Introduction
Vitiligo is an acquired disorder of pigmentation of the skin characterized by depigmented macules and patches as a result of the loss of melanocytes in the epidermis. The disease can affect any age, gender, or ethnicity but has a significant psychosocial impact, especially in those with higher skin phototype1. The distinctive feature of vitiligo is widespread cutaneous and mucosal depigmentation, which is linked to genetics, autoimmunity, oxidative stress, melanocyte self-destruction, and the release of cytokines2. Vitiligo is categorized into two primary forms based on clinical criteria, namely, segmental vitiligo, and non-segmental vitiligo, with the latter encompassing various subtypes such as generalized vitiligo, acrofacial vitiligo, and universal vitiligo3. The stability of vitiligo holds crucial importance for treatment approaches and prognosis, thus garnering significant attention in research and clinical practice4. Although the ideal length of time for the disease to be considered stable clinically is still debatable, the general consensus recommends a time period of the past 1 year of a patient having no new lesions, no progression of the existing lesions, and absence of Koebnerization for labeling a case as stable vitiligo5. Koebner’s phenomenon is an important aspect in determining whether surgical or invasive treatments are suitable for vitiligo cases, making the stability of the disease a critical aspect in its management.
Although numerous topical and systemic modalities of treatment are available, there is still a search for the ideal therapeutic modality since the response to treatment is not much satisfactory6.
Narrow-band ultraviolet B (NB-UVB) therapy, implemented since 1997, has emerged as one of the most effective and safest therapies for the treatment7,8. The light source used for NB-UVB phototherapy has a peak emission at 311 nm and is very effective in vitiligo since it can stimulate the dormant skin melanocytes and also modulate the cutaneous immune system9.
Fractional carbon dioxide laser (CO2) functions through fractional thermolysis, and it is suggested to enhance vitiligo treatment by reducing the affected area by causing shrinkage of the tissue, encouraging melanoblast migration from surrounding healthy skin, and promoting post-inflammatory pigmentation10-12.
Even though the precise etiology of the disease is yet unknown, it is well established that the pathophysiology of the disease is significantly influenced by the absence of basic fibroblast growth factor (bFGF) as the patients have been proven to have reduced bFGF mRNA expression in the lesions13. Thus, melanocyte growth and migration are facilitated by bFGF through a variety of signaling mechanisms and hence finds the role of bFGF-related decapeptide 0.1% in the treatment of vitiligo.
The melanocyte growth factor deprivation theory serves as the foundation for the decapeptide therapy of vitiligo, and the clinical data from Indian clinical studies substantiates the use of decapeptide as a medication for vitiligo management14.
The present study investigated the effect of a novel combination therapy involving NB-UVB phototherapy, bFGF-related decapeptide 0.1%, and fractional CO2 laser in the management of stable cases of non-segmental vitiligo and aims to provide novel insights into the treatment of the disease.
Materials and methods
The study was conducted after taking approval from the institutional ethical committee. All patients of clinically stable, non-segmental vitiligo attending Dermatology outpatient department of a tertiary care hospital from March 2023 to May 2023 were recruited in this prospective, interventional study after taking informed consent (from guardians in case of minors). Study subjects were selected based on the inclusion and exclusion criteria. A brief history along with details of any previous treatment taken was documented and confidentiality of the patients was ensured.
Exclusion criteria
The following criteria were excluded from the study:
− Patients with active Koebner’s phenomenon.
− Patients with mucosal vitiligo.
− Patients with active inflammation, infection, or ulcer in or around the vitiligo lesion.
− Females who are pregnant or are planning pregnancy; lactating mothers.
− Immunosuppressed patients, patients with chronic inflammatory diseases, systemic lupus erythematosus, xeroderma pigmentosa, and history of skin cancer.
Data analysis
The data were analyzed using Statistical Package for the Social Sciences version 23.0 software (SPSS Inc., Chicago, IL, USA for Windows), and valid conclusions were drawn by using the Chi-square test. P < 0.05 was considered statistically significant.
Procedure
Photographs were taken for the record before starting the procedure, at every session, and then during follow-up. Patients were exposed to NB-UVB chamber starting from 200 mJ/cm2 regardless of the skin phenotype, and an increment of 10-20% dose per session was done till a minimal erythema dose was achieved (pink, asymptomatic erythema lasting < 24 h). Two such sessions were done per week. Along with this, patients were asked to apply 1 mg/mL of bFGF-related decapeptide once every day, 2 h before bedtime. The lesions were exposed to fractional carbon dioxide laser at every 4 weekly interval @ 50 mJ energy and 100-200 spots/cm2 spot density according to the size of the lesion, after achieving anesthesia with topical anesthetic cream containing 2.5% prilocaine and 2.5% lidocaine. The laser was done before the NB-UVB exposure and an area of around 2 mm beyond the lesion was exposed. Four such sessions of fractional CO2 laser were carried out. Duration of therapy was 16 weeks and assessment of the patient was done at every 4-week interval using a quartile grading scale.
Results
A total of 22 patients met the inclusion-exclusion criteria during the stipulated time period and were enrolled in the study; however, two patients were lost to follow-up and hence were excluded from the study. Among these 20 patients, 8 (40%) were males and 12 (60%) were females (Fig. 1). The most common age group seen was 29-45 years (60%) and most patients belonged to skin types 3 and 4 (80%). Two female patients had a positive family history of vitiligo (10%) and two had hypothyroidism (10%). Disease duration was longer than 5 years for most patients (55%) and 85% of the patients had previous treatments (not within the past 3 months of study enrolment) (Table 1). The most common sites of lesions were the abdomen and lower back (15% each), followed by other sites as shown in figure 2.
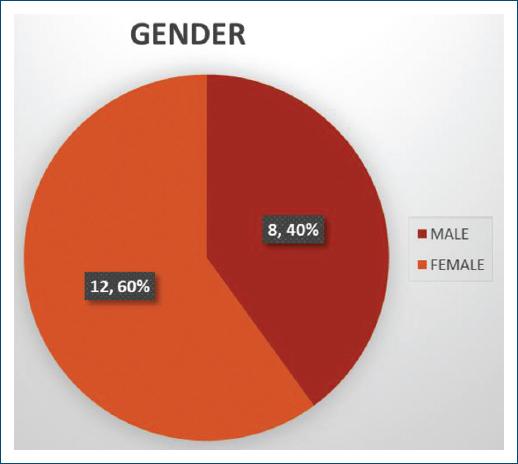
Figure 1 Gender-wise distribution of the patients enrolled in the study; 40% (8 out of 20) of patients enrolled were males, and 60% (12 out of 20) were females.
Table 1 Demographic details and brief history of the patients enrolled in the study
| Parameter | No. of patients | Percentage of patients |
|---|---|---|
| Age (in years) | ||
| 12-28 | 6 | 30 |
| 29-45 | 12 | 60 |
| 46-60 | 2 | 10 |
| Fitzpatrick skin type | ||
| 1 | 0 | 0 |
| 2 | 1 | 5 |
| 3 | 6 | 30 |
| 4 | 10 | 50 |
| 5 | 3 | 15 |
| 6 | 0 | 0 |
| Family history of vitiligo | ||
| Present | 2 | 10 |
| Absent | 18 | 90 |
| History of hypothyroidism | ||
| Present | 2 | 10 |
| Absent | 18 | 90 |
| Duration of disease (in years) | ||
| < 1 | 0 | 0 |
| 1-5 | 9 | 45 |
| > 5 | 11 | 55 |
| History of previous treatment (not within past 3 months of enrollment) | ||
| Present | 17 | 85 |
| Absent | 3 | 15 |
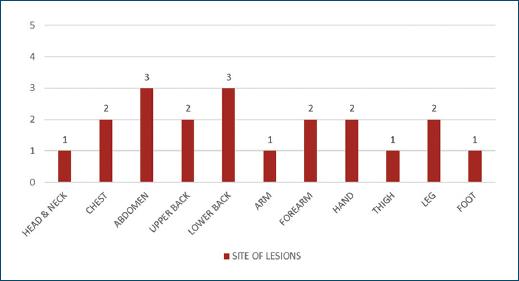
Figure 2 Distribution of patients according to the site of vitiliginous lesions; mucosal vitiligo was not included in the study (numerals indicate the number of patients).
The time taken for initiation of repigmentation was as early as 4 weeks after beginning the therapy, as observed in six patients (30%). The median time to the beginning of repigmentation was found to be 8 weeks. The most common type of repigmentation was perifollicular (Fig. 3A and B), followed by diffuse and marginal, with 65% of patients (13 out of 20) showing statistically significant repigmentation (p = 0.03), considered as good (51-75%, i.e., grade 3) or excellent (> 75%, i.e., grade 4) repigmentation (Table 2) (Fig. 4A and B). Lesser response (grade 1-2), that is, < 50% repigmentation was seen at acral and relatively less hairy sites.

Figure 3 A: perifollicular type of repigmentation seen in a 43-year-old female patient at 4 weeks after the initiation of treatment (site of lesion- right side of neck). B: perifollicular type of repigmentation seen in a 41-year-old male patient at 4 weeks after the initiation of treatment (site of lesion - left side of chest).
Table 2 Grades of repigmentation and gender-wise distribution at the end of 16 weeks of study (p = 0.03); percentage of patients showing good (51-75%) to excellent (> 75%) repigmentation as observed in the study - 65% (13 patients); p = 0.03
| Grade of repigmentation | Percentage of repigmentation | Male | Female | Total no. of patients (%) (n = 20) | p-value |
|---|---|---|---|---|---|
| Grade 4 (excellent response) | > 75% | 2 | 3 | 5 (25) | 0.03 |
| Grade 3 (good response) | 51-75% | 6 | 2 | 8 (40) | |
| Grade 2 (moderate response) | 26-50% | 0 | 5 | 5 (25) | |
| Grade 1 (minimal response) | 1-25% | 0 | 2 | 2 (10) | |
| Grade 0 (no response) | NIL | 0 | 0 | 0 |

Figure 4 A: grade 4 (> 75%) repigmentation observed in a 36-year-old female patient at the end of 16 weeks of study (site of lesion- right leg). B: grade 4 (> 75%) repigmentation observed in a 42-year-old female patient at the end of 16 weeks of study; hyperpigmentation was noted in the surrounding skin (site of lesion - lower back).
All patients experienced mild pain, redness, swelling, and slight burning sensation after the laser procedure but symptoms subsided after ice application or within a few hours after the treatment and were tolerable. Two patients also complained of a slight burning sensation after the 0.1% bFGF-related decapeptide application, but this was described as tolerable and subsided within a few minutes after the application. Similarly, one patient experienced mild itching, xerosis, and slight erythema post-NB-UVB exposure but the complaints were transient and resolved after application of an emollient.
Hyperpigmentation and therefore, change in skin type was observed in 11 (55%) patients (Fig. 4B). None of the patients reported any local infection, koebnerization, or increase in size of lesions. No adverse effects such as scarring, ulceration, telangiectasias, hypertrophic, or atrophic scars were noted.
No recurrence of lesions was observed at the end of follow-up period of 12 weeks in any of the patients.
Discussion
Vitiligo is a pigmentary skin disorder characterized by the absence of melanocytes in the epidermis, leading to the development of depigmented macules and patches on the body15. A variety of treatment options are available for vitiligo, including topical and systemic medications, phototherapy, laser therapy, and surgical interventions. While the topical treatments typically involve the use of corticosteroids, calcineurin inhibitors, bFGF-related decapeptide, vitamin D analogs, and ruxolitinib, there is the minimal response with topical therapy alone, thereby warranting the addition of systemic or combination therapy. Surgical therapy, on the other hand, is limited to segmental or localized stable vitiligo that is not involving a large body surface area16. Phototherapy is a commonly employed treatment modality and is effective for inducing repigmentation not only in early disease but also in disease of prolonged duration17. NB-UVB phototherapy, administered 2-3 times weekly with a wavelength of 311 nm, is widely utilized, as it helps in repigmentation by stimulating melanocyte activity, thus having more efficacy and relatively low risk of side effects compared to psoralen photochemotherapy which was previously used for management of vitiligo17,18. The addition of topical bFGF-related decapeptide could potentially enhance this effect, as bFGF is known for its role in promoting cell growth and differentiation by acting as a mitogen, thus, aiding melanocyte regeneration19. Shah et al. in their study have demonstrated that bFGF-related peptide (bFGFrP) exhibits synergistic effects when combined with other treatment modalities for vitiligo20. Similarly, fractionated CO2 acts by skin resurfacing, tissue shrinkage, activation, and migration of melanoblasts from the hair follicles and melanocytes from the skin surrounding the vitiliginous lesions21. Furthermore, it is known to stimulate Matrix metalloproteinase-2, thereby promoting migration of melanocytes from the adjacent skin as caused by NB-UVB and causes better penetration of topical drugs by creating micropores22,23. The efficacy of fractional CO2 laser therapy in treating refractory non-segmental vitiligo was demonstrated in a study conducted in 2014 where traditional treatments had been ineffective12. Therefore, fractional CO2 laser acts by facilitating penetration of the bFGFrP and improving melanocyte uptake, while also promoting skin remodeling.
In the present study, a novel combination of NB-UVB phototherapy with bFGF-related decapeptide 0.1% and fractional CO2 laser was used in patients of non-segmental, stable vitiligo which demonstrated early initiation of repigmentation (within 4 weeks) and the pattern of repigmentation most commonly observed was perifollicular. Moreover, the results obtained in the study were statistically significant (p = 0.03), which confirmed the efficacy of the combination in the management of vitiligo. The results obtained were similar to the study done in 2012 by Shin et al.24, which proved higher efficacy of the combination of fractional CO2 with NB-UVB as compared to NB-UVB alone. However, contrary to the results of > 50% repigmentation obtained in 10% of patients only, our study showed similar results in 65% of patients with the novel combination used. Similarly, Vachiramon et al.25, in 2016, found better results of the triple combination of fractional CO2 laser with NB-UVB phototherapy and 0.05% clobetasol propionate cream as compared to dual combination of NB-UVB and 0.05% clobetasol propionate cream, proving the efficacy of fractional CO2 laser in the treatment of vitiligo. Contrarily, the results obtained with the triple combination used in their study yielded > 50% repigmentation in 23.1% of patients only. Another study conducted in 2023 by Nayak et al.26 showed a better grade of repigmentation in vitiliginous patches when PUVA phototherapy was combined with bFGFrP as compared to PUVA monotherapy alone, thereby proving the synergistic effect of phototherapy with bFGFrP. However, while 61.8% of patients showed > 50% repigmentation with this combination, our study showed the same results in 65% of patients.
Lesions at the acral and glabrous sites, on the other hand, showed lesser response to treatment (< 50% repigmentation). This difference in results could be explained by the lack of stimulation or mobilization of melanoblasts from the outer root sheath of hair follicles surrounding the vitiliginous lesions at these regions, since the melanoblast activation and migration are essential processes for repigmentation of the lesions, as observed in previous studies21.
To the best of our knowledge, this combination used in the current study has not been studied before. This study proves the efficacy of the combination in the treatment of vitiliginous lesions without any major adverse effects and, hence, can be a safe potential future therapy for the management of stable, non-segmental vitiligo patients.
Conclusion
Although there are certain limitations such as the absence of a comparative group, lack of control area for measuring the efficacy of either modality alone, lesser duration of follow-up to monitor for the loss of achieved pigmentation, exclusion of mucosal vitiligo cases, and a relatively small sample size, the present study demonstrates significant results regarding the efficacy of this novel combination therapy. Combining NB-UVB phototherapy with bFGF-related decapeptide 0.1% and fractional CO2 laser treatment yielded better grades of repigmentation at a faster rate compared to the combinations of other modalities used previously. This approach offers a safe and effective treatment option, warranting further research to validate its efficacy and broader application in clinical practice.














