Introduction
Sporotrichosis is a subcutaneous mycosis resulting from the traumatic inoculation of fungi belonging to the Sporothrix genus, prevalent in tropical climate countries in South America, Asia, and Africa, particularly in Colombia, Peru, Brazil, Venezuela, Mexico, Japan, India, and China1. Since 1997, an epidemic of this zoonotic disease has been observed in the state of Rio de Janeiro, primarily transmitted by felines, with a higher incidence in the capital and municipalities of Baixada Fluminense. In this epidemic scenario, children may become infected due to their interactions with animals in areas proximal to their residences. However, the involvement of infants is rarely described and may pose a significant clinical and epidemiological challenge. Late diagnosis contributes to the progression of cutaneous lesions and the consequent formation of esthetically undesirable scars2.
Clinical case
A 9-month-old male patient, born in Rio de Janeiro, and residing in Duque de Caxias, was observed due to lumps on the neck. The mother reported the appearance of two asymptomatic nodules with progressive growth for 1 month, located in the right cervical and pre-auricular regions. The patient also exhibited irritability, fever, and insufficient weight gain. He had previously been treated with multiple antibiotic regimens, including amoxicillin with clavulanate, azithromycin, ceftriaxone, and oxacillin, without clinical improvement.
The patient was born via normal delivery at term, with normal growth and development for his age. He was breastfeeding, with a complete vaccination schedule, no comorbidities or medication use, and the family history did not indicate anything noteworthy. In the social history, the patient had contact with an apparently healthy cat in the household, but this cat did not stay exclusively indoors.
On dermatological examination, two erythematous nodules were observed, with a soft consistency. The larger nodule was in the right pre-auricular region, and a smaller one was in the right cervical region (Fig. 1).
Considering the clinical context, the diagnostic hypotheses considered were cat scratch disease, suppurative lymphadenitis, lymphocutaneous sporotrichosis, and cutaneous tuberculosis.
Lesion ultrasound revealed reactive right cervical lymphadenopathy with central flow. Complete blood count, serologies for Bartonella henselae, and quintana, toxoplasmosis, and cytomegalovirus, were normal or negative as well as the 5 mm purified protein derivative test and a chest X-ray. Aspiration of the larger nodule revealed abundant yellowish fluid, which underwent culture for fungi, tuberculous, and non-tuberculous mycobacteria, as well as Gram stain and culture for common bacteria. Mycological examination revealed the growth of a membranous colony with a white color and a dark halo that on microscopy showed septate, branched, thin hyphae, giving rise to conidiophores that produced pyriform conidia arranged in a daisy pattern (Fig. 2). These laboratory findings, combined with the clinical presentation, indicated the diagnosis of lymphocutaneous sporotrichosis.
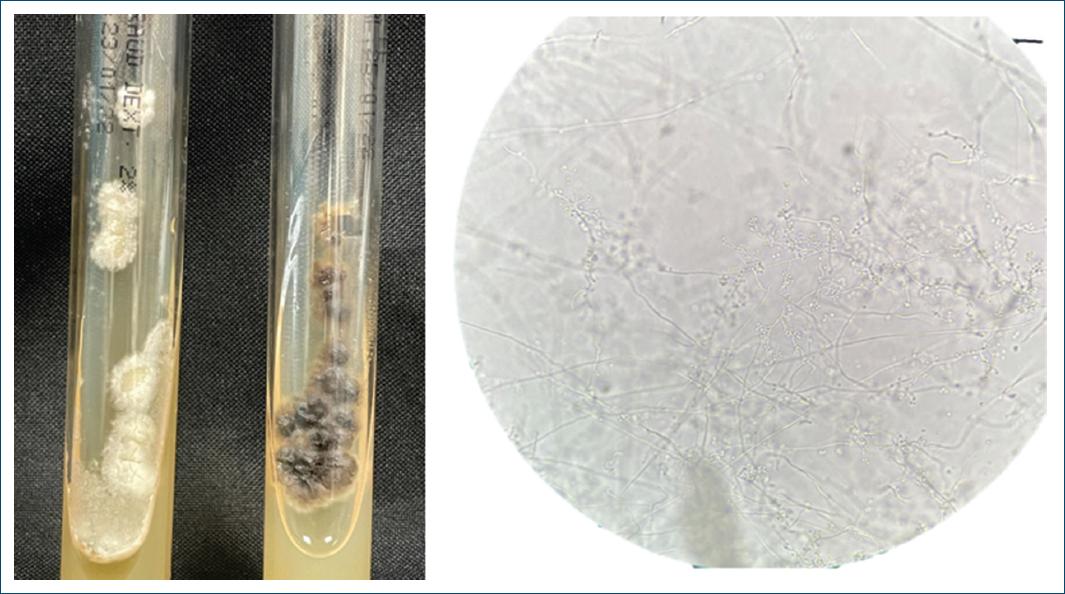
Figure 2 Mycological examination: macromorphology (figure on the left) reveals a membranous colony with a white color and a dark halo; micromorphology (figure on the right) reveals septate, branched, thin hyphae, from which conidiophores arise, giving rise to pyriform conidia arranged in a daisy-like pattern.
The patient was treated with oral itraconazole 10 mg/kg/day, with periodic reassessments initially at 2 weeks and monthly thereafter. The clinical lesions showed significant regression after the 1st month of treatment and nearly complete resolution by the end of the 2nd month of treatment (Fig. 3), with a total treatment duration of 4 months. A discreet hyperchromic scar remained at the site of the lesion.
Discussion
Sporotrichosis is a subacute and chronic fungal infection caused by species of the Sporothrix. genus. Notably, Sporothrix brasiliensis has been responsible for an epidemic in Rio de Janeiro, linked to feline zoonotic transmission3. Compulsory reporting in Rio de Janeiro since 2013 revealed a predominance in women (61%) and a higher incidence in individuals aged 40-594. The infection commonly results from traumatic inoculation, often through contact with contaminated soil or through scratches and bites from infected cats2,5.
Pediatric sporotrichosis is rare; primarily affects the skin of the face and limbs, particularly the hands, with lymphocutaneous involvement and the patient’s close contact with cats suggested a potential association1. The present case, in a 9-month-old patient with cervical and facial nodules, was diagnosed through mycological examination of the content of a nodule.
The literature review indicates that there are few cases of sporotrichosis in children under 1 year of age. Tlougan et al. reported, in 2009, a child residing in Texas who developed a facial lesion with confirmed Sporothrix etiology at just 3 weeks of age. This case represents the youngest patient documented in the literature6. A series of cases from the Chinese province of Jilin reported 15 patients under 10 months of age affected by the disease. All presented ulcerated lesions on the face, with no association with local trauma or contact with animals. In this series, the families of infants had the habit of using corn husks for cooking or heating. The isolation of S. schenckii from corn residues has been reported in India and Northeastern China7. Such reports indicate the variability of epidemiological profiles and disease transmission among countries. In this context, the case described in this study did not show a clear relationship with trauma before the development of lesions. However, close contact with cats is a crucial point for the potential association with this transmitting agent. Despite the patient hailing from an endemic area for sporotrichosis, he falls within an age group seldom described, classifying him as a relevant study subject. His clinical presentation, although documented, did not progress to ulceration, allowing for a wide range of possible diagnostic hypotheses for this age group8. Ultimately, access to appropriate laboratory tests enabled an accurate diagnosis and effective treatment, aiming to reduce morbidity and prevent the formation of unaesthetic scars.
















