Introduction
Tungiasis is a parasitic skin infection caused by the female sand flea Tunga penetrans, when it comes into contact with the skin and penetrates it1. This parasitosis is endemic to tropical and subtropical areas, typically in underdeveloped countries2. This disease is known by various names across the globe: chigoe, jigger, sand flea, puce-chique, kuti, suthi pique, níguas, bicho do pé or pulga de bicho3. Although it is not present in Europe, it is possible to observe this pathology in tourists, especially those staying in more rural areas and in local accommodations4.
The following case has the purpose to illustrate a disease that is not so well known in the European medical community but that needs better recognition due to globalization, easy access to travel, and close relations with certain communities3,4.
Clinical case
A 21-year-old man, caucasian, living in Portugal, with no previous medical or surgical history, no medication, and no documented allergies, with an up-to-date vaccination plan, was observed in the acute illness consultation at his primary health-care center with three pruritic skin lesions on his toes beginning the previous week, with a foreign body sensation and discomfort when walking, but no pain or any other symptoms or previous injuries. The patient reported having spent 2 weeks on vacation in Brazil, in a rural area, having been barefoot on the beach and the land near his accommodation.
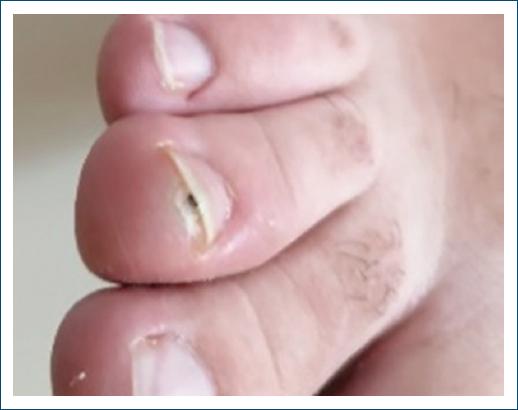
Inspection revealed three firms isolated 5 mm papules, bright yellow with a black central region, on the 1st and 4th toes of the left foot and the infra-ungual region of the 3rd toe of the right foot (Figs. 1-3). Lesions showed no signs of surrounding inflammation and no other lesions could be observed.
Based on the description of the lesions, symptoms, and recent trip to Brazil, the first diagnostic hypothesis was tungiasis. The patient was referred to the emergency department of the nearest hospital where the three parasites were extracted and the locae were debrided. Within 2 weeks, there was a complete recovery.
Discussion
Tungiasis is a parasitic disease endemic to tropical and subtropical areas, typically found in underdeveloped countries, particularly in sub-Saharan Africa, South America, and the Caribbean2,5. This parasitosis is more prevalent in more populated places, with poor sanitary and housing conditions and with reservoir animals present (rats, cats, cows, pigs, and dogs)6-8. The parasite is found in sandy soil and beach sand and is transmitted through direct contact.
The parasite begins its life cycle after hatching from an egg in the form of a larva that feeds on organic compounds in the environment. After growing, the larva pupates and becomes an adult flea. The adult male and female fleas feed intermittently on the blood of their hosts, but only the pregnant female flea is able to penetrate the host, which is essential for the parasite’s life cycle. The pregnant flea penetrates the skin through its cephalic portion, leaving the terminal portion in contact with the outside that allows the flea to breathe and expel feces and white eggs, and gives the skin lesions a black color in the center that contributes to the clinical identification. After 5-6 weeks, the flea dies and is expelled by the host after several weeks9,10.
Tungiasis differs in terms of epidemiology, clinical presentation, and complications between tourists and inhabitants of endemic regions: in tourists, the disease is typically benign and self-limited, whereas in endemic areas, the disease can be very disabling due to the longer exposure time and number of parasites2. In tourists, due to the penetration of isolated fleas, the disease usually presents as isolated papular or nodular lesions with white, gray, or yellowish color, surrounded by hyperkeratosis, and a small brown-to-black central opening, sometimes with eggs on the adjacent skin, corresponding to the posterior portions of the abdomen of the flea4,11. The lesions may be associated with itching, pain, skin desquamation, and foreign body sensation6,8. Typically, lesions occur on the feet (due to walking barefoot), typically on the toes, the interdigital region, and the infra-ungual region, but lesions may also be present on other parts of the body, such as the hands or back, if the person sleeps on the floor. In individuals living in endemic countries or in immunocompromised patients, lesions can be found in aggregate forms with up to 30 parasites in the same area, causing deformation of the adjacent skin, more often with hyperkeratosis, deformation of the extremities, bacterial over-infection, and gangrene1,2,4,7,9. In addition, other less common clinical presentations have been described, such as plantar wart-like lesions, crusted, bullous, pustular, and ulcerative lesions11.
The diagnosis of tungiasis is made clinically, based on the presence of typical lesions together with a corresponding travel history to an area where tungiasis is endemic11. Dermatoscopy has been shown to be helpful to aid the diagnosis of tungiasis, particularly in non-endemic regions4,6,11,12. The classical characteristics are a brown-to-black central pore, a white halo corresponding to the enlarged abdomen of the parasite, and a peripheral bluish-gray area corresponding to the parasite exoskeleton4. Confirmation of the diagnosis is made with microscopic analysis, which shows hyperkeratosis, parakeratosis, and acanthosis2,11. The flea is localized in the upper dermis, surrounded by a pseudo-cystic cavity. Eggs are also observed inside the flea. A perilesional, inflammatory infiltrate, is also present11.
The differential diagnosis of tungiasis may include viral warts, cutaneous myiasis, granuloma of foreign bodies, arthropod bites, ingrown foot nails, bacterial infections, pyogenic granuloma, malign tumors (melanoma and squamous cell carcinoma), and myxoid cysts3,4,5,6,9,11.
Treatment of choice is complete surgical excision of the parasite, with subsequent disinfection of the site2,4,9. Antibiotic therapy is not necessary unless there are signs of bacterial over-infection2,4. Vaccination status against tetanus should be checked and updated and prophylaxis may be necessary2,3,4,11. However, the surgical option is not recommended in severe infections with the presence of several parasites. There is still no topical or oral treatment with satisfactory results for tungiasis, but some studies report on the use of ivermectin and thiabendazole, especially topical2,9,10,11.
Prevention consists mainly of avoiding contact with contaminated soil, wearing closed shoes when in contact with soil and sand, and regular inspection of the feet for early identification of skin lesions4,10. In addition, some studies indicate the use of a plant-based repellent Zanzarin® (made up of coconut oil, jojoba oil, and aloe vera) to reduce the number of lesions2,9,10,13. Regular decontamination, implementation and improvement of sanitary measures, and the removal of parasite reservoir animals can reduce prevalence.
We present this case to emphasize the existence of this tropical disease, which is not so well known in the medical community in non-endemic countries14, but whose recognition is important, given the increase in globalization, tourism, and social migration phenomena.