Introduction
Hidradenitis suppurativa (HS) is a chronic inflammatory condition that involves apocrine glands and hair follicles in intertriginous regions, such as inguinal, axillary, genital, perineal, and perianal areas [1]. The pathogenesis of HS remains incompletely understood, but three key processes have been implicated: follicular hyperkeratosis and dilatation, follicular rupture with subsequent inflammatory response, and chronic inflammation with architectural tissue changes [2]. Several inflammatory cytokines, such as tumor necrosis factor (TNF), interferon-γ, interleukin (IL)-10, IL-12, IL-17, IL-23, and IL-32, as well as antimicrobial peptides LL-37, psoriasin, and β-defensins 2 and 3, may have a role in the development of the disease [3]. The etiologic role of genetic, hormonal, and environmental factors is not completely established [2].
As a systemic inflammatory disease, HS is associated with multiple comorbidities including metabolic, cardiovascular, endocrine, gastrointestinal, rheumatic, and psychiatric disorders [1]. In this setting, the relationship with neoplastic disorders may be a new area of research, in which the chronic inflammatory state and the increased immune activation in HS can trigger the development of lymphoma [1].
Case Report
A 72-year-old male with a 30-year history of HS was referred to our center due to severe perianal involvement. Past medical and surgical history included multiple antibiotic courses, percutaneous drainage of abscesses, and three fistulotomies. After exclusion of inflammatory bowel disease, namely, Crohn’s disease (normal findings in endoscopy, histology, and enterography), combination therapy with an anti-TNF was considered. At the time, although only a few cases of infliximab in HS were described, we decided to start it due to our center’s vast experience with this drug in aggressive perianal Crohn’s disease. Since the patient was a male above the age of 65 years, considering the risks of combining an anti-TNF with thiopurines in this subgroup, we opted for methotrexate to prevent immunogenicity and improve drug levels. Clinical remission was achieved.
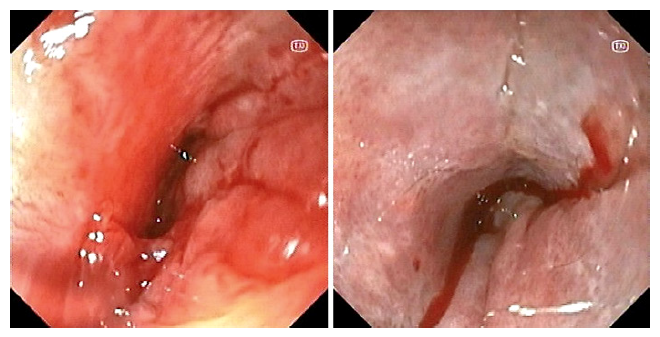
Four years later, he presented with a 3-month course of intense proctalgia, purulent perianal exudation, and fever without a specific pattern, refractory to oral and intravenous antibiotics. Apart from a mild leukocytosis (13.960 G/L) and an increase in C-reactive protein (72.3 mg/L), other laboratory studies, such as complete blood count, erythrocyte sedimentation rate, renal and hepatic function tests, lactate dehydrogenase, and creatinine kinase, were unremarkable. Cytomegalovirus and Epstein-Barr virus (EBV) serologies were compatible with previous infection. Blood and stool cultures, stool ova and parasite test, and perianal exudate cultures were negative. Pelvic magnetic resonance imaging revealed diffuse thickening of the rectum, deep ulcerations in the lower rectum, intersphincteric fistulas (with one extending to the prostatic apex/base of the penis), and multifocal disruption of the sphincter planes (Fig. 1). He underwent proctological examination and colonoscopy, showing extensive circumferential ulceration involving the entire anal canal and the distal 3 cm of the rectum, with pseudopolypoid formations and several depressions, some with pus drainage, suggestive of fistula openings (Fig. 2). Histopathology demonstrated extensive ulceration of distal rectal and anal mucosa, along with infiltration by large and atypical lymphoid cells. The neoplastic cells were positive for CD20, BCL6, MUM-1, BCL2, and Epstein-Barr encoding region in situ hybridization and negative for CD3 and CD10. Ki-67 was estimated in 50%. These findings were consistent with EBV-positive diffuse large B-cell lymphoma (DLBCL) (Fig. 3). Additional investigation included a bone marrow biopsy and full-body computerized tomography scan, both without relevant findings. A diagnosis of stage IV non-Hodgkin DLBCL was made.
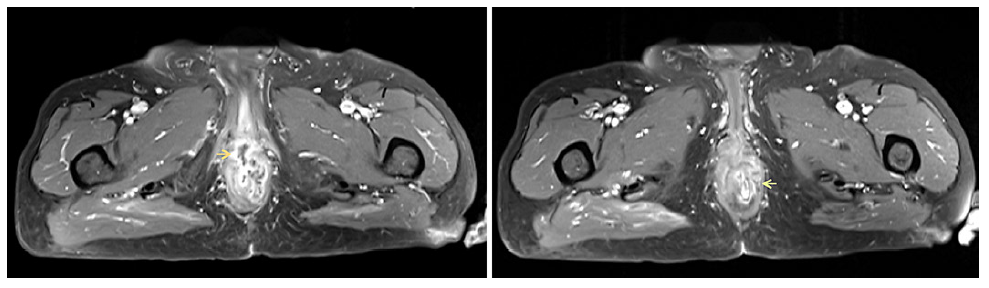
Fig. 1 Pelvic MRI (axial view, T1) revealing intersphincteric fistulas with one extending to the prostatic apex/base of the penis (orange arrow) and multifocal disruption of the sphincter planes (green arrow). MRI, magnetic resonance imaging.
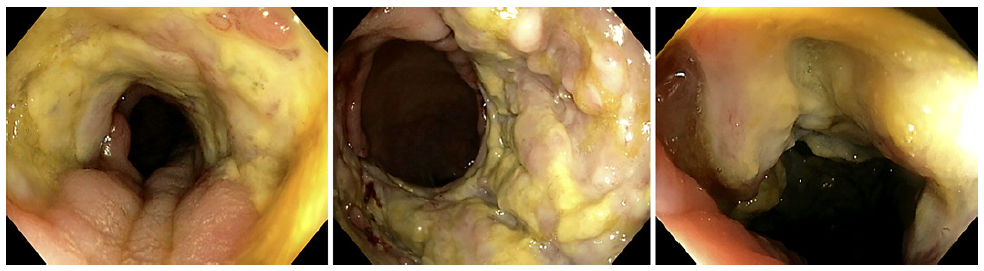
Fig. 2 Colonoscopy showing extensive circumferential ulceration involving the entire anal canal and the distal 3 cm of the rectum, with pseudopolypoid formations and several depressions, some with pus drainage, suggestive of fistula openings.
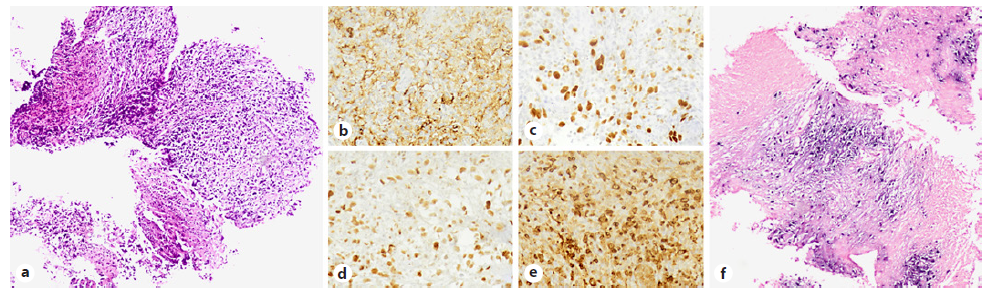
Fig. 3 Histopathology examination revealing rectal and anal mucosa with extensive ulceration and infiltration by large atypical lymphoid cells (hematoxylineosin [HE] ×100) (a). Neoplastic cells expressed CD20 (b), MUM-1 (c), BCL6 (d), and BCL2 (e) [×400]. EBER in situ hybridization revealed positive staining of the neoplastic cells (f) [×100]. EBER, Epstein-Barr encoding region.
After an expert multidisciplinary discussion, we decided to stop immunosuppression (MTX and infliximab); perform a colostomy in order to improve perianal sepsis and reduce the risk of infectious complications; and afterwards initiate immunochemotherapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone since he had no further comorbidities. Six cycles were performed with a complete response. Pelvic magnetic resonance imaging showed significant tumoral regression with some posttreatment inflammatory features and sustained anal canal and sphincter deformation. Reassessment rectosigmoidoscopy revealed a proximal anal canal stenosis with friable scar-like mucosa, which could not be overcome with the ultrathin endoscope (Fig. 4). Biopsies showed no evidence of lymphoma. Due to these findings, bowel transit reconstruction was not possible, and the patient remains with a colostomy.
Discussion/Conclusion
In the Western world, there has been an upward trend in the incidence of lymphoma in the past few decades, along with a parallel increase in the occurrence of inflammatory conditions treated with immunosuppressive agents [4]. Various studies have identified an increased risk of lymphoma among patients with several chronic inflammatory disorders [5, 6]. Persistent activation of the immune system may have a significant role in the genesis of lymphoproliferative disorders (LPD); chronic B-cell stimulation and proliferation, in particular, appear to have major roles [7]. With regard to HS, its association with lymphoma has recently been a topic of debate [2].
A case-control study showed a 2.03 greater odds of lymphoma in patients with HS relative to control individuals, although it was not statistically significant [8]. A recent cross-sectional study found that both males and females with HS were more likely to have LPD than the general population (odds ratio of 2.00 for non-Hodgkin and 2.26 for Hodgkin lymphoma), with male patients having a higher prevalence [9]. In another recent Korean nationwide population-based cohort study, patients with HS had an increased risk of Hodgkin’s lymphoma. However, in subgroup analysis, only male patients with HS had an increased risk. In addition, the risk of Hodgkin's lymphoma was greater in patients with moderate to severe HS than those with mild disease, suggesting that the risk of LPD may be related with disease severity [3].
In fact, despite the remaining uncertainties regarding the potential independent role of the disease itself in the pathogenesis of these LPD, the contribution of immunosuppressive therapy has been widely assessed in other diseases, such as rheumatoid arthritis or inflammatory bowel disease [1, 3, 7, 9-20]. LPD induced by MTX (MTX-LPD) are categorized as other iatrogenic immunodeficiency-associated LPD in the most recent edition of the World Health Organization's classification of hematopoietic and lymphoid tissue tumors, being described predominantly in patients with rheumatoid arthritis [21]. MTX-LPD consists mainly of DLBCL (35-60% of cases), and approximately 40-50% cases occur in extranodal sites, such as the skin, salivary glands, lungs, digestive tract, liver, and spine [21, 22]. Although spontaneous remission of MTX-LPD after MTX removal occurs in approximately 50% of cases, chemotherapy may be necessary [22]. The frequency of EBV infection is highly variable in these cases. The degree and duration of im-munosuppression, the degree of inflammation and/or chronic antigenic stimulation, as well as the patient’s genetic background play an important role in the development of EBV-positive LPD [23].
The potential effects of anti-TNF on malignancy are difficult to accurately predict, given the pleotropic effects of these inhibitors and the complexity of the pathways involved in inflammation and tumor development [10]. Although some recent studies have associated the use of anti-TNFα with an increased risk of LPD [11, 12], others did not find this relation, and apart from the case of hepatosplenic T-cell lymphoma for which anti-TNFα seems to enhance the deleterious effect of thiopurines [13], there is not enough evidence to claim that these agents may contribute to an increased LPD incidence [14-20].
To date, no study has specifically examined the general additional risk of LPD in patients with HS exposed to MTX or anti-TNFα. This case reinforces the concept that chronic inflammation is a very important pathway that leads to the development of LPD. The key point is that in the presence of severe disease presentation refractory to adequate treatment, reconsidering the patient’s initial diagnosis is mandatory. The possibility of LPD should be considered in these HS patients with long-standing active disease under immunosuppressive therapy. Further studies are necessary in order to assess the role of the disease itself and of immunosuppressive therapy in the development of LPD in patients with HS.