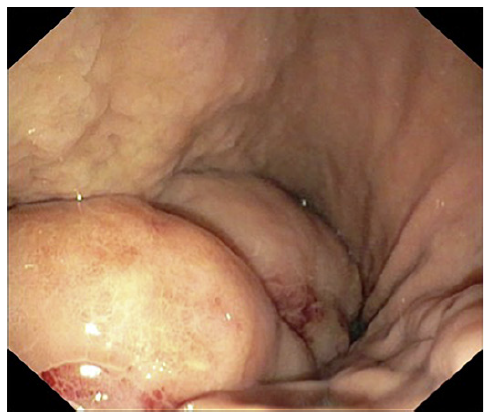
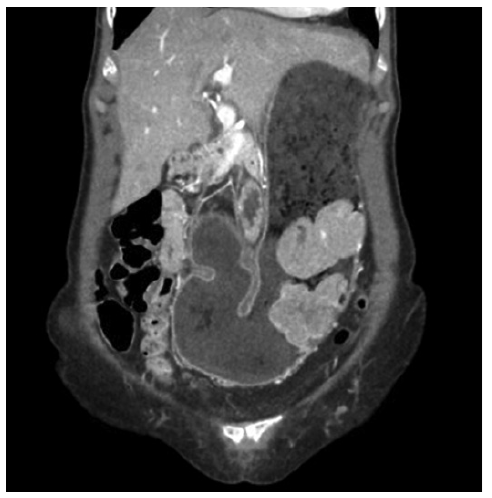
We present a 71-year-old female with no relevant past medical history. The patient was started on a proton pump inhibitor for dyspepsia, with complete symptomatic improvement. One year later, there was symptom recurrence with weight loss. Upper endoscopy revealed a 10 cm gastric subepithelial lesion, with central erosion (Fig. 1). Pathology evaluation was negative for malignancy. Computed tomography showed an extensive gastric wall lesion, with no adenopathies (Fig. 2). Endoscopic ultrasound (EUS) evaluation revealed an 8 cm subepithelial polycyclic hypoechoic lesion, with transition zone suggestive of the third/fourth layer origin (Fig. 3a). Quantitative elastography evaluation showed strain histogram 68 (Fig. 3b). The fine needle biopsy using a 22-G Franseen needle revealed clonal proliferation of plasma cells, positive for CD45/CD138 and negative for CD3/CD20/CD56 (Fig. 4). There was no anemia, hypercalcemia, or kidney impairment, and no abnormalities were found on bone marrow biopsy and myelogram apart from mildly increased plasma cell proliferation (5-10% of total cells). The positron emission tomography/computed tomography scan showed increased gastric uptake, with a maximum standardized uptake value of 3.3. Treatment consisted of surgical resection and the patient had an uneventful postoperative course. The surgical specimen confirmed the diagnosis.
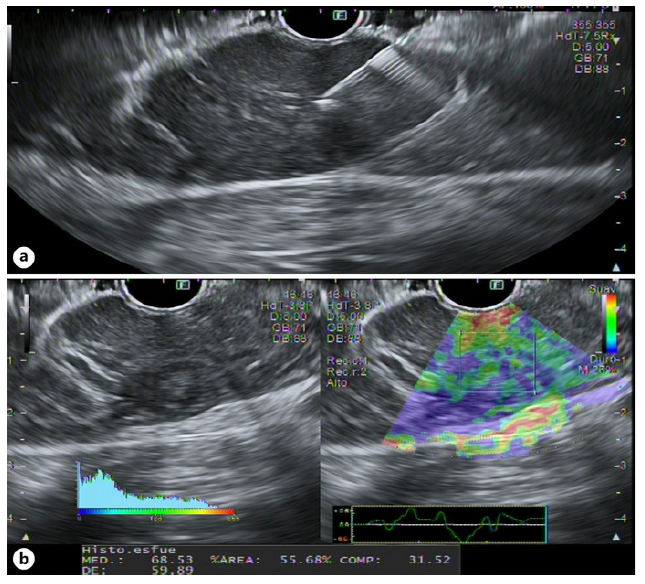
Fig. 3 EUS showing an 8-cm subepithelial polycyclic hypoecoid lesion, with transition zone suggestive of the third/fourth layer origin (a). Quantitative elastography eval-uation showed strain histogram 68 (b).
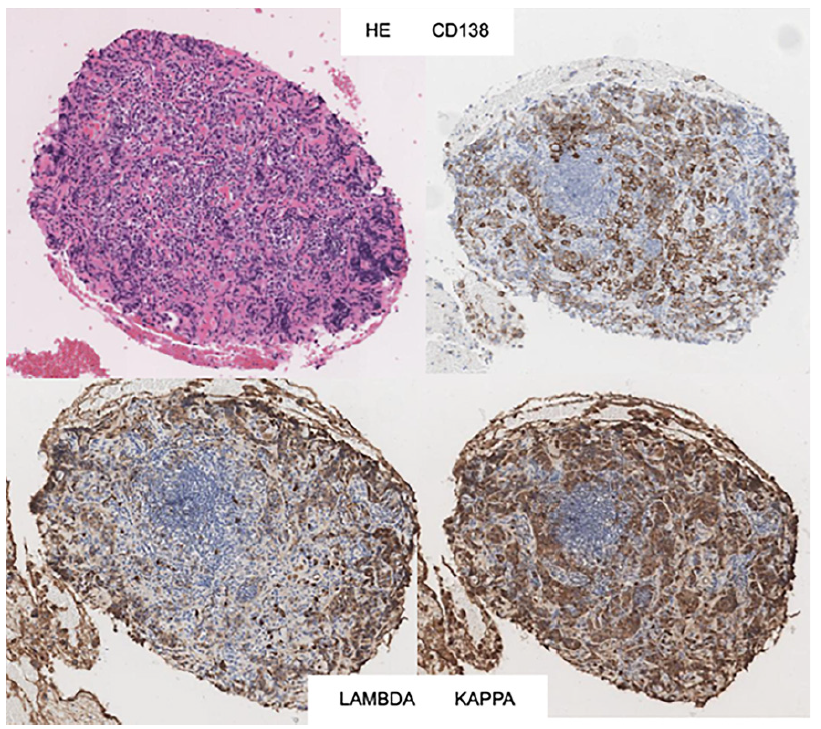
Fig. 4 Histopathology examination showing clonal proliferation of plasma cells, positive for CD45/CD138 and negative for CD3/CD20/CD56.
Solitary extramedullary plasmacytomas are plasma cell tumors arising outside of the bone marrow, accounting for approximately 3% of plasma cell malignancies [1]. Within this category, gastric plasmacytoma accounts for less than 2% of extramedullary plasmacytomas [2]. They frequently present as solitary lesions, although sometimes the endoscopic appearance can only reveal erosion of the mucosa [3]. Symptoms are nonspecific, with epigastric discomfort, abdominal pain, nausea, and vomiting commonly reported. Diagnosis requires biopsy-proven extramedullary tumor with evidence of clonal plasma cells, with flow cytometry immunophenotyping assuming a major role in most hematologic malignancies, along with normal skeletal and bone marrow survey and the absence of endorgan damage attributable to the underlying plasma cell disorder [4]. The role of EUS is not standardized, and data are scarce regarding EUS features of a gastric plasmacytoma [5]. Surgery is usually the treatment of choice, with a good prognosis [6]. The authors highlight the EUS role as part of the diagnostic workup of gastric plasmacytoma, a rare clinical entity.