Introduction
Epithelioid hemangioendothelioma (EHE) is a very rare vascular neoplasm composed of epithelioid or histiocytoid cells with endothelial characteristics. EHE is usually diagnosed between 20 and 60 years, with a median onset of disease at the age of 36 [1, 2]. It is more common in women than in men, depending on the involved organ [3].
In the majority of these cases, EHE is multifocal or metastatic at diagnosis. EHE most frequently arises in the liver, followed by the lung and bones [4]. Presenting symptoms are often based on disease site: liver EHE may cause constitutional symptoms, nausea, abdominal pain, and jaundice. It may appear on computed tomography or magnetic resonance imaging as a solitary or multifocal mass [4].
The natural history of EHE is variable, ranging from indolent disease (similar to those with benign hemangiomas) to a more aggressive disease (similar to those with angiosarcoma). The majority of patients (50-76%) with EHE are asymptomatic at diagnosis, and the disease is incidentally detected during radiographic imaging [4]. Morphologically, EHE is characterized by epithelioid endothelial cells often organizing in strands and cords set in a collagenous stroma, and expressing endothelial differentiation markers, such as CD31, CD34, factor VIII-related antigen, ERG, and FLI-1 [5].
Case Report
The authors present the case of a 41-year-old female who underwent liver transplantation in 2003 due to symptomatic familial amyloidotic polyneuropathy (dysautonomia and sensory polyneuropathy), immunosuppressed with cyclosporine. In March 2013, a routine analytical study revealed a discreet cholestasis pattern, with alkaline phosphatase of 151 U/L and gamma-GT of 75 U/L. The patient remained asymptomatic.
Three months later, the patient maintained a worsening pattern of cholestasis despite the increase of immunosuppression. In abdominal ultrasound, some nonspecific liver lesions were described. A thoracoabdominopelvic computed tomography was, then, performed, showing several subcapsular hepatic lesions with hypovascular behavior, the largest with 43 mm and 23 mm (shown in Fig. 1a). In the lung parenchyma, several micronodular lesions dispersed throughout both lungs were mentioned, the largest with 3 mm (shown in Fig. 1b).
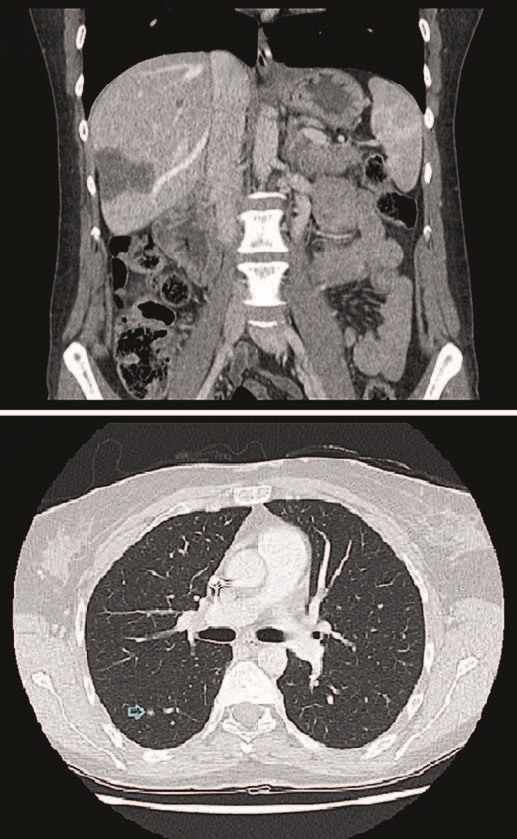
Fig. 1 a Several subcapsular hepatic lesions with hypovascular behavior, the largest with 43 mm and 23 mm. b Several micro-nodular lesions dispersed throughout both lungs’ parenchyma, the largest with 3 mm.
An ultrasound-guided biopsy was performed and the histological examination revealed a proliferative lesion with infiltrative growth, consisting of predominantly epithelioid, monomorphic cells, with abundant cytoplasm with formation of vascular lumens (shown in Fig. 2a). The immunohistochemical study showed immunoreactivity of neoplastic cells for CD31, CD34, and factor VIII, thus favoring the diagnostic hypothesis of EHE. Broncho-scopy was normal and cytology was negative for neoplastic cells. The dose of cyclosporine was reduced and everolimus was started at a dose of 0.5 mg twice daily. The donor’s medical record was reviewed: 20-year-old girl who’s died of traumatic brain injury, without abdominal trauma or known medical history and with a normal abdominal ultrasound.
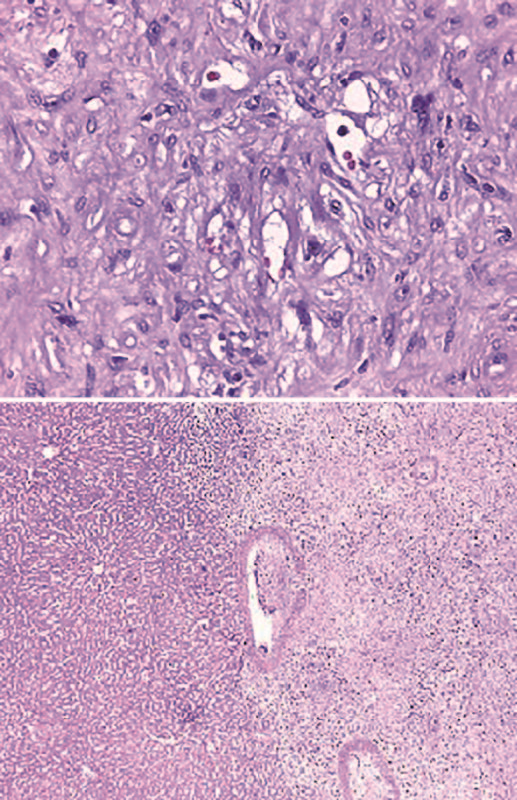
Fig. 2 a Proliferative lesion with infiltrative growth, consisting of predominantly epithelioid, monomorphic cells, with abundant cytoplasm with formation of vascular lumens. b Neoplasm of infiltrative borders constituted by fibromyxoid stroma whit spindle and epithelioid cells with moderate atypia.
Throughout the 6-month follow-up, there was progression of liver lesions with dimensional stability of pulmonary micro-nodules, and graft function remained stable. After a multidisciplinary discussion, liver re-transplantation was decided, which was carried out in July 2014. Immunosuppression was restarted with tacrolimus, mycophenolate mofetil, and corticosteroids, and 2 months later everolimus was restarted, with progressive suspension of mycophenolate mofetil and corticosteroids.
The histological analysis of the explant showed a neoplasm of infiltrative borders constituted by fibromyxoid stroma whit spindle and epithelioid cells, moderate atypia, low mitotic index, and no necrosis, compatible with EHE (shown in Fig. 2b). Images suggestive of vascular invasion were also identified. After 8 years of follow-up, the patient is clinically stable, with no graft dysfunction, no neoplastic recurrence, and dimensional stability of the pulmonary micronodules.
Discussion
Compared with general population, patients with organ transplant have higher risk of developing carcinoma by 2.6 times [6]. The development of cancer is a multi-factorial process. The effective immune system recognizes and attempts to eliminate primary tumors via cytotoxic T lymphocytes, macrophages, and natural killer cells, which can recognize tumor cells as nonself cells, delay tumor progression, and prevent angiogenesis, vascular infiltration, and metastasis [7]. The transmission of malignant tumors by donors, long-term exposure to risk factors, or potential carcinogenesis like the growth of age may be the inducing factors of tumors [8].
Therefore, the tumors of liver transplant recipients can be divided into four types: donor transmission cancer, donor-derived carcinoma, new cancer, and recurrent cancer [9]. In this particular patient, it is difficult to know if it is a donor-derived tumor or a new cancer.
In liver transplant recipients, minimization/modification of immunosuppression may be a key component of cancer prevention because the effect of immunosuppression on carcinogenesis seems to be dose-dependent [10]. However, the risk of rejection and the benefits of cancer prevention need to be carefully weighed. Sirolimus and everolimus have potential antiproliferative properties and are considered to inhibit tumor growth, reducing the risk of death in transplant recipients with de novo malignancies by76%[11].
Although some factors are believed to play a role in the etiology of hepatic EHE (alcohol consumption, asbestosis, oral contraceptive use), the reason for the onset of the disease is still unknown [1]. About 90% of all EHE have a t(1; 3) (p36; q25) translocation, resulting in the fusion gene WWTR1-CAMTA1 with high CAMTA1 activity [3]. The WWTR1-CAMTA1 rearrangement is a genetic hallmark of EHE and is not found in other vascular tumors [3]. In our patient, it was not possible to carry out the genetic test, so the diagnosis was made taking into account the immunohistochemical study, histological, and imaging characteristics.
No standard treatment strategy has been defined yet. Assumed the possible curative impact of local treatments and the risk of locoregional and/or systemic progression of EHE, at this state of knowledge, a prolonged watchful waiting policy for unifocal EHE is not suggested. Active surveillance should be considered only for patients who are not surgical candidates due to the presence of comorbidities or technical challenges [12].
Complete surgical resection is offered to patients with unifocal disease or disease limited to a few organs where surgery would not be overly morbid. Patients with unresectable disease that is symptomatic and/or progressive should be evaluated for orthotopic liver transplantation [13].
Unlike many other cancers, transplantation is a good option in metastatic disease. Limited and stable preexisting extrahepatic disease and lymph node invasion are not contraindications, as they do not appear to influence the prognosis nor have a negative impact on overall survival [13]. That said, despite not being 100% certain that it was a pulmonary metastatic disease, it was decided to go ahead with liver re-transplantation since the presence of pulmonary metastasis would not influence this therapeutic option. Long-term outcomes are excellent with transplant, with 10-year survival rates of approximately 74% [14].
Risk factors for EHE recurrence after transplant were pathologic evidence of macrovascular invasion, a waiting time from diagnosis to transplantation of less than 120 days, and involvement of hilar lymph nodes [14]. Longer waiting times from diagnosis to transplantation seem to be associated with a lower risk of recurrence, perhaps because of the more careful selection of patients with a better prognosis. According to Lerut et al. [15], 23.7% of patients undergoing liver transplantation (mean follow-up of 78.5 months) experienced recurrence of EHE.
Given the very limited activity of conventional chemotherapy in this disease and the absence of data suggesting a potential advantage in survival, neoadjuvant or adjuvant medical treatments are not recommended [16]. To our knowledge, this was the first case reported in the literature of an EHE of a liver transplant recipient effectively treated with liver re-transplantation.















