inclusion of a range of pedagogical, artistic, audiovisual and virtual tools ; (iv)modifications of the implementation approach, for example focusing on the exchange of knowledge between ancestral and western medicine to improve the health outcomes.
3.4.Implementation Process
Four groups of barriers for the implementation of cultural adaptations were identified (i) Barriers that decrease participation, including barriers linked to lack of access to economic resources, namely low incomes, which were identified in four studies (Catley et al., 2022; Maar et al., 2016; Orrego Dunleavy, 2020; Rose-Clarke et al., 2020); as well as cultural barriers such as fear of stigmatization and discrimination mentioned in seven studies (Fisher et al., 2014; Loganathan & Varghese, 2019; Maar et al., 2016; Orrego Dunleavy, 2020; Rose-Clarke et al., 2020; Sarmiento et al., 2020, 2022) and women’s childcare responsibilities and their lack of autonomy mentioned in two studies (Chomat et al., 2019; Rimal et al., 2021). (ii) Barriers that limit the fidelity of the interventions. Including barriers linked to the lack of access to resources such as fresh food or crowded living conditions, which were mentioned in four studies (Catley et al., 2022; Maar et al., 2016; Orrego Dunleavy, 2020; Rose-Clarke et al., 2020) and can prevent the implementation of specific elements of the interventions (e.g. healthy diets or natural ventilation). (iii) Barriers that negatively impact the reliability of the delivery, such as educational barriers, which were identified in three studies (Chomat et al., 2019; Loganathan & Varghese, 2019; Orrego Dunleavy, 2020), and include lower literacy levels, lack of fluency in a language, and lack of health knowledge; which can have a negative impact on the comprehension of the participants. (iv) Barriers that increase the cost and time of an intervention, including barriers related to national health systems, which were stated in four studies (Maar et al., 2016; Sarmiento et al., 2020, 2022; Zubieta et al., 2020) and refer to a lack of access to services and health care facilities, and the unsustainability of care due to few health professionals and dependency on international funding.
Five groups of facilitators for the implementation process were identified. (i) Facilitators linked to coordinated work with local institutions, which are mentioned in seven studies (Catley et al., 2022; Chomat et al., 2019; Fisher et al., 2014; Lamptey et al., 2022; Mohsin et al., 2021; Orrego Dunleavy, 2020; Rimal et al., 2021). This refers to the use of the facilities of local institutions and the involvement and training of local health workers or volunteers, which can decrease the cost of interventions. (ii) Facilitators linked to the relationship between the research team and participants, which appeared in three studies (Loganathan & Varghese, 2019; Sarmiento et al., 2020, 2022), and it includes good communication as well as empathy and commitment from the research team. This contributes to the constant adjustment of the intervention, making it more effective and improving acceptability. (iii) Facilitators that respond to logistical changes, which were mentioned in three studies (Fisher et al., 2014; Rose-Clarke et al., 2020; Zubieta et al., 2020). This refers to having as few meetings as possible, making them short and avoiding scheduling them during important community events, which can increase participant drop out. (iv) Facilitators linked to the inclusion of traditional medicine and other cultural characteristics, which were mentioned in five studies (Loganathan & Varghese, 2019; Maar et al., 2016; Orrego Dunleavy, 2020; Sarmiento et al., 2020, 2022). This refers to recognizing the capability of traditional health practitioners to engage the community, respecting indigenous skills, avoiding the stigmatization of traditional practitioners, and incorporating healthy traditional diets and some cultural non-sedentary habits, which can improve the community participation and acceptability of the interventions.
3.5.Outcomes of Cultural Adaptation
All studies stated that positive outcomes were achieved. Out of the 14 studies, 10 reported only one main outcome, and four mentioned two or three outcomes. Acceptability is the most frequently reported outcome. Eight studies (Chomat et al., 2019; Fisher et al., 2014; Orrego Dunleavy, 2020; Rimal et al., 2021; Sarmiento et al., 2022; Rose-Clarke et al., 2020; Zubieta et al., 2020) mentioned that the participants considered the cultural adaptation a satisfactory, comfortable, and interesting intervention, and they saw the high value of the project. The high acceptability contributed to improving health literacy and the participant’s motivation in the adoption of good health practices, as well as it led to the inclusion of new approaches to health to solve traditional health problems.
Effectiveness is mentioned directly in five studies (Catley et al., 2022; Chomat et al., 2019; Maar et al., 2016; Mohsin et al., 2021; Rimal et al., 2021), usually it refers to the achievement of the implementation’s objectives to address the health issue in a complex context. For instance, the identification of mediators to monitor and care for hypertension in rural and aboriginal populations. In other cases, the studies mention the effectiveness of the participatory approach to promote behavioral change, to address sexual and reproductive health in conservative cultures, or promote healthy lifestyle to control diabetes in low-income countries.
Feasibility is reported in five pilot projects (Cockcroft et al, 2022; Orrego Dunleavy, 2020; Rose-Clarke et al., 2020; Sarmiento et al., 2020; Zubieta et al., 2020, which reported that the implementation strategies are useful, adequate, or appropriate for the context and population. For example, a psychosocial intervention is feasible to improve the perinatal mental health for indigenous women in Guatemala, or a participatory multistage process is useful for adolescents with depression in rural Nepal.
Knowledge about a disease was the direct outcome in four studies which were educational programs (Fisher et al., 2014; Lamptey et al., 2022; Loganathan & Varghese, 2019; 2022; Orrego Dunleavy, 2020), however, all 14 studies mentioned an educational component. The above studies mention that the cultural adaptation facilitates the understanding and comprehensiveness of educational programs for population with specific learning needs, for example: low numeracy, low literacy, low resource settings, or with communicational barriers. The achievement of knowledge about diseases often increased the knowledge over transmission, stigma reduction, treatment, and prevention of different diseases such as HIV, diabetes and mental health diseases.
Furthermore, the studies reported other outcomes beyond health which are difficult to measure, such as social empowerment, as well as the positive influence of the empathy and social networks between participants and researchers. In addition, the studies state the cultural competency of researcher team and health workers is required for the cultural adaptation. Likewise, the challenge of the replicability of the implementation was mentioned, since, although the findings are generalizable for complex populations with similar settings and context, adaptation to the context are always necessary.
4.Discussion
4.1Using Cultural Adaptation
Cultural adaptations have different scopes according to the project objective, the main ones are health education and promotion of behavioral change. These adaptations can occur at the surface-structure level (Resnicow et al., 1999) when interventions focus on health education. They might involve using new pedagogical tools or translating content into the native language, and their objective is to ensure participants' comprehension. When the aim is to achieve behavioral change, the cultural adaptations are at the deep-structure level (Resnicow et al., 1999), which requires deep contextual knowledge, investigating the cultural factors that influence the inadequate practices in health, and the design of a new approach with innovative methods to solve the health issue. Similar findings have been reported in a systematic review by Tawankanjanachot et al. (2023) which found that adapting social skills interventions with adolescents with autism in Asian cultures require understanding the social context of the local culture, and the cultural characteristics of participants to modify the intervention’s content and structure and improve its effectiveness.
Likewise, the studies show different scopes according to the design of the study. In the mixed methods studies, experimental methods are used for measuring the effectiveness through the change in clinical outcomes, and the acceptability through focus groups. In the qualitative studies the cultural adaptation is based on a deeper comprehension of practices, attitudes, and knowledge, which allow the improvement of the intervention’s appropriateness according to the context and the recipients, usually they measure the acceptability, knowledge disease and feasibility.
In both cases, cultural adaptation includes a social diagnostic of the social and health context, using ethnographic techniques and surveys, while in the design and implementation the participatory approach involving local leaders, integrating traditional medicine, as well as the use of audiovisual tools are key factors. The triangulation of methods can be considered as a quality factor of the selected studies, since they integrate the comprehensive analysis of factors involved in health behavior provided by a qualitative approach, with the precision and sample size of experimental or quantitative studies.
In addition, some studies have pointed out the lack of replicability of culturally adapted interventions as a limitation. However, this is not a limitation of cultural adaptation itself, but a characteristic of social and qualitative research. When dealing with human behavior and social processes, it is impossible to replicate them entirely, due to the numerous uncontrolled factors involved. In this sense, social and qualitative research, where cultural adaptation is subscribed, holds significant value in its applicability. It enables the abstraction of models, processes and theoretical schemes that can be applied in other similar contexts, with basic adaptations that guarantee their appropriateness and suitability.
4.2Design and implementation of Culturally Adapted Interventions
Design is crucial in the development of cultural adaptations. All studies propose a person-centered design, based on in-depth knowledge of the context. In the design, all studies include a participatory approach and content adaptation based on socio-cultural features of the recipient population, and 11 of 14 studies included changes in service delivery, to mitigate the contextual factors that could became implementation barriers. The most complex designs include these three factors, highlighting a strong participatory approach as a co-design process involving a diverse range of stakeholders in all stages of intervention.
Regarding the implementation, the description of the process and the analysis of barriers suggest that cultural adaptation projects are complex interventions. First, the cultural adaptation addresses cultural issues, which in themselves are complex processes to intervene in, because all of them are historically anchored, and require time and join efforts from different instances such as educational systems, policies, etc. In addition, the vulnerability of population affects the fidelity and reliability of implementation, as it was also noted by Naderbagi et al. (2024) in their systematic review of cultural adapted digital health interventions, which found that barriers to digital sources due to limited technological knowledge, mobile data costs, and the lack of devices are contextual barriers for the interventions. Moreover, the barriers related to the health system can affect the efficiency of implementation and may hamper sustainability (Bautista-Gomez et al., 2022).
Despite this, there is a range of key facilitators. One of them is the knowledge exchange between the empirical knowledge of local leaders and the technical knowledge of researchers and practitioners, but also the exchange between traditional health knowledge and Western medicine.
Another facilitator is the involvement of the ancestral physicians, midwives, and other local leaders, who can contribute to the effectiveness with their health knowledge, to community engagement through an empirical cultural approach and to increase the trust and confidence of the participants in the project. Furthermore, several studies mention the importance of the integration of projects with local institutions and health workers, to facilitate the logistic of intervention, and its sustainability.
4.3Contribution of Cultural Adaptation
The main contribution of cultural adaptation is the generation of evidence to improve effectiveness and increase acceptability in health interventions in complex contexts (Bernal et al., 2009). The first key to achieve this is the design of an appropriate health intervention for the context and population based on a participatory approach. The importance of the participatory approach as one of the first steps of adaptation is in line with the finding reported by Venner et al. (2022) in their systematic review of cultural adaptation of substance use disorder treatments across Latinx communities. This first key aspect leads to overcoming challenges often faced by generic interventions where contextual and cultural barriers can limit their effectiveness, or where the traditional methods of interventions have not solved recurring health problems.
The second key is the people-centered approach (WHO, 2007). Cultural adaptation puts emphasis on the different people involved in the project. Evidently, the main actors are the recipient communities, for this reason, the intervention is designed based on their life practices and interests to integrate the project in the social context in the least disruptive manner. But also, the studies attribute an important value to the relationship between research team, health workers, and community leaders; factors such as empathy, commitment, and cultural competence play an important role in the creation of trust relationships.
A third key is innovation, which refers to new ways to solve traditional health problems. It can be through task shifting, an interdisciplinary approach integrating social and biomedical science, innovative artistic and communicational tools, and a range of cultural expressions. Cultural adaptation uses innovation to facilitate education, but especially to motivate change through sensitization and awareness raising.
There is a relationship between these three factors and the main components of the behavioral change COMB-B model (Michie et al., 2011), which are capacity, opportunity, and motivation. The appropriateness to the context of the cultural adaptation can have a positive effect on the opportunity because it facilitates participation, makes logistical adjustments and tries to achieve sustainability. The person-centered approach builds capacity in the community, increasing their health literacy seeks to improve their life conditions beyond health. Motivation, on the other hand, plays a crucial role in behavioral change, because even if the necessary conditions for change are in place, and an effective health education process has been conducted, without motivation behavioral change is not possible. For this reason, the cultural adaptation uses innovative tools to motivate the will to change. With these three components of behavioral change, cultural adaptation can contribute to it with the capacity and motivation, while the opportunity is more complex because there are a lot of not controlled factors that condition the opportunities to change.
5.Conclusion
The cultural adaptation with ethnic groups in vulnerable settings is useful to ensure comprehensive health education and to promote behavioral change using qualitative methods for the content adaptation based on the analysis of knowledge, beliefs, and cultural practices, as well as a participatory approach using innovative tools for the co-design process. Its main contribution is the generation of evidence to improve effectiveness and increase acceptability in health implementations in complex contexts through the attributes of appropriateness, people-centered approach, and innovation. Its main limitations are the fidelity and reliability of the implementation, both affected by contextual factors.